Abstract
Purpose of Review
Pediatric endoscopic skull base surgery (ESBS) is a field of practice that has seen significant advancement and widespread adoption from its initial description less than two decades ago. This manuscript aims to review the development of the technique with particular attention to how our knowledge of the field has increased within the past 5 years.
Recent Findings
The understanding of the anatomic nuances in the pediatric endonasal corridor has grown, especially regarding the impact of sphenoid pneumatization on outcomes and the intercarotid distance at the sella. In addition, more robust data on outcomes has shown that ESBS is safe and effective in the pediatric population. In particular, the use of the nasoseptal flap has been more successful in younger patients than previously shown. Finally, studies have shown the minimal impact of ESBS on craniofacial development.
Summary
Pediatric ESBS is minimally invasive and safe and has good patient outcomes.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
London NR Jr, Rangel GG, Walz PC. The expanded endonasal approach in pediatric skull base surgery: a review. Laryngoscope Investig Otolaryngol. 2020;5(2):313–25.
Wu T, Chandy Z, Ference E, Lee JT. Endoscopic skull base surgery in the pediatric population. Curr Treat Options Allergy. 2021;8(3):274–84.
Wang EW, Zanation AM, Gardner PA, et al. ICAR: endoscopic skull‐base surgery. Paper presented at: Int Forum Allergy Rhinol. 2019.
Ali ZS, Henn RE, Adappa ND, Palmer JN, Lee JY, Storm PB. Pediatric endoscopic endonasal skull base surgery: the Children's Hospital of Philadelphia experience. J Neurol Surg Part B Skull Base. 2015;76(S01):A057.
Kassam A, Thomas AJ, Snyderman C, et al. Fully endoscopic expanded endonasal approach treating skull base lesions in pediatric patients. J Neurosurg Pediatr. 2007;106(2):75–86.
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part I. Crista galli to the sella turcica. Neurosurg Focus. 2005;19(1):1–12.
Kassam A, Snyderman CH, Mintz A, Gardner P, Carrau RL. Expanded endonasal approach: the rostrocaudal axis. Part II. Posterior clinoids to the foramen magnum. Neurosurg Focus. 2005;19(1):1–7.
Tatreau JR, Patel MR, Shah RN, et al. Anatomical considerations for endoscopic endonasal skull base surgery in pediatric patients. Laryngoscope. 2010;120(9):1730–7.
Banu MA, Rathman A, Patel KS, et al. Corridor-based endonasal endoscopic surgery for pediatric skull base pathology with detailed radioanatomic measurements. Operative Neurosurg. 2014;10(2):273–93.
Banu MA, Guerrero-Maldonado A, McCrea HJ, et al. Impact of skull base development on endonasal endoscopic surgical corridors. J Neurosurg Pediatr. 2014;13(2):155–69.
• Hamid O, El Fiky L, Hassan O, Kotb A, El Fiky S. Anatomic variations of the sphenoid sinus and their impact on trans-sphenoid pituitary surgery. Skull Base. 2008;18(01):009–15.
Kuan EC, Kaufman AC, Lerner D, et al. Lack of sphenoid pneumatization does not affect endoscopic endonasal pediatric skull base surgery outcomes. Laryngoscope. 2019;129(4):832–6.
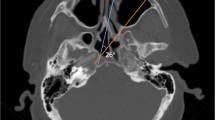
Li L, Carrau RL, Prevedello DM, et al. Intercarotid artery distance in the pediatric population: implications for endoscopic transsphenoidal approaches to the skull base. Int J Pediatr Otorhinolaryngol. 2021;140: 110520.
Shah RN, Surowitz JB, Patel MR, et al. Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope. 2009;119(6):1067–75.
Giovannetti F, Mussa F, Priore P, et al. Endoscopic endonasal skull base surgery in pediatric patients. A single center experience. J Cranio-Maxillofacial Surg. 2018;46(12):2017–2021.
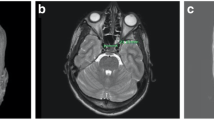
Purcell PL, Shinn JR, Otto RK, Davis GE, Parikh SR. Nasoseptal flap reconstruction of pediatric sellar defects: a radiographic feasibility study and case series. Otolaryngology-Head Neck Surg. 2015;152(4):746–51.
Madsen PJ, Buch VP, Douglas JE, et al. Endoscopic endonasal resection versus open surgery for pediatric craniopharyngioma: comparison of outcomes and complications. J Neurosurg Pediatr. 2019;24(3):236–45.
Drapeau A, Walz PC, Eide JG, et al. Pediatric craniopharyngioma. Childs Nerv Syst. 2019;35(11):2133–45.
Bogusz A, Müller HL. Childhood-onset craniopharyngioma: latest insights into pathology, diagnostics, treatment, and follow-up. Expert Rev Neurother. 2018;18(10):793–806.
Trifanescu R, Ansorge O, Wass JA, Grossman AB, Karavitaki N. Rathke’s cleft cysts. Clin Endocrinol. 2012;76(2):151–60.
Han SJ, Rolston JD, Jahangiri A, Aghi MK. Rathke’s cleft cysts: review of natural history and surgical outcomes. J Neurooncol. 2014;117(2):197–203.
Dhandapani S, Singh H, Negm HM, et al. Endonasal endoscopic reoperation for residual or recurrent craniopharyngiomas. J Neurosurg. 2017;126(2):418–30.
Low CM, Vigo V, Nunez M, Fernández-Miranda JC, Patel ZM. Anatomic considerations in endoscopic pituitary surgery. Otolaryngol Clin North Am. 2022;55(2):223–32.
McCrea HJ, George E, Settler A, Schwartz TH, Greenfield JP. Pediatric suprasellar tumors. J Child Neurol. 2016;31(12):1367–76.
Ali ZS, Lang S-S, Kamat AR, et al. Suprasellar pediatric craniopharyngioma resection via endonasal endoscopic approach. Childs Nerv Syst. 2013;29(11):2065–70.
Patel VS, Thamboo A, Quon J, et al. Outcomes after endoscopic endonasal resection of craniopharyngiomas in the pediatric population. World Neurosurg. 2017;108:6–14.
Alalade AF, Ogando-Rivas E, Boatey J, et al. Suprasellar and recurrent pediatric craniopharyngiomas: expanding indications for the extended endoscopic transsphenoidal approach. J Neurosurg Pediatr. 2018;21(1):72–80.
Beer-Furlan A, Todeschini AB, Carrau RL, Prevedello DM. Endoscopic endonasal approach for posterior fossa tumors. Skull Base Surg Posterior Fossa. Springer. 2018:75–86.
Rajappa P, Margetis K, Sigounas D, Anand V, Schwartz TH, Greenfield JP. Endoscopic endonasal transclival approach to a ventral pontine pediatric ependymoma: case report. J Neurosurg Pediatr. 2013;12(5):465–8.
Sanborn MR, Kramarz MJ, Storm PB, Adappa ND, Palmer JN, Lee JY. Endoscopic, endonasal, transclival resection of a pontine cavernoma: case report. Operative Neurosurg. 2012;71(suppl_1):onsE198-onsE203.
Maggiore G, Lazio MS, Gallo O. Treatment of pediatric esthesioneuroblastoma with smell preservation. Auris Nasus Larynx. 2018;45(5):1107–12.
Sigler AC, D’Anza B, Lobo BC, Woodard TD, Recinos PF, Sindwani R. Endoscopic skull base reconstruction: an evolution of materials and methods. Otolaryngol Clin North Am. 2017;50(3):643–53.
Harvey RJ, Parmar P, Sacks R, Zanation AM. Endoscopic skull base reconstruction of large dural defects: a systematic review of published evidence. Laryngoscope. 2012;122(2):452–9.
•• Shah N, Deopujari C, Bommakanti V. The reconstruction of skull base defects in infants using pedicled nasoseptal flap—a review of four cases. Childs Nerv Syst. 2019;35(11):2157–62. This study reports the successful use of the nasoseptal flap in four infants.
Kuan EC, Carey RM, Palmer JN, Adappa ND. Special considerations for nasoseptal flap use in children. Oper Tech Otolaryngol Head Neck Surg. 2019;30(1):78–84.
Stapleton AL, Tyler-Kabara EC, Gardner PA, Snyderman CH, Wang EW. Risk factors for cerebrospinal fluid leak in pediatric patients undergoing endoscopic endonasal skull base surgery. Int J Pediatr Otorhinolaryngol. 2017;93:163–6.
• Ghosh A, Hatten K, Learned KO, et al. Pediatric nasoseptal flap reconstruction for suprasellar approaches. Laryngoscope. 2015;125(11):2451–6. The paper reports success in the use of the nasoseptal flap for suprasellar defects in patients < 10 years old.
Lopez EM, Farzal Z, Dean KM, et al. Outcomes in pediatric endoscopic skull base surgery: a systematic review. J Neurol Surg Part B Skull Base. 2021. (AAM).
Yamada S, Fukuhara N, Yamaguchi-Okada M, et al. Therapeutic outcomes of transsphenoidal surgery in pediatric patients with craniopharyngiomas: a single-center study. J Neurosurg Pediatr. 2018;21(6):549–62.
Zwagerman NT, Wang EW, Shin SS, et al. Does lumbar drainage reduce postoperative cerebrospinal fluid leak after endoscopic endonasal skull base surgery? A prospective, randomized controlled trial. J Neurosurg. 2018;131(4):1172–8.
Van Peteghem A, Clement P. Influence of extensive functional endoscopic sinus surgery (FESS) on facial growth in children with cystic fibrosis: comparison of 10 cephalometric parameters of the midface for three study groups. Int J Pediatr Otorhinolaryngol. 2006;70(8):1407–13.
Bothwell MR, Piccirillo JF, Lusk RP, Ridenour BD. Long-term outcome of facial growth after functional endoscopic sinus surgery. Otolaryngology-Head Neck Surg. 2002;126(6):628–34.
Senior B, Wirtschafter A, Mai C, Becker C, Belenky W. Quantitative impact of pediatric sinus surgery on facial growth. Laryngoscope. 2000;110(11):1866–70.
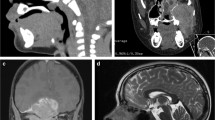
•• Chen W, Gardner PA, Branstetter BF, et al. Long-term impact of pediatric endoscopic endonasal skull base surgery on midface growth. J Neurosurg Pediatr. 2019;23(4):523–30. This paper shows no impact on the growth of the facial skeleton if ESBS is performed prior to cranial suture fusion.
•• Parasher AK, Lerner DK, Glicksman JT, et al. The impact of expanded endonasal skull base surgery on midfacial growth in pediatric patients. Laryngoscope. 2020;130(2):338–42. This paper showed no difference in craniofacial measurements between children who had undergone ESBS versus open surgery.
Ben-Ari O, Wengier A, Ringel B, et al. Nasoseptal flap for skull base reconstruction in children. J Neurol Surg Part B: Skull Base. 2018;79(01):037–41.
Funding
Internal departmental funding was utilized without commercial sponsorship or support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Pediatric Otolaryngology: Challenges in Pediatric Otolaryngology
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Low, C.M., Hwang, P.H. Endoscopic Skull Base Surgery in Children. Curr Otorhinolaryngol Rep 10, 440–446 (2022). https://doi.org/10.1007/s40136-022-00432-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-022-00432-3