Abstract
Purpose of Review
The aim of this review is to present the current literature on pathophysiology, evaluation, and management of laryngeal dystonia.
Recent Findings
Recent evidence suggests loss of cortical inhibition, and sensory dysfunction plays an important role in the pathophysiology of laryngeal dystonia. New treatments addressing these changes include electrical stimulation for neuromodulation of the larynx, vibrotactile therapy, and sodium oxybate. Preliminary investigations are promising and these may impact the future of care for laryngeal dystonia patients.
Summary
The current literature emphasizes a new understanding of the pathophysiology of laryngeal dystonia which has led to investigation of novel therapies.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Blitzer A, Brin MF, Stewart CF. Botulinum toxin management of spasmodic dysphonia (laryngeal dystonia): a 12-year experience in more than 900 patients. Laryngoscope. 1998;108:1435–41.
Blitzer A, Brin MF, Fahn S, Lovelace RE. Localized injections of botulinum toxin for the treatment of focal laryngeal dystonia (spastic dysphonia). Laryngoscope. 1988;98:193–7.
Kaye R, Blitzer A. Chemodenervation of the larynx. Toxins (Basel). 2017;9(11):356. https://doi.org/10.3390/toxins9110356.
Murry T. Spasmodic dysphonia: let’s look at that again. J Voice. 2014;28:694–9.
Butler AG, Duffey PO, Hawthorne MR, Barnes MP. An epidemiologic survey of dystonia within the entire population of northeast England over the past nine years. Adv Neurol. 2004;94:95–9.
Hintze JM, Ludlow CL, Bansberg SF, Adler CH, Lott DG. Spasmodic dysphonia: a review. Part 1: pathogenic factors. Otolaryngol Head Neck Surg. 2017;157:551–7.
Schweinfurth JM, Billante M, Courey MS. Risk factors and demographics in patients with spasmodic dysphonia. Laryngoscope. 2002;112:220–3.
Robe E, Brumlik J, Moore P. A study of spastic dysphonia. Neurologic and electroencephalographic abnormalities. Laryngoscope. 1960;70:219–45.
Dedo HH. Recurrent laryngeal nerve section for spastic dysphonia. Ann Otol Rhinol Laryngol. 1976;85:451–9.
• Lungu C, Ozelius L, Standaert D, Hallett M, Sieber BA, Swanson-Fisher C, et al. Defining research priorities in dystonia. Neurology. 2020;94:526–37 A recent review from pioneering dystonia scientists discussing the future direction of research.
Battistella G, Termsarasab P, Ramdhani RA, Fuertinger S, Simonyan K. Isolated focal dystonia as a disorder of large-scale functional networks. Cereb Cortex. Oxford University Press. 2015;27:bhv313.
•• Bianchi S, Battistella G, Huddleston H, Scharf R, Fleysher L, Rumbach AF, et al. Phenotype-and genotype-specific structural alterations in spasmodic dysphonia. Mov Disord. Wiley Online Library; 2017;32:560–8. It is one of the first studies to show association of structual changes in the CNS to LD.
Bianchi S, Fuertinger S, Huddleston H, Frucht SJ, Simonyan K. Functional and structural neural bases of task specificity in isolated focal dystonia. Mov Disord. 2019;34:555–63.
Delmaire C, Vidailhet M, Wassermann D, Descoteaux M, Valabregue R, Bourdain F, et al. Diffusion abnormalities in the primary sensorimotor pathways in writer’s cramp. Arch Neurol. 2009;66:502–8.
Delmaire C, Vidailhet M, Elbaz A, Bourdain F, Bleton JP, Sangla S, et al. Structural abnormalities in the cerebellum and sensorimotor circuit in writer’s cramp. Neurology. 2007;69:376–80.
Garraux G, Bauer A, Hanakawa T, Wu T, Kansaku K, Hallett M. Changes in brain anatomy in focal hand dystonia. Ann Neurol. 2004;55:736–9.
Granert O, Peller M, Gaser C, Groppa S, Hallett M, Knutzen A, et al. Manual activity shapes structure and function in contralateral human motor hand area. Neuroimage. 2011;54:32–41.
Ramdhani RA, Kumar V, Velickovic M, Frucht SJ, Tagliati M, Simonyan K. What’s special about task in dystonia? A voxel-based morphometry and diffusion weighted imaging study. Mov Disord. 2014;29:1141–50.
Simonyan K, Tovar-Moll F, Ostuni J, Hallett M, Kalasinsky VF, Lewin-Smith MR, et al. Focal white matter changes in spasmodic dysphonia: a combined diffusion tensor imaging and neuropathological study. Brain. 2008;131:447–59.
Simonyan K, Ludlow CL. Abnormal structure-function relationship in spasmodic dysphonia. Cereb Cortex. 2012;22:417–25.
Kirke DN, Battistella G, Kumar V, Rubien-Thomas E, Choy M, Rumbach A, et al. Neural correlates of dystonic tremor: a multimodal study of voice tremor in spasmodic dysphonia. Brain Imaging Behav. 2017;11:166–75.
•• Blitzer A, Brin MF, Simonyan K, Ozelius LJ, Frucht SJ. Phenomenology, genetics, and CNS network abnormalities in laryngeal dystonia: a 30-year experience. Laryngoscope. Wiley Online Library; 2018;128:S1–9. Comprehensive review of clinic and pathophysiological research studies from a cohort of 1400 LD patients.
•• Hanekamp S, Simonyan K. The large-scale structural connectome of task-specific focal dystonia. Hum Brain Mapp. 2020. https://doi.org/10.1002/hbm.25012Recommended paper for better understanding abnormal structural and functional neural network aspect of LD pathophsiology.
Fuertinger S, Horwitz B, Simonyan K. The functional connectome of speech control. PLoS Biol. 2015;13:1–31.
Bonini F, Burle B, Lieǵeois-Chauvel C, Reǵis J, Chauvel P, Vidal F. Action monitoring and medial frontal cortex: leading role of supplementary motor area. Science. 2014;343:888–91.
Swann NC, Cai W, Conner CR, Pieters TA, Claffey MP, George JS, et al. Roles for the pre-supplementary motor area and the right inferior frontal gyrus in stopping action: electrophysiological responses and functional and structural connectivity. Neuroimage. 2012;59:2860–70.
Chen M, Summers RLS, Prudente CN, Goding GS, Samargia-Grivette S, Ludlow CL, et al. Transcranial magnetic stimulation and functional magnet resonance imaging evaluation of adductor spasmodic dysphonia during phonation. Brain Stimul Elsevier BV. 2020;13:908–15.
Samargia S, Schmidt R, Kimberley TJ. Cortical silent period reveals differences between adductor spasmodic dysphonia and muscle tension dysphonia. Neurorehabil Neural Repair. 2016;30:221–32.
Pirio RS. Enhanced dorsal premotor-motor inhibition in cervical dystonia. Clin Neurophysiol. 2015;126:1387–91.
Kirke DN, Frucht SJ, Simonyan K. Alcohol responsiveness in laryngeal dystonia: a survey study. J Neurol. 2015;262:1548–56.
Konczak J, Aman JE, Chen YW, Li KY, Watson PJ. Impaired limb proprioception in adults with spasmodic dysphonia. J Voice. 2015;29:777.e17–23.
Yoneda Y, Rome S, Sagar HJ, Grünewald RA. Abnormal perception of the tonic vibration reflex in idiopathic focal dystonia. Eur J Neurol. 2000;7:529–33.
Grünewald RA, Yoneda Y, Shipman JM, Sagar HJ. Idiopathic focal dystonia: a disorder of muscle spindle afferent processing. Brain. 1997;120:2179–85.
Conte A, Rocchi L, Ferrazzano G, Leodori G, Bologna M, Li Voti P, et al. Primary somatosensory cortical plasticity and tactile temporal discrimination in focal hand dystonia. Clin Neurophysiol. 2014;125:537–43.
Termsarasab P, Ramdhani RA, Battistella G, Rubien-Thomas E, Choy M, Farwell IM, et al. Neural correlates of abnormal sensory discrimination in laryngeal dystonia. NeuroImage Clin The Authors. 2016;10:18–26.
Simonyan K, Ludlow CL. Abnormal activation of the primary somatosensory cortex in spasmodic dysphonia: an fMRI study. Cereb Cortex. 2010;20:2749–59.
Ali SO, Thomassen M, Schulz GM, Hosey LA, Varga M, Ludlow CL, et al. Alterations in CNS activity induced by botulinum toxin treatment in spasmodic dysphonia: an H215O PET study. J Speech Lang Hear Res. 2006;49:1127–46.
Rosenkranz K, Butler K, Williamon A, Rothwell JC. Regaining motor control in musician’s dystonia by restoring sensorimotor organization. J Neurosci. 2009;29:14627–36.
Tinazzi M, Zarattini S, Valeriani M, Stanzani C, Moretto G, Smania N, et al. Effects of transcutaneous electrical nerve stimulation on motor cortex excitability in writer’s cramp: neurophysiological and clinical correlations. Mov Disord. 2006;21:1908–13.
Trompetto C, Currà A, Buccolieri A, Suppa A, Abbruzzese G, Berardelli A. Botulinum toxin changes intrafusal feedback in dystonia: a study with the tonic vibration reflex. Mov Disord. 2006;21:777–82.
• Rosales RL, Arimura K, Takenaga S, Osame M. Extrafusal and intrafusal muscle effects in experimental botulinum toxin-A injection. Muscle Nerve. 1996;19:488–96 This paper suggests BTX mitigates the symptoms of dystonia via treatment of the intrafusal fibers of the muscle spindle.
Leis AA, Dimitrijevic MR, Delapasse JS, Sharkey PC. Modification of cervical dystonia by selective sensory stimulation. J Neurol Sci. 1992;110:79–89.
Xiao J, Zhao Y, Bastian RW, Perlmutter JS, Racette BA, Tabbal SD, et al. Novel THAP1 sequence variants in primary dystonia. Neurology. Ovid Technologies (Wolters Kluwer Health). 2010;74:229–38.
Fuchs T, Saunders-Pullman R, Masuho I, San Luciano M, Raymond D, Factor S, et al. Mutations in GNAL cause primary torsion dystonia. Nat Genet Nature Publishing Group. 2013;45:88–92.
Putzel GG, Fuchs T, Battistella G, Rubien-Thomas E, Frucht SJ, Blitzer A, et al. GNAL mutation in isolated laryngeal dystonia. Mov Disord Wiley Online Library. 2016;31:750–5.
Clarimon J, Asgeirsson H, Singleton A, Jakobsson F, Hjaltason H, Hardy J, et al. Torsin A haplotype predisposes to idiopathic dystonia. Ann Neurol Wiley. 2005;57:765–7.
Hague S, Klaffke S, Clarimon J, Hemmer B, Singleton A, Kupsch A, et al. Lack of association with TorsinA haplotype in German patients with sporadic dystonia. Neurology. Ovid Technologies (Wolters Kluwer Health). 2006;66:951–2.
Sharma N, Franco RA, Kuster JK, Mitchell AA, Fuchs T, Saunders-Pullman R, et al. Genetic evidence for an association of the TOR1A locus with segmental/focal dystonia. Mov Disord Wiley. 2010;25:2183–7.
Blitzer A, Lovelace RE, Brin MF, Fahn S, Fink ME. Electromyographic findings in focal laryngeal dystonia (spastic dysphonia). Ann Otol Rhinol Laryngol. 1985;94:591–4.
Novakovic D, Waters HH, D’Elia JB, Blitzer A. Botulinum toxin treatment of adductor spasmodic dysphonia: longitudinal functional outcomes. Laryngoscope. 2011;121:606–12.
Aronson AE, De Santo LW. Adductor spastic dysphonia: three years after recurrent laryngeal nerve resection. Laryngoscope. 1983;93:1–8.
Berke GS, Blackwell KE, Gerratt BR, Verneil A, Jackson KS, Sercarz JA. Selective laryngeal adductor denervation-reinnervation: a new surgical treatment for adductor spasmodic dysphonia. Ann Otol Rhinol Laryngol. 1999;108:227–31.
Isshiki N, Tsuji DH, Yamamoto Y, Iizuka Y. Midline lateralization thyroplasty for adductor spasmodic dysphonia. Ann Otol Rhinol Laryngol. 2000;109:187–93.
Matsushima K, Isshiki N, Tanabe M, Yoshizaki N, Otsu K, Fukuo A, et al. Operative procedure of anterior commissure for type II thyroplasty. J Voice Elsevier BV. 2018;32:374–80.
Su CY, Chuang HC, Tsai SS, Chiu JF. Transoral approach to laser thyroarytenoid myoneurectomy for treatment of adductor spasmodic dysphonia: short-term results. Ann Otol Rhinol Laryngol. 2007;116:11–8.
• Schuering JHC, Heijnen BJ, Sjögren E V, Langeveld APM. Adductor spasmodic dysphonia: Botulinum toxin a injections or laser thyroarytenoid myoneurectomy? A comparison from the patient perspective. Laryngoscope. Wiley; 2020;130:741–6. First comparative study between the gold standard BTX therapy and surgergical intervention for ADLD.
Koufman JA. Management of abductor spasmodic dysphonia by endoscopic partial posterior cricoarytenoid (PCA) myectomy. Phonoscope-San Diego. Singular Publishing Group Inc; 1999;2:159–66.
Dewan K, Berke GS. Bilateral vocal fold medialization: a treatment for abductor spasmodic dysphonia. J Voice. Elsevier BV. 2019;33:45–8.
Ludlow CL, Naunton RF, Terada S, Anderson BJ. Successful treatment of selected cases of abductor spasmodic dysphonia using botulinum toxin injection. Otolaryngol Head Neck Surg. 1991;104:849–55.
Eller RL, Miller M, Weinstein J, Sataloff RT. The innervation of the posterior cricoarytenoid muscle: exploring clinical possibilities. J Voice. 2009;23:229–34.
Benito DA, Ferster APO, Sataloff RT. Bilateral posterior cricoarytenoid myoneurectomy for abductor spasmodic dysphonia. J Voice. Elsevier BV. 2020;34:127–9.
Shaw GY, Sechtem PR, Rideout B. Posterior cricoarytenoid myoplasty with medialization thyroplasty in the management of refractory abductor spasmodic dysphonia. Ann Otol Rhinol Laryngol. 2003;112:303–6.
Postma GN, Blalock PD, Koufman JA. Bilateral medialization laryngoplasty. Laryngoscope. 1998;108:1429–34.
Bari AA, Thum J, Babayan D, Lozano AM. Current and expected advances in deep brain stimulation for movement disorders. Prog Neurol Surg. 2018;33:222–9.
Dougherty DD. Deep brain stimulation. Psychiatr Clin North Am Elsevier BV. 2018;41:385–94.
Lyons MK, Boucher OK, Evidente VGH. Spasmodic dysphonia and thalamic deep brain stimulation: long-term observations, possible neurophysiologic mechanism and comparison of unilateral versus bilateral stimulation. J Neurol Neurophysiol. 2010;1:106. https://doi.org/10.4172/2155-9562.1000106.
NCT02558634 @ clinicaltrials.gov [Internet]. Available from: https://clinicaltrials.gov/ct2/show/NCT02558634. Accessed 5/10/2020.
•• Rumbach AF, Blitzer A, Frucht SJ, Simonyan K. An open-label study of sodium oxybate in spasmodic dysphonia. Laryngoscope. 2017;127:1402–7 First trial of a promising therapeutic for alcohol responsive LD patients.
NCT03292458 @ clinicaltrials.gov [Internet]. Available from: https://clinicaltrials.gov/ct2/show/NCT03292458. Accessed 5/10/2020.
Cakmur R, Donmez B, Uzunel F, Aydin H, Kesken S. Evidence of widespread impairment of motor cortical inhibition in focal dystonia: a transcranial magnetic stimulation study in patients with blepharospasm and cervical dystonia. Adv Neurol. 2004;94:37–44.
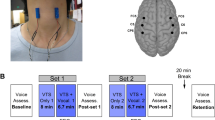
•• Khosravani S, Mahnan A, Yeh IL, Aman JE, Watson PJ, Zhang Y, et al. Laryngeal vibration as a non-invasive neuromodulation therapy for spasmodic dysphonia. Sci Rep. 2019;9:17955 This study shows non-invasive laryngeal vibrotactile stimulation improving symptoms of ADLD by positive changes in the somatosensory region of the motor cortex.
NCT03746509 @ clinicaltrials.gov [Internet]. Available from: https://clinicaltrials.gov/ct2/show/NCT03746509. Accessed 5/10/2020.
Tinazzi M, Farina S, Bhatia K, Fiaschi A, Moretto G, Bertolasi L, et al. TENS for the treatment of writer’s cramp dystonia: a randomized, placebo-controlled study. Neurology. Ovid Technologies (Wolters Kluwer Health). 2005;64:1946–8.
•• Pitman MJ. Treatment of spasmodic dysphonia with a neuromodulating electrical implant. Laryngoscope. Wiley; 2014;124:2537–43. First study showing a positive effect of neuromodulation with electrical stimulation on laryngeal dystonia.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Necati Enver declares no conflict of interest.
Michael J. Pitman has a royalty and patent interest with MedEl in the use of electrical stimulation for laryngeal and focal dystonia.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical collection on Neurolaryngology
Rights and permissions
About this article
Cite this article
Enver, N., Pitman, M.J. What Is New in Laryngeal Dystonia: Review of Novel Findings of Pathophysiology and Novel Treatment Options. Curr Otorhinolaryngol Rep 8, 209–215 (2020). https://doi.org/10.1007/s40136-020-00301-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40136-020-00301-x