Abstract
Purpose of the Review
Conditions typically prevalent in adults such as hypertension, kidney stones, osteoporosis, and chronic kidney disease are increasing among adolescents and young adults (AYA). The purpose of this review is to describe the association of these conditions to a high salt diet among pediatric patients.
Recent Findings
We present animal, human, and 23Na MRI evidence associated with the negative impact of high dietary salt in children. Special focus is placed on novel 23Na MRI imaging which reveals the important concept of a third compartment for sodium storage in soft tissue. Finally, we make recommendations on who should not be on a low salt diet.
Summary
A high salt intake predisposes children and AYA to considerable morbidity. We exhort the reader to engage in advocacy efforts to curve the incidence and prevalence of high salt-related life-limiting conditions.
Similar content being viewed by others
Introduction
Life expectancy has been declining steadily in North America over the past 5 years [1], even before the COVID-19 pandemic, owing to poor diet and lifestyle choices. Of the modifiable factors, limiting dietary salt is important. Prehistoric man was characteristically exposed to very low levels of dietary sodium—typically with 20 times higher potassium than sodium in their urine (sodium/potassium ratio 0.02); life expectancy reached 70 years and modern day non-communicable diseases such as heart attacks and strokes were almost absent [2]. In stark contrast, we can find urinary sodium/potassium ratios of 10 (healthy < 2.4) in youth with kidney stones [3]. Diseases that used to be described in adults such as hypertension, kidney stones, type II diabetes, metabolic syndrome, and even cardiovascular disease are increasing among adolescents and young adults (AYA) [4,5,6,7]—all potentially linked to increased sodium exposure.
Socioeconomic status is inversely correlated with salt intake as low-cost foods contain great amounts of salt in general [8]. In fact, up to 75% of the salt intake is due to processed food [9]. The authors of this review are particularly concerned about the impact of high dietary salt in children of families with low socioeconomical means, who cannot afford the cost of some low sodium foods. The gap between rich and poor is increasing in developed countries, and in view of the detrimental impact of high salt diet in childhood on longevity and all-cause mortality, we need a call to action. The food industry uses the cheapest preservatives to increase the shelf life of products and profits. Therefore, access to low salt food becomes a matter of social injustice and legislature changes are required to limit salt in processed food, similar to what has been done in Finland, Argentina, and South Africa [10]. The purpose of this review is to summarize the recent literature on salt intake and morbidity in children and AYA, since comprehensive legislation to lower salt in processed food is an easily modifiable factor to improve longevity and reduce salt related morbidity and mortality.
The Impact of a High Salt Diet the Unborn
It has long been known that maternal diet during pregnancy can have a profound impact on the offspring. Too much salt is already a problem since salt worsens the edema of the face, hands, legs, ankles, and feet commonly experienced by the mother during pregnancy. Moreover, high maternal salt intake affects the fetal renal renin angiotensin aldosterone system (RAAS). According to the Dietary Guidelines for Americans established by the Department of Agriculture and the Department of Health and Human Services, the recommendation is up to about a teaspoon of salt a day—that is, 6 g of salt, or approximately 2300 mg of sodium. However, most people living in North America consume more than 3500 mg of sodium per day, including pregnant women [11, 12].
The developmental origins of health and disease theory indicates that many adult-onset diseases originate in the earliest stages of life. The developing kidney is particularly vulnerable to adverse in utero conditions, leading to morphological and functional changes and potentially suboptimal nephron endowment. Malnutrition is the common factor related to hypertension and kidney disease; however, a variety of nutritional insults can cause renal programming including high sucrose and fructose consumption, protein and calorie restriction, and high fat diet [13]. High salt diet during pregnancy needs to be added to this list, at least suggested by data derived from experimental study of female Wistar rats [13, 14]. Oxidative stress, an imbalance between reactive oxygen/nitrogen species and antioxidant systems, plays a pathogenic role in the developmental programming of kidney disease [15]. There is increasing evidence that activation of the RAAS increases oxidative stress. This is important since there is a finite nephron endowment that develops until 36 weeks of gestational age [16].
Another possible explanation is the induction of expression of renal angiotensin II due to a high salt diet [14]. Animal studies suggest that intra-uterine exposure to high salt is associated with activation of the local RAAS (which persisted after birth), a risk factor for the development of kidney or cardiovascular diseases. When pregnant ewes were fed a high salt diet for 2 months during mid to late gestation, their offspring were noted to have high urinary sodium with lower urine volume compared to those exposed to a low salt diet [17]. Those with a high salt diet had persistently elevated serum sodium up until 15 and 90 days of age. Furthermore, ewes with a high salt diet had a greater mRNA expression relating to angiotensin, angiotensin 1 (AT1), angiotensin 2 (AT2), angiotensin converting enzyme (ACE) levels, and ACE:ACE2 ratio [17]. In another set of experiments, vascular dysfunction has been demonstrated in adult offspring of AT1 receptor antibody positive pregnant rats exposed to a high salt diet in utero [18]. Prenatal exposure to AT2 has been shown to cause reduced nephron endowment and kidney impairment in male rat offspring [19]. The results from the latter study suggest that prenatally increased AT2 promoted infiltration of immune cells in the kidney and subsequent oxidative stress, inducing damage of the renal glomerular and tubular system, entailing negative consequences on the cardiovascular system [19].
Taken together, current evidence strongly suggests that the RAAS plays a significant role on renal programming. As shown here, animal data suggest that a high salt diet during pregnancy contributes to this and may be responsible for hypertension and CKD later in life. This concept warrants further research.
Hypertension and Salt
Determination of total body sodium content in vivo has been challenging till the recent development of sodium-23 magnetic resonance imaging (23Na MRI), which allows the non-invasive quantification of tissue sodium content [20]. We have applied a relatively standard approach to sodium imaging to directly study tissue accumulation in children. Briefly, a multinuclear-capable 3.0-Tesla MRI scanner (Discovery MR750 3.0 T, General Electric Healthcare, Milwaukee, WI, USA) is used to acquire 23Na spin-density images of the lower leg, for which subjects were positioned in the magnet bore in the supine position, with the thickest part of their right or left calf muscle at the center of a custom-made 23Na birdcage radiofrequency coil. Calibration vials with 10, 20, 30, and 40 mmol/L of saline are placed in the RF coil over the subjects’ shins. A single-slice 23Na MRI image is obtained with a radial k-space acquisition pulse sequence known as “Density-Adapted 2D Projection Reconstruction,” with the following parameters: slice-selective radiofrequency pulse; flip angle 90°; repetition time/echo time: 100/1.2 ms; total acquisition time: 30 min; number of signals averages, 100; slice thickness, 30 mm and isotropic field of view/resolution, 18/0.3 cm2. During the same imaging session, additional axial 1H MR images were acquired using a standard “Spoiled Gradient-Recalled Echo” pulse sequence to identify and delineate the relevant anatomical structures.
Healthy children (n = 17) had a median skin sodium concentration of 13.4 (3.3 interquartile range [IQR]), whereas 19 healthy adults had a median skin sodium concentration of 18.7 (6.2 IQR). Similarly, muscleSoleus sodium concentrations were 18.6(1.6 IQR) in children and 22.2 (4.3 IQR) in adults (unpublished results). Sodium concentrations correlated with age. CKD and dialysis patients had much higher sodium concentrations compared to normal controls (in adult patients), and skin sodium concentration was higher in a small cohort (10 subjects) of children with CKD c.f. with age matched controls.
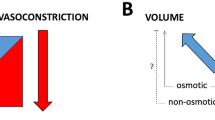
While there is ample evidence for sodium accumulation going hand in hand with fluid retention to maintain the environmental effective osmotic pressure gradient (tonicity) [21, 22], experimental evidence has also shown that the skin is a reservoir for water-free sodium in mammals including humans [23, 24]. However, similar studies in children and adolescents remain scant. Sodium accumulation has been experimentally associated with endothelial dysfunction and vascular stiffening [25, 26]. Tissue sodium has been shown to be mobilized by loop diuretic therapy [27], hemodialysis [28], and the novel sodium glucose cotransporter 2 (SGLT2) inhibitors [29•]. SGLT2 inhibitors are a class of drug widely used in the management of type 2 diabetes mellitus that work by inhibiting the reabsorption of glucose in the proximal convoluted tubule [30]. This class of medications inhibits the coupled reabsorption of sodium and glucose, thereby increasing urinary sodium and glucose wasting. The natriuretic effects coupled with tissue sodium depletion may be one of the main reasons why these medications have such a profound effect on cardiovascular complications [31].
However, in children and adolescents, the importance of a low sodium diet is poorly elucidated. During the first 3 days of life, preterm infants have a lower concentration ability than full-term babies. Tubular immaturity is associated with greater natriuresis until about 3 weeks of life [32]. While a positive sodium balance promotes growth in childhood, studies that correlate a high salt diet and hypertension during childhood are difficult to conduct. These studies rely on food diaries, 24-h urinary Na, or spot urinary Na/creatinine ratio, making absolute Na intake unreliable. Aparicio et al. showed in a study of 205 school children that the sodium intake of hypertensive children was higher than that of normotensive children [33]. Owing to obesity and high salt intake, high blood pressure is increasingly becoming prevalent among children and youth. A meta-analysis of 10 controlled trials [34] assessed the effect of reducing dietary salt in hypertension (n = 966 patients, ages 8–16 years); and a reduction of salt by 42%, reduced systolic, and diastolic blood pressure [34]. In the same publication, three trials of infants and children ages 8 weeks to 6 months who had a 56% reduction in dietary salt also had a reduction in systolic blood pressure [34].
Roth and coworkers used 23Na MRI in 32 obese adolescents aged 13–17 years of which 11 had arterial hypertension. Median skeletal muscle Na + content in hypertensive obese (11.95 mmol/L [interquartile range 11.62–13.66]) was significantly lower than in normotensive obese (13.63 mmol/L [12.97–17.64]; p = 0.043) or controls (15.37 mmol/L [14.12–16.08]; p = 0.012). No significant differences were found between normotensive obese individuals and control subjects [35]. Unfortunately, the question whether tissue sodium concentration is associated with the development of hypertension in children and adolescents is understudied. However, mechanistic computer modeling would suggest that large vessel stiffness owing to sodium retention resulting in peripheral resistance could be the prime source of arterial hypertension even in a newborn with acute kidney injury [36].
Urinary Stone Disease and Salt
Traditionally, urinary stone disease (USD) has been a disease of older males. In children and AYA, USD was rare and mostly related to rare genetic conditions such as renal tubular acidosis, cystinuria, or hyperoxaluria [3]. However, we are witnessing an unprecedented increase of USD in AYA, especially among females [4, 37,38,39,40]. Based on the data in one of our own centers, the number of patients with USD quadrupled among 10 to 17-year-olds studied from 2015 to 2019, tripling among young adults (Fig. 1). Most of these patients did not have any inherited causes for USD identified. Hypercalciuria and insufficient citrate with a urinary calcium/citrate ratio > 1 are most often found in these patients [41].
USD is a critical public health concern as it is associated with osteoporosis, the development of CKD, and shortened life-expectancy [42, 43]. A large proportion of USD patients already developed decreased bone mineral density [44, 45]. Interestingly, this was more prevalent in adolescent males [46], even though females tend to have lower bone mineral density z-scores than males. A major reason for USD is the steady increase in dietary sodium intake in Western countries (typically > 3500 mg/day, whereas the World Health Organization (WHO) recommends < 2000 mg/day) [11, 12, 47, 48]. The sodium intake in the USA for children aged 6–11 years of age increased from 200 mg/day in the 1970s to 3000 mg/day in the 2000s [49]. There is a direct relationship between urinary sodium excretion and urinary calcium wasting [50]. This makes limiting the salt intake the easiest step to reduce the lithogenic risk [51].
Unfortunately, socioeconomic status is inversely correlated with salt intake, as low-cost foods are highly salted in general [8], with up to 75% of the salt intake derived from ingestion of processed food [9]. On this basis, the recognized correlation between socioeconomic status and USD [52] is unsurprising. The American Urological Association recommends limitation of sodium intake [53], but this may be impossible for low-income families who have to rely on inexpensive, processed food.
Osteoporosis and Salt
Osteoporosis is a major public health problem, affecting 16% of men and 29.9% of women older than 50 years of age in the USA [54]. A high sodium, high protein, and high salt diet is one of the most important factors driving osteoporotic disease progression [55]. While the etiology of osteoporosis is multifactorial, high salt intake is a major risk factor for the development of osteoporosis [56]. The relationship between osteoporosis and a high salt diet is the same as for USD; high salt intake requires the kidneys to excrete more salt, which inhibits the calcium reabsorption in the distal tubule [57]. Since the calcium homeostasis requires that serum calcium remains very tightly controlled, salt-induced calcium wasting leads to the need of mobilization of bone-derived calcium aggravated by the fact that many children and adolescents in North America are vitamin D deficient [48, 58]. Epidemiological studies suggest that osteoporosis is affecting younger and younger people [59]. Rendina et al. highlight the linkage between USD and osteoporosis and propose to call the combination of both a new syndrome [59]. Furthermore, children and youth with neuromuscular disorders, chronic diseases, and low motor competence are particularly at risk for the future development of osteoporosis [60].
Adolescents accrue bone mineral density only until early adulthood [61]; there is evidence to suggest that peak bone mass and later fracture risk are influenced by the pattern of growth in childhood and by nutritional exposures in utero, in infancy, and during childhood and adolescence.
Unfortunately, the typical developed country diets of children and youth consist of high protein intake (i.e., large acid load), high salt intake (i.e. calcium wasting), and low fruit and vegetable intake—which serve as an important source of buffers. Large population-based studies of bone mineral density in adolescents are lacking but based on the findings in USD patients and the continuously rising salt intake in our population, we may face a future increase of osteoporosis constituting a further major public health problem.
Sodium-23 Magnetic Resonance Imaging and Chronic Kidney Disease
The relationship between salt intake, blood pressure, cardiovascular, and kidney diseases has been the subject of a considerable volume of research [62]. Traditional clinical estimates of sodium status include serum sodium and 24-h urine sodium excretion but are poor estimates of total body sodium. Recently, 23Na MRI became available as a non-invasive tool to estimate sodium accumulation in soft tissues such as skin and muscles in the extremities [63, 64]. Importantly, this imaging technique does not distinguish water-bound from water-free sodium, and increased tissue sodium concentrations are mainly a function of extracellular volume expansion [65]. Skin and muscle sodium concentrations increase with age likely due to a reduction of cellular mass in favor of interstitial expansion [22, 63]. Larger skin sodium concentrations have also been observed in male sex compared with females and may be relevant in the pathophysiology of essential hypertension in humans [63].
Preliminary observations from our group point out that children may have the lowest tissue sodium concentration [66•], as opposed to adult dialysis patients where tissue sodium concentrations are largest [67, 68]. Though intuitively increased dietary sodium intake should be associated with increased tissue sodium levels, clinical evidence in this respect is scarce; Bracconier et al. have shown that in healthy individuals, higher salt intake is associated with higher sodium concentrations in muscle tissue and sweat [69•]. Elevated sodium content has been demonstrated in several pathological states in adults, suggesting a potential role of sodium accumulation as a mediator of outcomes: primary hyperaldosteronism [20], type 2 diabetes mellitus [70], acute heart failure [27], CKD, and kidney failure [71].
In our own current work, in the pediatric population, we observed that the sodium status differs between kidney disease etiologies—likely reflecting variable kidney sodium handling for different disease states. Glomerular diseases causing nephrotic syndrome are associated with primary sodium reabsorption and increased total body sodium [72] and lead to larger sodium accumulation, whereas some tubular diseases such as idiopathic Fanconi syndrome are associated with kidney sodium wasting and result in substantial tissue sodium depletion compared with healthy age and sex-matched controls [66•]. As a proof-of-concept, we represent 23Na MRI results of a 14-year-old hemodialysis patient (primary etiology of focal and segmental glomerulosclerosis) showing dramatic skin and muscle sodium accumulation, as compared to a healthy 14-year-old (Fig. 2).
23Na MRI of the leg in a 14-year-old healthy female (A) and a 14-year-old female patient with end-stage CKD (B). Images show a substantially increased whole leg sodium concentration ([Na+]) (A 15.9 vs B 36.2 mmol/L, Z-score + 12.2) skin [Na+] (A 10.5 vs B 30.4 mmol/L, Z-score + 7.0), and triceps surae muscle [Na+] (A 19.5 vs B 38.2 mmol/L, Z-score + 11.0). Na+ measurement was possible by linear trend analysis as detailed in [71], using three to four calibration vials containing increasing concentrations of NaCl solution (from left to right in A 40, 20, 10 mmol/L, and in B 40, 30, 20, 10 mmol/L). Tissue [Na+] is displayed as heat map, with greater signal intensity proportional to tissue [Na+]
The Problem with the Food Industry
A fundamental problem remains in the refusal of the food industry to voluntarily reduce the salt in the food. Salt is an effective and inexpensive food preservative, thereby increasing product shelf life, simplifying logistics, and maximizing profits. Despite the fact that the WHO declared a war on salt and made a reduction of sodium intake below 2000 mg/day a high priority (endorsed by all WHO members), only nine countries have any legislation about how much salt can be added to the food through industry and restaurants. Of these, six only pertain to bread which accounts for 26% of the daily salt intake mainly as result of how much of this relatively low salt-containing foodstuff is typically consumed. Only Finland, South Africa, and Argentina have comprehensive salt laws [10].
Who Should Not Be on a Low Salt Diet?
It is very clear that some children and AYA with tubular diseases are salt wasters. For instance, there is no place for sodium restriction in patients with Fanconi syndrome [66•]. Another example are patients with KCNJ16 mutations resulting in a novel tubulopathy with salt wasting [73]. Renal salt wasting may result from cystinosis, Dent disease, disorders of paracellular claudin-10b, and Kir4.1 potassium-channel deficiency [74]. We recently described profound salt wasting in a patient with compound heterozygous Bartter syndrome (KCNJ1 gene, a frameshift deletion, p.Glu334Glyfs*35, and a missense variant, p. Pro110Leu) [75]. Obviously, these patients must not be on a low salt diet. 23Na MRI studies in these patients remain scant. It has been shown repeatedly that serum sodium and urinary 24-h sodium excretion are not sufficient to diagnose sodium wasting or sodium retention. 23Na MRI forms a potent, non-invasive tool to determine tissue sodium content and may help to guide dietary and medication interventions for hypertension, heart failure, osteoporosis, USD, and other non-communicable disorders.
Conclusions
This review highlights the relationship between high salt intake and chronic life-limiting conditions such as hypertension, USD, osteoporosis, and CKD in children and AYA as well as the importance of sodium accumulation in the body, measured by 23Na MRI of muscle and skin. The high salt diet in Western societies may be the easiest modifiable factor to curb the growing prevalence of these non-communicable diseases. Obviously, salt wasters must be identified and supplemented accordingly. We exhort the reader to engage in advocacy efforts to curb the incidence and reduce the prevalence of high salt-related life-limiting conditions.
Abbreviations
- AYA:
-
Adolescents and young adults
- CKD:
-
Chronic kidney disease
- CAKUT:
-
Congenital anomalies of the kidneys and urinary tract
- eGFR:
-
Estimated glomerular filtration rate
- MRI:
-
Magnetic resonance imaging
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Venkataramani AS, O’Brien R, Tsai AC. Declining life expectancy in the United States: the need for social policy as health policy. JAMA J Am Med Assoc. 2021;325(7):621–2. https://doi.org/10.1001/jama.2020.26339.
Palmer BF, Clegg DJ. Achieving the benefits of a high-potassium, paleolithic diet, without the toxicity. Mayo Clin Proc. 2016;91(4):496–508. https://doi.org/10.1016/j.mayocp.2016.01.012.
Rodriguez Cuellar CI, Wang PZT, Freundlich M, Filler G. Educational review: role of the pediatric nephrologists in the work-up and management of kidney stones. Pediatr Nephrol. 2020;35(3):383–97. https://doi.org/10.1007/s00467-018-4179-9.
Sharma AP, Filler G. Epidemiology of pediatric urolithiasis. Indian J Urol. 2010;26(4):516–22. https://doi.org/10.4103/0970-1591.74450.
Battistoni A, Canichella F, Pignatelli G, Ferrucci A, Tocci G, Volpe M. Hypertension in young people: epidemiology, diagnostic assessment and therapeutic approach. High Blood Press Cardiovasc Prev. 2015;22(4):381–8. https://doi.org/10.1007/s40292-015-0114-3.
Lascar N, Brown J, Pattison H, Barnett AH, Bailey CJ, Bellary S. Type 2 diabetes in adolescents and young adults. Lancet Diabetes Endocrinol. 2018;6(1):69–80. https://doi.org/10.1016/S2213-8587(17)30186-9.
Chen W, Srinivasan SR, Berenson GS. Path analysis of metabolic syndrome components in black versus white children, adolescents, and adults: the Bogalusa Heart Study. Ann Epidemiol. 2008;18(2):85–91. https://doi.org/10.1016/j.annepidem.2007.07.090.
Ji C, Kandala NB, Cappuccio FP. Spatial variation of salt intake in Britain and association with socioeconomic status. BMJ Open. 2013;3(1). https://doi.org/10.1136/bmjopen-2012-002246.
James WP, Ralph A, Sanchez-Castillo CP. The dominance of salt in manufactured food in the sodium intake of affluent societies. Lancet. 1987;1(8530):426–9. https://doi.org/10.1016/s0140-6736(87)90127-9.
Filler G. Chapter 1: current salt legislation in developed countries. In: Filler G: AsSALTed Victoria: FriesenPress; 2020. 2020.
Barberio AM, Sumar N, Trieu K, Lorenzetti DL, Tarasuk V, Webster J, et al. Population-level interventions in government jurisdictions for dietary sodium reduction: a Cochrane Review. Int J Epidemiol. 2017;46(5):1551–2405. https://doi.org/10.1093/ije/dyw361.
Fischer PW, Vigneault M, Huang R, Arvaniti K, Roach P. Sodium food sources in the Canadian diet. Appl Physiol Nutr Metab. 2009;34(5):884–92. https://doi.org/10.1139/H09-077.
Hsu CN, Tain YL. Targeting the renin-angiotensin-aldosterone system to prevent hypertension and kidney disease of developmental origins. Int J Mol Sci. 2021;22(5). https://doi.org/10.3390/ijms22052298.
da Silva AA, de Noronha IL, de Oliveira IB, Malheiros DM, Heimann JC. Renin-angiotensin system function and blood pressure in adult rats after perinatal salt overload. Nutr Metab Cardiovasc Dis. 2003;13(3):133–9. https://doi.org/10.1016/s0939-4753(03)80172-2.
Hsu CN, Tain YL. Developmental origins of kidney disease: why oxidative stress matters? Antioxidants (Basel). 2020;10(1). https://doi.org/10.3390/antiox10010033.
Filler G, Bhayana V, Schott C, Diaz-Gonzalez de Ferris ME. How should we assess renal function in neonates and infants? Acta Paediatr. 2020. https://doi.org/10.1111/apa.15557.
Mao C, Liu R, Bo L, Chen N, Li S, Xia S, et al. High-salt diets during pregnancy affected fetal and offspring renal renin-angiotensin system. J Endocrinol. 2013;218(1):61–73. https://doi.org/10.1530/JOE-13-0139.
Zhang X, Zhang SL, Xiong HY, Du YH, Quan L, Yang J, et al. Vascular dysfunction in the offspring of AT1 receptor antibody-positive pregnant rats during high-salt diet. Sheng Li Xue Bao. 2011;63(2):149–54.
Svitok P, Okuliarova M, Varga I, Zeman M. Renal impairment induced by prenatal exposure to angiotensin II in male rat offspring. Exp Biol Med (Maywood). 2019;244(11):923–31. https://doi.org/10.1177/1535370219851110.
Kopp C, Linz P, Wachsmuth L, Dahlmann A, Horbach T, Schofl C, et al. (23)Na magnetic resonance imaging of tissue sodium. Hypertension. 2012;59(1):167–72. https://doi.org/10.1161/HYPERTENSIONAHA.111.183517.
Bhave G, Neilson EG. Body fluid dynamics: back to the future. J Am Soc Nephrol. 2011;22(12):2166–81. https://doi.org/10.1681/ASN.2011080865.
Rossitto G, Mary S, Chen JY, Boder P, Chew KS, Neves KB, et al. Tissue sodium excess is not hypertonic and reflects extracellular volume expansion. Nat Commun. 2020;11(1):4222. https://doi.org/10.1038/s41467-020-17820-2.
Titze J, Lang R, Ilies C, Schwind KH, Kirsch KA, Dietsch P, et al. Osmotically inactive skin Na+ storage in rats. Am J Physiol Renal Physiol. 2003;285(6):F1108–17. https://doi.org/10.1152/ajprenal.00200.2003.
Linz P, Santoro D, Renz W, Rieger J, Ruehle A, Ruff J, et al. Skin sodium measured with (2)(3)Na MRI at 7. 0 T. NMR Biomed. 2015;28(1):54–62. https://doi.org/10.1002/nbm.3224.
Machnik A, Neuhofer W, Jantsch J, Dahlmann A, Tammela T, Machura K, et al. Macrophages regulate salt-dependent volume and blood pressure by a vascular endothelial growth factor-C-dependent buffering mechanism. Nat Med. 2009;15(5):545–52. https://doi.org/10.1038/nm.1960.
Oberleithner H, Riethmuller C, Schillers H, MacGregor GA, de Wardener HE, Hausberg M. Plasma sodium stiffens vascular endothelium and reduces nitric oxide release. Proc Natl Acad Sci U S A. 2007;104(41):16281–6. https://doi.org/10.1073/pnas.0707791104.
Hammon M, Grossmann S, Linz P, Kopp C, Dahlmann A, Garlichs C, et al. 23Na magnetic resonance imaging of the lower leg of acute heart failure patients during diuretic treatment. PLoS ONE. 2015;10(10):e0141336. https://doi.org/10.1371/journal.pone.0141336.
Dahlmann A, Dorfelt K, Eicher F, Linz P, Kopp C, Mossinger I, et al. Magnetic resonance-determined sodium removal from tissue stores in hemodialysis patients. Kidney Int. 2015;87(2):434–41. https://doi.org/10.1038/ki.2014.269.
• Karg MV, Bosch A, Kannenkeril D, Striepe K, Ott C, Schneider MP, et al. SGLT-2-inhibition with dapagliflozin reduces tissue sodium content: a randomised controlled trial. Cardiovasc Diabetol. 2018;17(1):5. https://doi.org/10.1186/s12933-017-0654-z. (Inhibition of the sodium glucose cotransporter 2 can lead to a significant reduction, thereby providing a potent tool to reduce the cardiovascular risk.)
Ojha U, Reyes L, Eyenga F, Oumbe D, Watkowska J, Saint-Jacques H. Diabetes, heart failure and beyond: elucidating the cardioprotective mechanisms of sodium glucose cotransporter 2 (SGLT2) inhibitors. Am J Cardiovasc Drugs. 2021. https://doi.org/10.1007/s40256-021-00486-6.
Zanchi A, Burnier M, Muller ME, Ghajarzadeh-Wurzner A, Maillard M, Loncle N, et al. Acute and chronic effects of SGLT2 inhibitor empagliflozin on renal oxygenation and blood pressure control in nondiabetic normotensive subjects: a randomized, placebo-controlled trial. J Am Heart Assoc. 2020;9(13):e016173. https://doi.org/10.1161/JAHA.119.016173.
Herin P, Aperia A. Neonatal kidney, fluids, and electrolytes. Curr Opin Pediatr. 1994;6(2):154–7. https://doi.org/10.1097/00008480-199404000-00005.
Aparicio A, Rodriguez-Rodriguez E, Cuadrado-Soto E, Navia B, Lopez-Sobaler AM, Ortega RM. Estimation of salt intake assessed by urinary excretion of sodium over 24 h in Spanish subjects aged 7–11 years. Eur J Nutr. 2017;56(1):171–8. https://doi.org/10.1007/s00394-015-1067-y.
He FJ, MacGregor GA. Importance of salt in determining blood pressure in children: meta-analysis of controlled trials. Hypertension. 2006;48(5):861–9. https://doi.org/10.1161/01.HYP.0000245672.27270.4a.
Roth S, Marko L, Birukov A, Hennemuth A, Kuhnen P, Jones A et al. Tissue Sodium Content and Arterial Hypertension in Obese Adolescents. J Clin Med. 2019;8(12). https://doi.org/10.3390/jcm8122036.
Altamirano-Diaz L, Kassay AD, Serajelahi B, McIntyre CW, Filler G, Kharche SR. Arterial hypertension and unusual ascending aortic dilatation in a neonate with acute kidney injury: mechanistic computer modeling. Front Physiol. 2019;10:1391. https://doi.org/10.3389/fphys.2019.01391.
Ziemba JB, Matlaga BR. Epidemiology and economics of nephrolithiasis. Investig Clin Urol. 2017;58(5):299–306. https://doi.org/10.4111/icu.2017.58.5.299.
Issler N, Dufek S, Kleta R, Bockenhauer D, Smeulders N, Van’t Hoff W. Epidemiology of paediatric renal stone disease: a 22-year single centre experience in the UK. BMC nephrology. 2017;18(1):136. https://doi.org/10.1186/s12882-017-0505-x.
Edvardsson VO, Ingvarsdottir SE, Palsson R, Indridason OS. Incidence of kidney stone disease in Icelandic children and adolescents from 1985 to 2013: results of a nationwide study. Pediatr Nephrol. 2018;33(8):1375–84. https://doi.org/10.1007/s00467-018-3947-x.
Kusumi K, Becknell B, Schwaderer A. Trends in pediatric urolithiasis: patient characteristics, associated diagnoses, and financial burden. Pediatr Nephrol. 2015;30(5):805–10. https://doi.org/10.1007/s00467-014-3012-3.
Lee M, Rodriguez Cuellar CI, Nagra R, Wang ZTP, Bhayana V, Filler G. Does the urinary calcium/citrate ratio add to the diagnostic workup of children at risk of kidney stones? A cross-sectional study. J Child Sci. 2019;9:e1–6.
Dhondup T, Kittanamongkolchai W, Vaughan LE, Mehta RA, Chhina JK, Enders FT, et al. Risk of ESRD and mortality in kidney and bladder stone formers. Am J Kidney Dis. 2018;72(6):790–7. https://doi.org/10.1053/j.ajkd.2018.06.012.
Chuang TF, Hung HC, Li SF, Lee MW, Pai JY, Hung CT. Risk of chronic kidney disease in patients with kidney stones-a nationwide cohort study. BMC Nephrol. 2020;21(1):292. https://doi.org/10.1186/s12882-020-01950-2.
Sakhaee K, Maalouf NM, Poindexter J, Adams-Huet B, Moe OW. Relationship between urinary calcium and bone mineral density in patients with calcium nephrolithiasis. J Urol. 2017;197(6):1472–7. https://doi.org/10.1016/j.juro.2017.01.002.
Sakhaee K, Maalouf NM, Kumar R, Pasch A, Moe OW. Nephrolithiasis-associated bone disease: pathogenesis and treatment options. Kidney Int. 2011;79(4):393–403. https://doi.org/10.1038/ki.2010.473.
Kusumi K, Schwaderer AL, Clark C, Budge K, Hussein N, Raina R, et al. Bone mineral density in adolescent urinary stone formers: is sex important? Urolithiasis. 2020;48(4):329–35. https://doi.org/10.1007/s00240-020-01183-w.
Choi SE, Brandeau ML, Basu S. Expansion of the national salt reduction initiative: a mathematical model of benefits and risks of population-level sodium reduction. Med Decis Making. 2016;36(1):72–85. https://doi.org/10.1177/0272989X15583846.
Rodriguez Cuellar CI, Wang PZT, Freundlich M, Filler G. Educational review: role of the pediatric nephrologists in the work-up and management of kidney stones. Pediatr Nephrol. 2019. https://doi.org/10.1007/s00467-018-4179-9.
Filler G. Chapter 2: kidney stones and salt. In: Filler G: AsSALTed Victoria: FriesenPress; 2020. 2020.
Osorio AV, Alon US. The relationship between urinary calcium, sodium, and potassium excretion and the role of potassium in treating idiopathic hypercalciuria. Pediatrics. 1997;100(4):675–81. https://doi.org/10.1542/peds.100.4.675.
Afsar B, Kiremit MC, Sag AA, Tarim K, Acar O, Esen T, et al. The role of sodium intake in nephrolithiasis: epidemiology, pathogenesis, and future directions. Eur J Intern Med. 2016;35:16–9. https://doi.org/10.1016/j.ejim.2016.07.001.
Tang J, Mettler P, McFann K, Chonchol M. The association of prevalent kidney stone disease with mortality in US adults: the National Health and Nutrition Examination Survey III, 1988–1994. Am J Nephrol. 2013;37(5):501–6. https://doi.org/10.1159/000350691.
Pearle MS, Goldfarb DS, Assimos DG, Curhan G, Denu-Ciocca CJ, Matlaga BR, et al. Medical management of kidney stones: AUA guideline. J Urol. 2014;192(2):316–24. https://doi.org/10.1016/j.juro.2014.05.006.
Wright NC, Saag KG, Dawson-Hughes B, Khosla S, Siris ES. The impact of the new National Bone Health Alliance (NBHA) diagnostic criteria on the prevalence of osteoporosis in the USA. Osteoporos Int. 2017;28(4):1225–32. https://doi.org/10.1007/s00198-016-3865-3.
Davis JA, Mohebbi M, Collier F, Loughman A, Shivappa N, Hebert JR, et al. Diet quality and a traditional dietary pattern predict lean mass in Australian women: Longitudinal data from the Geelong Osteoporosis Study. Prev Med Rep. 2021;21:101316. https://doi.org/10.1016/j.pmedr.2021.101316.
Fatahi S, Namazi N, Larijani B, Azadbakht L. The association of dietary and urinary sodium with bone mineral density and risk of osteoporosis: a systematic review and meta-analysis. J Am Coll Nutr. 2018;37(6):522–32. https://doi.org/10.1080/07315724.2018.1431161.
Sellmeyer DE, Schloetter M, Sebastian A. Potassium citrate prevents increased urine calcium excretion and bone resorption induced by a high sodium chloride diet. J Clin Endocrinol Metab. 2002;87(5):2008–12. https://doi.org/10.1210/jcem.87.5.8470.
Herrick KA, Storandt RJ, Afful J, Pfeiffer CM, Schleicher RL, Gahche JJ, et al. Vitamin D status in the United States, 2011–2014. Am J Clin Nutr. 2019;110(1):150–7. https://doi.org/10.1093/ajcn/nqz037.
Rendina D, De Filippo G, Iannuzzo G, Abate V, Strazzullo P, Falchetti A. Idiopathic osteoporosis and nephrolithiasis: two sides of the same coin? Int J Mol Sci. 2020;21(21). https://doi.org/10.3390/ijms21218183.
Jenkins M, Hart NH, Nimphius S, Chivers P, Rantalainen T, Rothacker KM, et al. Characterisation of peripheral bone mineral density in youth at risk of secondary osteoporosis - a preliminary insight. J Musculoskelet Neuronal Interact. 2020;20(1):27–52.
Zemel B. Bone mineral accretion and its relationship to growth, sexual maturation and body composition during childhood and adolescence. World Rev Nutr Diet. 2013;106:39–45. https://doi.org/10.1159/000342601.
Farquhar WB, Edwards DG, Jurkovitz CT, Weintraub WS. Dietary sodium and health: more than just blood pressure. J Am Coll Cardiol. 2015;65(10):1042–50. https://doi.org/10.1016/j.jacc.2014.12.039.
Kopp C, Linz P, Dahlmann A, Hammon M, Jantsch J, Muller DN, et al. 23Na magnetic resonance imaging-determined tissue sodium in healthy subjects and hypertensive patients. Hypertension. 2013;61(3):635–40. https://doi.org/10.1161/HYPERTENSIONAHA.111.00566.
Kopp C, Linz P, Maier C, Wabel P, Hammon M, Nagel AM, et al. Elevated tissue sodium deposition in patients with type 2 diabetes on hemodialysis detected by (23)Na magnetic resonance imaging. Kidney Int. 2018;93(5):1191–7. https://doi.org/10.1016/j.kint.2017.11.021.
Rossitto G, Touyz RM, Petrie MC, Delles C. Much Ado about N... atrium: modelling tissue sodium as a highly sensitive marker of subclinical and localized oedema. Clin Sci (Lond). 2018;132(24):2609–13. https://doi.org/10.1042/CS20180575.
• Filler G, Geda R, Salerno FR, Zhang YC, Ferris M, McIntyre C. Management of polyuria in idiopathic Fanconi syndrome. Pediatr Nephrol. 2021. (Some patients are salt wasters and must not be sodium restricted, for instance, patients with Fanconi syndrome, Bartter syndrome, or renal tubular acidosis.)
Lemoine S, Salerno FR, Akbari A, McIntyre CW. Influence of dialysate sodium prescription on skin and muscle sodium concentration. Am J Kidney Dis. 2021;78(1):156–9. https://doi.org/10.1053/j.ajkd.2020.11.025.
Sahinoz M, Tintara S, Deger SM, Alsouqi A, Crescenzi RL, Mambungu C, et al. Tissue sodium stores in peritoneal dialysis and hemodialysis patients determined by 23-sodium magnetic resonance imaging. Nephrol Dial Transplant. 2020. https://doi.org/10.1093/ndt/gfaa350.
• Braconnier P, Milani B, Loncle N, Lourenco JM, Brito W, Delacoste J, et al. Short-term changes in dietary sodium intake influence sweat sodium concentration and muscle sodium content in healthy individuals. J Hypertens. 2020;38(1):159–66. https://doi.org/10.1097/HJH.0000000000002234. (This report of 38 healthy persons clearly demonstrates the impact of a high salt intake on muscle and sweat sodium concentrations, demonstrating that muscle and sweat play a role in regulating sodium balance in humans.)
Kannenkeril D, Karg MV, Bosch A, Ott C, Linz P, Nagel AM, et al. Tissue sodium content in patients with type 2 diabetes mellitus. J Diabetes Complications. 2019;33(7):485–9. https://doi.org/10.1016/j.jdiacomp.2019.04.006.
Qirjazi E, Salerno FR, Akbari A, Hur L, Penny J, Scholl T, et al. Tissue sodium concentrations in chronic kidney disease and dialysis patients by lower leg sodium-23 magnetic resonance imaging. Nephrol Dial Transplant. 2020. https://doi.org/10.1093/ndt/gfaa036.
Svenningsen P, Bistrup C, Friis UG, Bertog M, Haerteis S, Krueger B, et al. Plasmin in nephrotic urine activates the epithelial sodium channel. J Am Soc Nephrol. 2009;20(2):299–310. https://doi.org/10.1681/ASN.2008040364.
Schlingmann KP, Renigunta A, Hoorn EJ, Forst AL, Renigunta V, Atanasov V, et al. Defects in KCNJ16 cause a novel tubulopathy with hypokalemia, salt wasting, disturbed acid-base homeostasis, and sensorineural deafness. J Am Soc Nephrol. 2021;32(6):1498–512. https://doi.org/10.1681/ASN.2020111587.
Bamgbola OF, Ahmed Y. Differential diagnosis of perinatal Bartter, Bartter and Gitelman syndromes. Clin Kidney J. 2021;14(1):36–48. https://doi.org/10.1093/ckj/sfaa172.
Verma S, Chanchlani R, Siu VM, Filler G. Transient hyponatremia of prematurity caused by mild Bartter syndrome type II: a case report. BMC Pediatr. 2020;20(1):311. https://doi.org/10.1186/s12887-020-02214-6.
Acknowledgements
We thank our patients and their parents/caregivers, for participating in research projects to help optimize the care of children, adolescents, and young adults with kidney disease. We thank our families for the patience that was required to prepare this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Renal
Rights and permissions
About this article
Cite this article
Filler, G., Salerno, F., McIntyre, C.W. et al. Animal, Human, and 23Na MRI Imaging Evidence for the Negative Impact of High Dietary Salt in Children. Curr Pediatr Rep 9, 110–117 (2021). https://doi.org/10.1007/s40124-021-00249-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-021-00249-6