Abstract
Purpose of Review
Many disorders involving the cerebral hemispheres have been identified and classified; however, in the last five years, significant progress has been made in the identification of genes involved in hindbrain development. Space constraints prohibit an exhaustive review of genetics of brain malformations encountered in the newborn. Rather, this review will address malformations of the corpus callosum, one of the more common malformations, and the hindbrain disorders, a less common entity.
Recent Findings
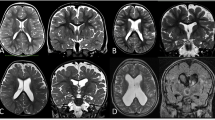
Neuroimaging of the brain is often one of the first steps in the determination of etiology and prognosis of an encephalopathic condition in the newborn. Structural anomalies of the brain are seen with some frequency in this setting. Due to the complex nature of cortical development, both genetic and non-genetic (environmental, toxins, etc.) factors may lead to a very similar pattern on MRI. In recent years, given the advances in genetic sequencing technologies as well as improvements in neuroimaging field, clarity, and technical advances in imaging sick and small infants, progress has been made to identify the genetic underpinnings of many cortical malformations. This has been particularly the case with regard to posterior fossa abnormalities.
Summary
Congenital malformations of the posterior fossa are relatively rare but are frequently more recognized, given the continuous improvements of neuroimaging. High-resolution genetic testing has led to identification of the etiology for some, but the cause of many still is elusive. Future application of high-resolution genetic testing such as whole exome sequencing will help identify other variants. MRI patterns may not sufficiently differentiate the clinical entities.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Gousias IS, Hammers A, Counsell SJ, et al. Magnetic resonance imaging of the newborn brain: automatic segmentation of brain images into 50 anatomical regions. PLoS One. 2013;8(4):e59990.
∙∙ Shroff MM, Soares-Fernandes JP, Whyte H, et al. MR imaging for diagnostic evaluation of encephalopathy in the newborn. Radiographics. 2010;30(3):763–80. This paper address the normal MR imaging appearances of the physiologic processes of myelination, cell migration, and sulcation, as well as patterns of injury, in the neonatal brain at various stages of gestational development. It also includes a differential diagnosis including metabolic and genetic etiologies.
Christidi F, Karavasilis E, Samiotis K, et al. Fiber tracking: a qualitative and quantitative comparison between four different software tools on the reconstruction of major white matter tracts. Eur J Radiol Open. 2016;18(3):153–61.
Li X, Gao J, Wang M, Wan M, Yang J. Rapid and reliable tract-based spatial statistics pipeline for diffusion imaging in the neonatal brain: applications to the white matter development and lesions. Magn Reson Imaging. 2016. doi:10.1016/j.mri.2016.07.011.
∙∙ Raybaud C. The corpus callosum, the other great forebrain commissures, and the septum pellucidum: anatomy, development, and malformation. Neuroradiology. 2010;52:447–77. This is a very comprehensive look at the anatomy, development, and radiological appearance of the mid-line structures: septum pellucidum and corpus callosum and demonstrates the continuum of malformations of these structures.
Hatten ME. Central nervous system neuronal migration. Annu Rev Neurosci. 1999;22:511–39.
Mihrshahi R. The corpus callosum as an evolutionary innovation. J Exp Zool (Mol Dev Evol). 2006;306B:8–17.
Silver J. Glia-neuron interactions at the midline of the developing mammalian brain and spinal cord. Perspect Dev Neurobiol. 1993;1:227–36.
Shu T, Richards LJ. Cortical axon guidance by glial wedge during the development of the corpus callosum. J Neurosci. 2001;21:2749–58.
Lent R, Uziel D, Baudrimont M, Fallet C, et al. Cellular and molecular tunnels surrounding the forebrain commissures of human fetus. J Comp Neurol. 2005;483:375–82.
Silver J, Lorenz SE, Wahlsten D, et al. Axonal guidance during development of the great cerebral commissures: descriptive and experimental studies, in vivo, on the role of preformed glial pathways. J Comp Neurol. 1982;210:10–29.
Myrianthopolous NC. Epidemiology of central nervous system malformations. In: Vinken PJ, Bruyn GW, Myrianthopolous NC, editors. Congenital malformations of the brain and skull. Amsterdam: North-Holland; 1977. p. 139–79.
Jeret JS, Serur D, Wisniewski KE, et al. Frequency of agenesis of the corpus callosum in the developmentally disabled population as determined by computerized tomography. Pediatr Neurosci. 1986;12:101–3.
Sowell ER, Mattson SN, Thompson PM. e. Mapping callosal morphology and cognitive correlates. Effects of heavy prenatal alcohol exposure. Neurology. 2001;57(2):235–44.
De Meirleir L. Disorders of pyruvate metabolism. Handb Clin Neurol. 2013;113:1667–73.
Sajan SA, Fernandez L, Nieh SE, et al. Both rare and de novo copy number variants are prevalent in agenesis of the corpus callosum but not in cerebellar hypoplasia or polymicrogyria. PLoS Genet. 2013;9(10):e1003823.
∙∙ Barkovich AJ, Millen KJ, Dobyns WB. A developmental classification of malformations of the brainstem. Ann Neurol. 2007;62(6):625–39. This is a very comprehensive article about the radiological and genetic characteristics of the midbrain malformations.
∙∙ Barkovich AJ, Millen KJ, Dobyns WB. A developmental and genetic classification for midbrain-hindbrain malformations. Brain. 2009;132(Pt 12):3199–230. This is a very comprehensive article about the genetics of the midbrain malformations and demonstrates the radiographic spectrum within the groups.
Abdel Razek AA, Castillo M. Magnetic resonance imaging of malformations of midbrain-hindbrain. J Comput Assist Tomogr. 2016;40(1):14–25.
Bosemani T, Poretti A, Huisman TA. Susceptibility-weighted imaging in pediatric neuroimaging. J Magn Reson Imaging. 2014;40(3):530–44.
Poretti A, Denecke J, Miller DC, et al. Brainstem disconnection: two additional patients and expansion of the phenotype. Neuropediatrics. 2015;46(2):139–44.
Jurkiewicz E, Dobrzańska A, Nowak K, et al. MRI findings in the young infant with brainstem disconnection and extracerebral features. Report of one case and review of the literature. Brain Dev. 2010;32(6):495–8.
DuffieldC, Jocson J, Wootton-Gorges SL. Brainstem disconnection. Pediatr Radiol. 2009;39(12):1357–60.
Barth PG, de Vries LS, Nikkels PG, et al. Congenital brainstem disconnection associated with a syrinx of the brainstem. Neuropediatrics. 2008;39(1):1–7.
∙ Ishak GE, Dempsey JC, Shaw DW, et al. Rhombencephalosynapsis: a hindbrain malformation associated with incomplete separation of midbrain and forebrain, hydrocephalus and a broad spectrum of severity. Brain. 2012;135(Pt 5):1370–86. This is an important reference in that it clarifies the presentations of rhomboencephalosynapsis, which is still underdiagnosed.
Whitehead MT, Choudhri AF, Grimm J, et al. Rhombencephalosynapsis as a cause of aqueductal stenosis: an under-recognized association in hydrocephalic children. Pediatr Radiol. 2014;44(7):849–56.
∙ Poretti A, Boltshauser E. Fetal diagnosis of rhombencephalosynapsis. Neuropediatrics. 2015;46(6):357–8. This is an important demonstration of the fetal diagnosis of atypical presentation of rhomboencephalosynapsis early in gestation.
Demurger F, Pasquier L, Dubourg C, et al. Array-CGH analysis suggests genetic heterogeneity in rhombencephalosynapsis. Mol Syndromol. 2013;4(6):267–72.
de Mattos VF, Graziadio C, Machado Rosa RF, et al. Gomez-Lopez-Hernandez syndrome in a child born to consanguineous parents: new evidence for an autosomal-recessive pattern of inheritance? Pediatr Neurol. 2014;50(6):612–5.
Parisi MA, Dobyns WB. Human malformations of the midbrain and hindbrain: review and proposed classification scheme. Mol Genet Metab. 2003;80(1–2):36–53.
Alexiou GA, Sfakianos G, Prodromou N. Dandy-Walker malformation: analysis of 19 cases. J Child Neurol. 2010;25(2):188–91.
Bokhari I, Rehman L, Hassan S, et al. Dandy-Walker malformation: a clinical and surgical outcome analysis. J Coll Physicians Surg Pak. 2015;25(6):431–3.
Aldinger KA, Lehmann OJ, Hudgins L, et al. FOXC1 is required for normal cerebellar development and is a major contributor to chromosome 6p25.3 Dandy-Walker malformation. Nat Genet. 2009;41(9):1037–42.
Reeder MR, Botto LD, Keppler-Noreuil KM, et al. Risk factors for Dandy-Walker malformation: a population-based assessment. Am J Med Genet A. 2015;9(16):1.
Zhang XB, Gu YQ, Sun XF, et al. Dandy-Walker complex: a clinicopathologic study of 9 cases. Zhonghua Bing Li Xue Za Zhi. 2013;42(12):815–8.
Mimaki M, Shiihara T, Watanabe M, et al. Holoprosencephaly with cerebellar vermis hypoplasia in 13q deletion syndrome: critical region for cerebellar dysgenesis within 13q32.2q34. Brain Dev. 2015;37(7):714–8.
Alp MY, Çebi AH, Seyhan S, et al. 22.5 MB Deletion of 13q31.1-q34 associated with HPE, DWM, and HSCR: a case report and redefining the smallest deleted regions. Genet Couns. 2016;27(1):43–9.
Peltekova IT, Hurteau-Millar J, Armour CM. Novel interstitial deletion of 10q24.3-25.1 associated with multiple congenital anomalies including lobar holoprosencephaly, cleft lip and palate, and hypoplastic kidneys. Am J Med Genet A. 2014;12(6):24.
Grinberg I, Northrup H, Ardinger H, et al. Heterozygous deletion of the linked genes ZIC1 and ZIC4 is involved in Dandy-Walker malformation. Nat Genet. 2004;36(10):1053–5.
Haldipur P, Gillies GS, Janson OK, et al. Foxc1 dependent mesenchymal signalling drives embryonic cerebellar growth. Elife. 2014;16(3):03962.
Wakeling EL, Jolly M, Fisk NM, et al. X-linked inheritance of Dandy-Walker variant. Clin Dysmorphol. 2002;11(1):15–8.
Parisi MA. Clinical and molecular features of Joubert syndrome and related disorders. Am J Med Genet C. Semin Med Genet. 2009;15(4):326–40.
Badano JL, Mitsuma N, Beales PL, et al. The ciliopathies: an emerging class of human genetic disorders. Annu Rev Genom Hum Genet. 2006;7:125–48.
Briguglio M, Pinelli L, Giordano L, et al. Pontine tegmental cap dysplasia: developmental and cognitive outcome in three adolescent patients. Orphanet J Rare Dis. 2011;6(36):1750–72.
Bachmann-Gagescu R, Dempsey JC, Phelps IG, et al. Joubert syndrome: a model for untangling recessive disorders with extreme genetic heterogeneity. J Med Genet. 2015;52(8):514–22.
Suzuki T, Miyake N, Tsurusaki Y, et al. Molecular genetic analysis of 30 families with Joubert syndrome. Clin Genet. 2016;19(10):12836.
Ben-Salem S, Al-Shamsi AM, Gleeson JG, et al. Mutation spectrum of Joubert syndrome and related disorders among Arabs. Hum Genome Var. 2014;1:14020.
Poretti A, Huisman TA, Scheer I, et al. Joubert syndrome and related disorders: spectrum of neuroimaging findings in 75 patients. AJNR Am J Neuroradiol. 2011;32(8):1459–63.
Poretti A, Meoded A, Rossi A, et al. Diffusion tensor imaging in Joubert syndrome. AJNR Am J Neuroradiol. 2007;28(10):1929–33.
Jissendi-Tchofo P, Doherty D, McGillivray G, et al. Pontine tegmental cap dysplasia: MR imaging and diffusion tensor imaging features of impaired axonal navigation. AJNR. 2009;30(1):113–9.
Caan M, Barth PG, Niermeijer JM, et al. Ectopic peripontine arcuate fibres, a novel finding in pontine tegmental cap dysplasia. Eur J Paediatr Neurol. 2014;18(3):434–8.
Barth PG, Majoie CB, Caan MW, et al. Pontine tegmental cap dysplasia: a novel brain malformation with a defect in axonal guidance. Brain. 2007;130(Pt 9):2258–66.
Singh D, Hsu CC, Kwan GN, et al. Pontine tegmental cap dysplasia: MR evaluation of vestibulocochlear neuropathy. J Neuroimaging. 2015;25(6):1038–43.
Nixon JN, Dempsey JC, Doherty D, et al. Temporal bone and cranial nerve findings in pontine tegmental cap dysplasia. Neuroradiology. 2016;58(2):179–87.
Clement E, Mercuri E, Godfrey C, et al. Brain involvement in muscular dystrophies with defective dystroglycan glycosylation. Ann Neurol. 2008;64(5):573–82.
Barth PG. Pontocerebellar hypoplasias. An overview of a group of inherited neurodegenerative disorders with fetal onset. Brain Dev. 1993;15(6):411–22.
Tentler D, Leisti J, Schueler M, et al. Deletion including the oligophrenin-1 gene associated with enlarged cerebral ventricles, cerebellar hypoplasia, seizures and ataxia. Eur J Hum Genet. 1999;7(5):541–8.
Vermeulen RJ, Peeters-Scholte C, Van Vugt JJ, et al. Fetal origin of brain damage in 2 infants with a COL4A1 mutation: fetal and neonatal MRI. Neuropediatrics. 2011;42(1):1–3.
Siegel DH, Tefft KA, Kelly T, et al. Stroke in children with posterior fossa brain malformations, hemangiomas, arterial anomalies, coarctation of the aorta and cardiac defects, and eye abnormalities (PHACE) syndrome: a systematic review of the literature. Stroke. 2012;43(6):1672–4.
Hess CP, Fullerton HJ, Metry DW, et al. Cervical and intracranial arterial anomalies in 70 patients with PHACE syndrome. AJNR. 2010;31(10):1980–6.
Millen KJ, Steshina EY, Iskusnykh IY, et al. Transformation of the cerebellum into more ventral brainstem fates causes cerebellar agenesis in the absence of Ptf1a function. Proc Natl Acad Sci USA. 2014;111(17):14.
Aldinger KA, Mendelsohn NJ, Chung BH, et al. Variable brain phenotype primarily affects the brainstem and cerebellum in patients with osteogenesis imperfecta caused by recessive WNT1 mutations. J Med Genet. 2016;53(6):427–30.
Mester J, Eng C. When overgrowth bumps into cancer: the PTEN-opathies. Am J Med Genet C. 2013;2:114–21.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosure
Amali Mallawaarachchi and Felicity Collins declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical collection on Genetics.
Rights and permissions
About this article
Cite this article
Obeid, R., Gropman, A.L. The New Findings in the Genetics and Pathology of Structural Brain Diseases. Curr Pediatr Rep 4, 164–172 (2016). https://doi.org/10.1007/s40124-016-0112-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40124-016-0112-5