Abstract
Introduction
The peripheral nervous system is an increasingly popular target for chronic pain treatment modalities. Noninvasive neuromodulation has shown promise at providing significant chronic pain relief with a much safer side effect profile. This retrospective pilot study is shaped around a noninvasive neuromodulation system over a 2-week treatment timeline.
Methods
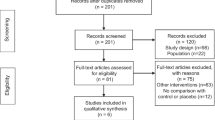
Open-label survey of chronic pain patients recruited from Veteran Affairs, orthopedic, and pain health systems. If a noninvasive neuromodulation system was prescribed the patients were then offered a 2-week follow-up survey. This voluntary survey did not affect their therapy duration or quality. This survey was designed to address similar metrics as smaller noninvasive neuromodulation studies to allow a quality comparison while giving more power with a large population size of 1511 patients. Overall pain scores (including before and after scores), satisfaction level, desire to continue therapy, medication use, effect on functional metrics (mood, sleep, sit, stand, walk, and lift), and activities of daily living (ADL) scores were assessed.
Results
The results demonstrated an overall pain reduction of 46%. All functional metrics were improved throughout with the largest improvements reported in mood and sleep at over 47%. Medication use was reported as decreased or eliminated in 42% of patients. There were no adverse reactions or complications reported over the 1511 patients.
Conclusion
This survey is amongst the largest population sizes every studied for noninvasive neuromodulation. Within just 2 weeks patients can see a reduction in overall pain and medication needs. Although survey studies have inherent limitations such as duration and compliance biases with such an overwhelming benefit in every category we believe that noninvasive neuromodulation therapy is a promising, safe, and cost-effective therapy. Future studies should focus on long-term follow-ups and post-therapy pain scores with a placebo group.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Our study aimed at assessing the efficacy of non-invasive nerve stimulation using BioWave in treating chronic pain. |
This was a survey study measuring pain scores before and after use of the device. |
Study outcomes also included measurement of any adverse outcomes. |
Out study concluded that this mode of therapy is effective. |
Introduction
The prevalence of chronic pain continues to rise each year. A number of epidemiological studies done in various regions of the world found that chronic pain prevalence rates ranged from 12% to 80% depending on the country and demographic [1]. Chronic pain is often regarded as the most underappreciated healthcare issue affecting people’s quality of life. In particular, chronic low back pain remains a difficult to treat clinical entity for which there is an unmet need for effective noninvasive interventions. The biological, psychological, sociodemographic, and behavioral effects of pain must all be considered when developing safe, preventative therapies [2].
The modern neuromodulation era began around the turn of the millennium, when a search for new therapies to effectively treat mental disorders with noninvasive, well-tolerated methods piqued interest, and studies on the influence of direct current on cerebral cortex excitability were pursued [3]. Electroconvulsive therapy (ECT), transcranial electrical stimulation (TES), transcranial magnetic stimulation (TMS), static magnetic stimulation, transcranial direct current stimulation (tDCS), transcranial alternating current stimulation (tACS), random noise stimulation, ultrasound/focused ultrasound stimulation (FUS), and peripheral/cranial nerve stimulation are among the many noninvasive neuromodulatory techniques available today [4]. These technologies can be used to change brain circuitry for a number of therapeutic and nontherapeutic objectives, in addition to providing insight into our nervous system physiology.
The peripheral nervous system (PNS) provides a vital conduit of communication between the body and the environment. The PNS is an accessible window allowing physicians to manage both acute and chronic pain. Therapies that work via the PNS can be segregated into invasive techniques, including spinal cord stimulators, and noninvasive techniques such as transcutaneous electrical nerve stimulation (TENS) and PNS stimulators. This study focuses on the latter. The noninvasive neuromodulation therapy utilizes a high frequency electric field to bypass the skin’s impedance. Two sinusoidal high frequency signals then penetrate deep tissues while a low frequency electric current spanning 1–180 Hz halts the action potentials’ propagation. This creates a 4–6-cm region underneath the electrodes which is hypothesized to hyperpolarize the nearby C fibers. This hyperpolarization works via the frequency conduction block theory (FCBT) to inhibit the pain signals [5]. The principle of the FCBT is the multiplication of two sine waves that leads to the hyperpolarization of the C fibers (Fig. 1). The FCBT has parallels with the well-known gate control theory which targets the central nervous system and is utilized in spinal cord stimulators (SCS) [6].
Neuromodulation devices have proven to be a viable and safe alternative to traditional pharmaceutical therapies, with several studies demonstrating quality efficacy for migraine and cluster headaches [7].
Neuromodulation often uses either a tonic stimulation, where pulse signals are continuously fired over a set duration, or a more novel burst waveform pattern, where pulse signals are sent in rapid succession. The Neuromodulation with BURST (SUNBURST) study was a randomized control study that demonstrated that burst stimulation was superior to the traditional tonic stimulation. The study indicated that patients preferred a treatment modality that was below the perception threshold [8].
TENS is a widely used noninvasive tonic neuromodulation treatment modality. The TENS nomenclature is based on the output of the device and not the physiological intention of the current. Conventional TENS selectively activates large diameter afferents via low intensity and low frequency signals typically in the range between 1 and 180 Hz. The intense TENS activates small diameter noxious afferents to elicit peripheral nerve blockade via high intensity and high frequency. TENS uses hyperstimulation and paresthesias to inhibit activity in the second-order nociceptive transmission [4, 9].
Noninvasive neuromodulators provide an alternative treatment modality for several acute and chronic pain conditions. These devices may offer a unique treatment flexibility since they may be employed as an early therapy, either alone or in conjunction with pharmaceutical treatment. Noninvasive neuromodulation is also a unique option for people in vulnerable patient groups, e.g., pregnant women and adolescents, as well as those who have had poor tolerability or effectiveness with pharmacologics [7,8,9].
Over the past 10 years the technology for PNS has advanced rapidly [10, 11]. For example, the first randomized control trial (RCT) that compared the efficacy of peripheral nerve field stimulation (PNFS) plus conventional medical management (CMM) vs CMM alone was in November 2012 when Medtronic Inc. performed the SubQStim II Study [12,13,14,15]. Neuromodulation now has several different leads and techniques that can be implemented for different subtypes of chronic pain.
We performed an open-label pilot study intended to add strength and depth to the current research of noninvasive burst neuromodulation effectiveness in people with chronic pain. A previous study of 463 individuals who were surveyed after 2 weeks of noninvasive neuromodulation therapy showed an average pain reduction of 3.05 points on a Numeric Pain Scale (NPS) [16]. This prompted follow-up studies with larger power to assess the efficacy of noninvasive neuromodulation therapy as a promising, safe, and cost-effective treatment modality.
Methods
Participants
This pilot study was performed via retrospective review of volunteer surveys performed by patients with chronic pain primarily through Veterans Affairs (VA), pain centers, and orthopedic hospital systems over a 24-month period. The number of units shipped from January 1, 2021 through November 25, 2022 in the VA was 8779 and the number of surveys completed within the same time period for the VA was 1962. Therefore, the response rate is 22.4%. The majority of patients were male (66% of 1511 patients; Table 1). A wide variety of chronic pain subtypes were treated, the most common being back pain and neck pain (60% and 9%, respectively; Table 3). There were patients with more than one chronic pain location; however, the survey recorded the primary site of treatment. Those not able to understand English, and patients not capable of operating the noninvasive neuromodulation device were excluded. The subject of this study is a clinically tested at-home neuromodulation device called the BioWaveHOME (Norwalk, CT, USA: BioWave Corporation). This study was ethically sound and an institutional review board (IRB) waiver was obtained.
Each patient had a thorough noninvasive neuromodulation system demonstration where they learned the necessary skills to perform a standardized treatment and the 2-week survey was discussed. The patient’s willingness to participate in the survey did not impact their quality or duration of care. After 2 weeks of noninvasive neuromodulation therapy the surveys were collected.
Questionnaire
A questionnaire was designed and tested the survey in conjunction with healthcare providers and patients from VA Hospitals. Mock-up surveys were created and refined several times incorporating both provider and patient feedback. The survey consisted of 15 questions: pain score reduction (with pre- and post-therapy scores), activities of daily living (ADL) score change (with pre and post scores), primary chronic pain location, change in quality of life (QoL), mood, desire to continue therapy, satisfaction level, medication use, and effects on functional metrics: mood, sleep, sit, stand, walk, and lift (Fig. 2). The activity of daily living score comes from a 10-point scale that assess hygiene, dressing, toileting, locomotion, continence, and meals. There was also an optional written section for patient comments and side effects. SPSS version 26 was used to perform the analysis which included descriptive analysis expressing data as numbers and percent. Pre- and post-intervention measures were presented as mean ± SD and compared using paired t test. A p value ≤ 0.05 was considered significant.
The patient treatment surveys were collected in several ways. The majority were received via mail followed by fax or email. Patients had the option to request phone surveys. In this scenario written consent from the provider to contact patients was obtained. Surveys were then entered into the electronic data collection system.
Noninvasive Neuromodulation
The BioWaveHOME system is a name brand noninvasive peripheral nerve stimulator. PNS stimulators are designed for temporary use and placement often occurs earlier in the perioperative setting. Devices are often removed between 14 and 60 days [11]. The systems consist of a control unit (Fig. 3a) and two types of electrodes. B-set electrodes (two 2-inch-diameter round electrodes) which are used in several fashions; two distinct areas of localized pain, origin and proximal pain location (radiculopathies), or one general area of pain (Fig. 3b). There is an alternative E-set electrode configuration, which is designed for treating a single location of pain. The E-set is comprised of a smaller 1.375-inch-diameter round electrode placed directly over the localized pain site; and a large 2 × 4 inch rectangular dispersive electrode that is placed over a bony prominence typically near the pain site, which is a comfortable location, to receive a deep soothing stimulation (Fig. 3c). The electrodes allow for the delivery of two high frequency sinusoidal signals to bypass the skin’s impedance and penetrate deep tissues. Tissues that have a charge associated with them, like the membrane of the C fiber, act in a nonlinear fashion and force the multiplication of the two high frequency signals which results in the formation of a low frequency electrical field with current at 122 Hz, 4 kHz, 4.122 kHz, and 8.122 kHz that halt action potentials’ propagation. This creates a 4–6-cm region underneath the electrodes which hyperpolarizes the nearby C fibers.
Results
A total of 1511 participants completed surveys over the 24-month window; 66% were men while 20% were female and 14% did not indicate a gender (Table 1). The mean starting pain score was 7.56 with an average reduction of 3.47 (Fig. 4). This was a statistically significant reduction (p < 0.001) in pain over a 2-week period (Table 2). A before and after ADL score demonstrated a vast improvement for most participants with the mean increase of 2.54 (p < 0.001) (Table 2).
The most common primary pain location among survey respondents was chronic back pain at 60%. This was followed by neck pain 9%, and ankle/foot pain 8% (Table 3). It is reported that 40–70% of patients with chronic pain report discomfort in more than one anatomical region so our survey recorded the primary site and treatment location [1].
Lifestyle metrics included quality of life (QoL), medication usage, and overall satisfaction rate. An improvement in QoL was reported by 87.6% of patients (Table 4). One-third of patients reported a reduction of medication while an additional 6% reported eliminating medication all together (Table 4). Patients were able to respond as eliminated, decreased, and unchanged medication use; 42% of patients reported that they were able to eliminate or reduce their medications and 39% reported no change in their medications. Overall, the noninvasive neuromodulation system satisfaction rate was 8.35 on a scale of 0–10 and 97.2% of patients wanted to continue therapy after completing the survey (Table 5).
Functional Outcomes
Functional outcomes, i.e., ability sit, stand, walk, and lift along with sleep and mood, were assessed. Patients were given the option of their ability to perform said tasks as improved, same, or decreased. There was an average improvement in all activities. Almost half of all patients reported sleep 47.9% and mood 47.7% being the most improved (Table 6).
Discussion
This open-label pilot study demonstrated significant improvement for patients with chronic pain in several key areas: quantitative pain levels, activities of daily living, quality of life, medication usage, functional metrics, and overall satisfaction. It is worth noting that this unique bioelectronic therapy was able to produce these results in a time frame of just 2 weeks.
Our survey had one of the largest population sizes of any PNS neuromodulation study with 1511 patients. This pilot survey demonstrated an overall satisfaction rate of 97% and an average pain reduction of 3.47. This is in line with previous studies of noninvasive high frequency neuromodulation [16]. Our study was able to provide a strong correlation with all metrics. Despite the potential for selection bias amongst the survey respondents, data with positive improvement across a large group of subjects suggests possible underlying efficacy. Combined with the safe and at-home nature of this therapy, these results highlight the potential for this emerging form of electrotherapy.
TENS is used in a wide variety of chronic pain subsets; however, its efficacy is controversial. A large randomized, sham-controlled pilot crossover trial compared TENS and a placebo TENS therapy and found that although TENS was safe it was unlikely to offer more analgesic effects than a placebo [17].
There are many similarities between the new noninvasive neurmodulation techniques and TENS machines. They are both small, portable, battery-operated devices that use electricity to treat pain in a noninvasive pattern. The main difference is the hypothetical ability of the new neuromodulation systems to use alternating currents to block the pain signals via hyperpolarization.
While the technical revolution in PNS proceeds apace, fundamental concerns of biophysical and therapeutic significance remain unanswered. For example, the importance of contact spacing and several independent current controllers, as well as the advantages of constant current versus constant voltage schemes, is unknown. The appropriate number or arrangement of leads for controlling back pain with unilateral or bilateral leg discomfort must be determined [18, 19].
Our survey’s universal improvements were seen independent of the clinical subgroup. With the majority of the patients in this survey comprising veterans, it is promising to see a new therapy demonstrate significant benefit for this at-risk population. To better assess chronic pain treatment in veterans a study that integrates post-traumatic stress disorder (PTSD) scores and parallel coping strategies paired with neuromodulation could show a synergistic relationship between treatment modalities.
A noninvasive treatment modality that has a large safety profile with the ability to be reversed has numerous advantages. Chronic pain can often develop after surgical procedures making patients more reluctant to undergo another invasive procedure. Having a treatment option that does not require an operation could help patient adherence and possibly lead to treating chronic pain earlier in its disease process [20, 21].
Our large pilot study of 1511 patients demonstrates that the alternating current of the noninvasive neuromodulation system has the potential to treat numerous types of chronic pain conditions. Follow-up studies should be conducted to assess length of chronic pain reduction after treatment has stopped. They should also randomize placebo, new noninvasive neurmodulation techniques, and TENS treatment groups. Placebo effects can account for up to 30% of pain improvement in this population which could be further delineated with a control group in future studies [9].
Surveys and survey-based studies have inherent limitations. Compliance is potentially biased when it requires effort to submit the survey which is more likely if one has been performing their treatments. It is difficult to assess dishonest questionnaire answers or to assess a respondent’s potential agenda. Patients may not be aware of the importance of each answer and the nuances between question choices despite prior survey education.
Despite having one of the largest noninvasive neuromodulation study populations the patients surveyed were biased towards men and specifically those in the VA health systems. This is a specific limitation when the prevalence of both acute and chronic pain is higher among women than men, with 66% of elderly women reporting pain in the past 4 weeks vs 57% of elderly men [22].
A way to strengthen future surveys would be to increase the length of treatment and the addition of a period without treatment. This could be accomplished in a follow-up survey. Although our survey portrays a significant pain reduction in a short period of time we have no data to suggest its longevity at this time.
Conclusion
Noninvasive neuromodulation is a promising treatment strategy for various types of chronic pain. We performed one of the largest noninvasive neuromodulation studies with 1511 patients surveyed. Patients from orthopedic, chronic pain, and the vulnerable population in the Veteran Affair Health Systems demonstrated considerable improvement in multiple categories, including quantitative pain levels, activities of daily living, sleep, mood, and numerous functional data points. The findings of this study generally matched those of prior noninvasive neuromodulation device studies and noninvasive neuromodulation investigations, while also providing much-needed power and reproducibility. This pilot study helps highlight the potential benefits of novel noninvasive neuromodulation treatment modalities while calling for randomized trials comparing neurostimulation devices versus placebo and TENS.
References
Mills SEE, Nicolson KP, Smith BH. Chronic pain: a review of its epidemiology and associated factors in population-based studies. Br J Anaesth. 2019;123(2):e273–83. https://doi.org/10.1016/j.bja.2019.03.023.
Pitcher MH, Von Korff M, Bushnell MC, Porter L. Prevalence and profile of high-impact chronic pain in the United States. J Pain. 2019;20:146–60.
Wang J, Chen Z. Neuromodulation for pain management. Adv Exp Med Biol. 2019;1101:207–23. https://doi.org/10.1007/978-981-13-2050-7_8.
Gibson W, Wand BM, Meads C, Catley MJ, O’Connell NE. Transcutaneous electrical nerve stimulation (TENS) for chronic pain—an overview of Cochrane Reviews. Cochrane Database Syst Rev. 2019;4:CD011890.
Kilgore KL, Bhadra N. Nerve conduction block utilizing high-frequency alternating current. Med Biol Eng Comput. 2004;42(3):394–406. https://doi.org/10.1007/BF02344716.
Reuter U, McClure C, Liebler E, et al. Non-invasive neuromodulation for migraine and cluster headache: a systematic review of clinical trials. J Neurol Neurosurg Psychiatry. 2019;90:796–804.
Deer T, Slavin KV, Amirdelfan K, et al. Success using neuromodulation with burst (SUNBURST) study: results from a prospective, randomized controlled trial using a novel burst waveform. Neuromodulation. 2018;21(1):56–66. https://doi.org/10.1111/ner.12698.
Johnson M. Transcutaneous electrical nerve stimulation: mechanisms. Clin Appl Evid Rev Pain. 2007;1(1):7–11. https://doi.org/10.1177/204946370700100103.
Eldabe S, Kern M, Peul W, Green C, Winterfeldt K, Taylor RS. Assessing the effectiveness and cost effectiveness of subcutaneous nerve stimulation in patients with predominant back pain due to failed back surgery syndrome (SubQStim study): study protocol for a multicenter randomized controlled trial. Trials. 2013;14:189. https://doi.org/10.1186/1745-6215-14-189.
Helm S, Shirsat N, Calodney A, et al. Peripheral nerve stimulation for chronic pain: a systematic review of effectiveness and safety. Pain Ther. 2021;10(2):985–1002.
Abd-Elsayed A, D’Souza RS. Peripheral nerve stimulation: the evolution in pain medicine. Biomedicines. 2021;10(1):18.
Hegarty DA, Bretherton B. An open-label pilot study investigating noninvasive high-frequency peripheral nerve fiber stimulation in chronic pain. Pain Pract. 2021;21(5):578–87. https://doi.org/10.1111/papr.12993.
Fiala KJ, Kim RB, Martens JM, Abd-Elsayed A. Lumbar level peripheral nerve stimulation for low back pain. Ochsner J. 2022;22(3):265–72.
Abd-Elsayed A. Wireless peripheral nerve stimulation for treatment of peripheral neuralgias. Neuromodulation. 2020;23(6):827–30.
Busch C, Smith O, Weaver T, Vallabh J, Abd-Elsayed A. Peripheral nerve stimulation for lower extremity pain. Biomedicines. 2022;10(7):1666. https://doi.org/10.3390/biomedicines10071666.
Abd-Elsayed A, Tang T, Karri J, et al. Neuromodulation for pain management in the inpatient setting: a narrative review. Cureus. 2021;13(3):e13892. https://doi.org/10.7759/cureus.13892.
Siemens W, Boehlke C, Bennett MI, Offner K, Becker G, Gaertner J. Transcutaneous electrical nerve stimulation for advanced cancer pain inpatients in specialist palliative care—a blinded, randomized, sham-controlled pilot cross-over trial. Support Care Cancer. 2020;28(11):5323–33. https://doi.org/10.1007/s00520-020-05370-8.
Kumar K, Rizvi S. Spinal cord stimulation and other neuromodulation: in chronic pain. In: Toth C, Moulin D, editors. Neuropathic pain: causes, management and understanding. Cambridge: Cambridge University Press; 2013.
Gyorfi M, Abd-Elsayed A. Peripheral nerve stimulator for treating sural and posterior tibial neuralgias—case report. Pain Med Case Rep. 2021;5:413–416
Slavin KV. History of peripheral nerve stimulation. Prog Neurol Surg. 2011;24:1–15.
Xu J, Sun Z, Wu J, et al. Peripheral nerve stimulation in pain management: a systematic review. Pain Physician. 2021;24(2):E131–52.
Musey PI Jr, Linnstaedt SD, Platts-Mills TF, et al. Gender differences in acute and chronic pain in the emergency department: results of the 2014 Academic Emergency Medicine consensus conference pain section. Acad Emerg Med. 2014;21(12):1421–30. https://doi.org/10.1111/acem.12529.
Acknowledgements
Funding
funding was received for the publication
Authors’ Contributions
Alaa Abd-Elsayed, MD, MPH, FASA: Study design, data analysis and manuscript writing. Michael Gyorfi, MD: Data analysis and manuscript writing. Michael Fischman, MD: Study design and manuscript writing. Charles Odonkor, MD: Study design and, manuscript writing. Bradford Siff: data collection and manuscript writing. Kevin Cyr: data collection and manuscript writing.
Disclosures
Alaa Abd-Elsayed, Michael Fischman, Charles Odonkor are consultants fir BioWave, Bradfor Siff and Kevin Cyr have appointments with Biowave.
Compliance with Ethics Guidelines
This study was ethically sound and an IRB waiver was obtained from the University of Wisconsin.
Data Availability
The data sets generated during and/or analyzed during the current study are not publicly available due to the need for patient data protection and the lack of IRB permission to share it in public.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Abd-Elsayed, A., Gyorfi, M., Fischman, M. et al. Reduced Pain and Improved Function Following Short-Term Use of Noninvasive BioWave High Frequency Peripheral Nerve Stimulation for Pain Management. Pain Ther 12, 553–562 (2023). https://doi.org/10.1007/s40122-023-00480-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-023-00480-7