Abstract
Introduction
Postoperative cancer pain imposes severe physical and psychological problems. We aimed to investigate the pain experiences of patients with cancer after surgery, analyze the impact of infusion volume by patient-controlled analgesia (PCA), and explore the variations between day 1 and day 2.
Methods
Data were retrospectively extracted from a large health data platform. Descriptive statistics were presented for the demographic and clinical profiles of patients. Multiple logistic regression analyses were performed to evaluate associations between intensity of pain and PCA use after adjustment for risk factors.
Results
Among 11,383 patients with cancer, the incidence of pain (moderate to severe pain) was 93.3% (18.3%) at the first 24 h after operation, while the respect values decreased to 91.1% and 9.5% at the second 24 h. Further, female patients consistently experienced higher risk of pain over the whole 48 h postoperatively. Surgical sites were related to pain risk, with the highest risk among the respiratory system (OR 2.077, 95% CI 1.392–3.100). High doses of continuous volume (OR 2.453, 95% CI 1.742–3.456) and total volume (OR 2.830, 95% CI 2.037–3.934) of infusions were related to 1–3-fold elevated pain risk. Additionally, the observed associations were mostly repeated and could be up to over 10 times when pain was evaluated with number of PCA pump compressions instead of Numerical Rating Scale (NRS).
Conclusions
High risk of postoperative cancer pain, particularly among the high PCA dose group, could possibly indicate inadequate pain control, and presence of modifiable risk factors warrants more aggressive pain management strategies perioperatively.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
•How to obtain an accurate dosage of intravenous patient-controlled analgesia (IV-PCA) in clinical practice needs real-world evidence, especially that based on a large amount of data. •The purpose of this research was to observe the incidence of postoperative pain, investigate the risk factors influencing postoperative pain, and dissect the association between PCA usage and postoperative pain in the first 24 h and the second 24 h after surgery, which had not been done much on the basis of a large sample size. |
What was learned from the study? |
•Our research corroborates high risk of postoperative cancer pain, identifies associated risk factors, and quantifies analgesic effect of PCA. •All of these could together indicate inadequate pain control if opioid-induced hyperalgesia could be excluded. •Presence of modifiable risk factors warrants more aggressive pain management strategies perioperatively. |
Introduction
Today, patients with cancer live longer owing to the significant therapeutic effects of new cancer therapies. However, pain is still one of the most distressing and burdensome symptoms of cancer and cancer therapies, affecting all aspects of a patient’s life. Patient-controlled analgesia (PCA) has been utilized to optimize pain relief since 1971, with the first commercially available PCA pump appearing in 1976. The goal of PCA is to efficiently deliver pain relief at a patient’s preferred dose and schedule by allowing them to administer a predetermined bolus dose of medication on-demand at the press of a button. PCA has proven to be more effective at pain control than non-patient opioid injections and results in higher patient satisfaction, especially in patients who are unable to tolerate oral medications.
Intravenous patient-controlled analgesia (IV-PCA) with continuous infusion of opioids upon the patient’s individual analgesic needs is widely used to manage acute postoperative pain [1, 2]. IV-PCA has become the most common standard modality for postoperative pain control worldwide and is associated with high satisfaction rates [3, 4]. PCA pumps used in the postoperative setting decrease total opioid consumption and increase patient and nurse satisfaction.
Approximately 15.5 million cancer survivors were alive in the USA in 2016, and that number is expected to increase to nearly 20 million by 2026 because nearly half of cancer survivors live longer than 10 years. There are 2.8 million incident patients with diagnosis of advanced cancer in China annually, of which 80% have pain and 70% have not been effectively treated [5]. Identification of demographic, physiologic, clinical, and behavioral correlates of pain among cancer survivors could help identify subgroups most in need of pain management.
However, how to obtain an accurate dosage of IV-PCA in clinical practice needs real-world evidence, especially that based on a large amount of data. This is because a large sample could more accurately reflect the safety and efficacy of PCA usage, better eliminate the distortion of designated association from various covariates, and provide the change to do the stratified analyses, all of which could help improve issues such as the safety of nursing care and further influence future clinical practice guidelines (CPG) [6, 7]. In the present study, in addition to providing information on distribution and associated risk factors of pain after surgical operation, we in particular aimed to compare the pain intensity and PCA use after multiple adjustment among the first and second 24 h after surgery, assuming that the residual effects of operative anesthesia still existed at the first 24 h and had disappeared at the second. We also used Numerical Rating Scale (NRS) and numbers of PCA pump compressions as the study outcomes in parallel. Recording the number of compressions together with NRS is necessary, and there was a previous article which analyzed the number of compressions as a secondary outcome in comparison with pain [8].
Methods
Data Sources and Study Population
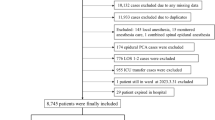
All data used in the study were extracted from the health data platform of Rehn Medtech (RM: www.rehn.cc) (Jiangsu, China) which is a big-data intelligence platform that integrates and converges mass multisource heterogeneous electronic health records data from multiple medical centers or hospitals all over China (over 500 hospitals in 28 provinces for the time being).
The study population comprised patients with cancer having their surgery in Nantong tumor hospitals during January 1, 2014–December 31, 2019, which were intercepted via the RM platform. The exclusion criteria were as follows: (1) less than 18 years of age; (2) refused to participate in the study; (3) was not present in room or had been discharged at the time of data collection; (4) had cognitive deficits. The final cohort for the analyses consisted of 11,383 patients.
Intravenous Patient-Controlled Analgesia and Covariates
Dosage of PCA including continuous volume of infusion and total volume of infusion in the first and second 24 h as well as a series of demographic and clinical characteristics, mainly age, gender, weight, surgical mode, surgical site, and medication classification, was abstracted from the medical intelligence platform, i.e., RM, for the present study.
All patients received general anesthesia during the operation. After surgery, patients were transferred to the post-anesthesia care unit (PACU), where intravenous self-administered PCA was initiated, containing either sufentanil or non-sufentanil. A lock-in period of 5–15 min was set in order to avoid overdose of these drugs. The continuous volume of infusion was the amount of drug infused uniformly over 1 h, i.e., the rate of administration per hour. In the analyses, we categorized the continuous volume as 0.1–1.1, 1.2–1.4, 1.5–1.6, or > 1.6 ml/h according to the interquartile method for both the first and second 24 h. In the same way, the total volume of infusion in the first 24 h was grouped into four groups: ≤ 27 ml, 28–34 ml, 35–43 ml, and > 43 ml; the total volume of infusion in the second 24 h was divided into four groups: ≤ 30 ml, 31–37 ml, 38–46 ml, and > 46 ml.
Age and weight were analyzed as continuous variables. Other variables were analyzed as categorical variables: gender was analyzed as male or female, surgical mode was categorized as non-lumpectomy or lumpectomy, surgical sites were grouped into digestive system, urinary system, reproductive system, respiratory system, blood circulatory system, and other systems considering the feasibility of the data, and medication was characterized as sufentanil or non-sufentanil.
In this study, we intentionally investigated and compared the effect of PCA in the first and second 24 h given the fact that the effect of general anesthesia from the surgery still existed in the first day after operation, but not in the second day.
Study Outcomes
The main outcomes in this study included NRS and number of PCA pump compressions in parallel.
First, patients were asked to rate their current pain during movement using a numeric rating scale, the NRS (0–10): “Please rate your current pain during movement by indicating the number that best describes your pain, where 0 indicates no pain and 10 indicates the most severe pain.” They were asked to rate the severity of their postoperative pain for each of the two postoperative days. On the basis of the NRS score, we classified patients into three categories of pain, namely, no pain (0), mild pain (1–3/10), and moderate to severe pain (≥ 4/10).
Second, we included the number of PCA pump compressions as an additional outcome variable to evaluate the association of postoperative pain and PCA use. PCA patients were trained and tested in the use of the PCA pump. If the patient presses three times in 15 min, the reason was recorded. The reason for multiple compressions was inadequate pain control [9]. In our research when the patient hit the self-control button more than three times inside the limited period, the central monitoring workstation indicated insufficient analgesia, which immediately alerted our medical personnel to deal with it appropriately. This outcome was set as a dichotomous variable: more than three times, and three times or less.
In the present study, we compared the consistency of these two outcomes, which represented the intensity of pain in patients in different ways. To our knowledge, this had not been reported in previous studies to date.
Statistical Analysis
Descriptive statistics were first performed: continuous variables were presented as mean ± standard deviation, and categorical data were expressed as numbers and percentages. Univariate analyses were then conducted: continuous variables were compared using analysis of variance (ANOVA) and categorical variables were compared using chi-square whenever it was appropriate. Next, multivariate logistic regression analysis was used to assess the relationship between the degree of pain, either NRS index (no pain, mild pain, and moderate to severe pain) or the numbers of PCA pump compressions (> 3 or ≤ 3), and infusion volume of IV-PCA after adjustment for associated risk factors.
All analyses were performed using the SAS statistical package ver. 9.4. (SAS Institute Inc., Cary, NC). All p values were based on two-sided tests, with the statistical significance level set to 0.05.
Compliance with Ethics Guidelines
Our research protocols were approved by the institutional review boards of Nantong Tumor Hospital (IRB2018-010). For the safety and rationality of the research, we signed the informed consent for all the participants. The implementation of the current study adhered to the tenets of the Declaration of Helsinki of the World Medical Association with regard to scientific research on human subjects. In order to preserve anonymity, individual records of all participants were de-identified before the analysis.
Results
Data on a total of 11,383 patients with cancer who underwent surgery were retrospectively analyzed, all of whom were evaluated for pain during movement. Of these, 9382 patients and 10,032 patients went through pain evaluation according to NRS within the first 24 h and the second 24 h after surgery, respectively. The respective reporting rates of pain for the first and second 24 h were 93.3% and 91.1%. Among them, there were 74.9% (n = 7030) of mild pain and 18.3% (n = 1721) of moderate to severe pain reported in the first 24 h compared to 81.6% (n = 8188) of mild pain and 9.5% (n = 949) of moderate to severe pain in the second.
We observed that distribution of pain incidence rates was statistically different by gender, surgical mode, surgical site, continuous volume, and total volume of infusions administered on both the first and second 24 h after surgery (Table 1). Weight was statistically different only on postoperative 24 h, while age was statistically different only on postoperative 48 h. Compared to male patients, a higher percentage of female patients had mild pain on both day 1 and day 2. In terms of surgical mode, a significantly higher proportion of patients who underwent lumpectomy suffered mild pain and moderate to severe pain compared to those who received non-lumpectomy surgery. About 25% of these procedures are lumpectomies and about 75% are non-lumpectomies. Difference of use of minimally invasive surgery was not statistically significant by surgery time (X2 = 6.5349, p = 0.163). The proportion of pain varied a lot according to surgical sites in different systems, with the highest in the respiratory system followed by digestive system and others, especially for moderate to severe pain. Notably, the highest proportions of moderate to severe pain were consistently observed among the highest dosage group of both “continuous volume of PCA infusion” and “total volume of PCA infusion”. The main tumor sites in patients were the esophagus (n = 1671, 15.5%), lung (n = 1477, 13.7%), intestine (n = 1098, 10.1%), abdomen (n = 1018, 9.4%), uterus (n = 806, 7.5%), stomach (n = 761, 7.0%), and other sites as detailed in Table S4 in the electronic supplementary material. Non-sufentanil drugs, specifically buprenorphine (n = 807, 60.1%), fentanyl (n = 259, 19.3%), morphine (n = 123, 9.2%), dizocin (n = 79, 5.9%), and oxycodone (n = 74, 5.5%), are also shown in Table S2.
Multivariate analysis showed a number of variables associated with mild or moderate to severe pain, including age, gender, surgical mode, and surgical site as well as continuous volume of PCA infusion during both the first- and second 24 h (Table 2). The risk of moderate to severe pain (≥ 4/10) decreased slightly with increasing age (OR 0.986; 95% CI 0.975–0.996) during the first 24 h after surgery. Female patients consistently experienced higher risk of mild pain (OR 1.550; 95% CI 1.237–1.942) at the first and second 24 h after operation. Patients who underwent lumpectomy had higher risk of developing both mild pain (OR 1.384; 95% CI 1.106–1.730) and moderate to severe pain (OR 1.475; 95% CI 1.112–1.955) in the second 24 h. Surgical sites were related to pain risk, with the highest risk among the respiratory system (OR 2.043, 95% CI 1.370–3.046).
Moreover, we found that both high doses of continuous volume were widely related to 1–3-fold elevated pain risk. Patients with a continuous volume of 1.2–1.4 ml or > 1.6 ml had a higher risk of moderate to severe pain when referring to those with a continuous volume of ≤ 1.1 ml (1.2–1.4 ml: OR 1.555; 95% CI 1.120–2.160; > 1.6 ml: OR 2.453; 95% CI 1.742–3.456) in the first 24 h. Similar risk variation was noted for the second 24 h: patients with a continuous volume of 1.2–1.4 ml experienced a higher risk of mild pain than those with a continuous volume of ≤ 1.1 ml (OR 1.278; 95% CI 1.027–1.590). Patients with a continuous volume of 1.2–1.4 ml or > 1.6 ml had a higher risk of moderate to severe pain than patients with a continuous volume of ≤ 1.1 ml (1.2–1.4 ml: OR 1.512; 95% CI 1.079–2.120; > 1.6 ml: OR 1.941; 95% CI 1.382–2.726).
Similar to Table 2, multivariate analysis revealed a number of variables associated with mild or moderate to severe pain, including age, gender, surgical mode, surgical site, and total volume of infusions after operation (Table 3). We found consistently increased pain risk among the highest total volume of PCA infusion: the risk of mild pain was higher in patients with total infusions > 43 ml when referring to those with total infusions ≤ 27 ml (OR 1.404; 95% CI 1.064–1.853) in the first 24 h and the risk of mild pain was higher in patients with total infusions > 46 ml than in patients with total infusions ≤ 30 ml (OR 1.258; 95% CI 1.008–1.571) in the second 24 h; the risk of moderate to severe pain was higher in patients with total infusions > 43 ml when referring to those with total infusions ≤ 27 ml (OR 2.830; 95% CI 2.037–3.934) in the first 24 h and the risk of moderate to severe pain was higher in patients with total infusions > 46 ml than in patients with total infusions ≤ 30 ml (OR 3.024; 95% CI 2.199–4.159) in the second 24 h.
Table 4 shows the comparison of perioperative factors with the numbers of PCA pump compressions. Multivariate analyses were done to include only either continuous volume or total volume of infusion to avoid the presence of multicollinearity. A number of variables were associated with the numbers of PCA pump compressions, including age, weight, gender, surgical mode, surgical site, and continuous volume/total volume of infusion in the first and second 24 h. Although similar trends for associations were observed for many risk factors with numbers of compressions as they were associated with NRS, some varied associations did exist: in the multivariate analysis incorporating total volume of infusion, we could observe that increasing age gave a slightly elevated risk of inadequate analgesia (OR 1.006; 95% CI 1.002–1.011). The risk of inadequate analgesia was lower in female patients compared to male patients (OR 0.848; 95% CI 0.763–0.943). Patients undergoing lumpectomy had less inadequate analgesia than those undergoing non-lumpectomy procedures (OR 0.593; 95% CI 0.528–0.666). Patients with surgical sites in all other designated five systems experienced less inadequate analgesic compared with patients whose surgical site was the digestive system.
As for the association of numbers of PCA pump compressions with total/continuous volume of PCA infusion, a similar trend as for NRS was noted for dosage groups: patients in other groups of continuous volume had more inadequate analgesic compared to patients with ≤ 1.1 ml (1.2–1.4 ml: OR 1.369; 95% CI 1.210–1.550; 1.5–1.6 ml: OR 1.294; 95% CI 1.146–1.462; > 1.6 ml: OR 2.023; 95% CI 1.772–2.309) in the first 24 h while patients with a continuous volume of 1.2–1.4 ml or > 1.6 ml had a higher risk of inadequate analgesic than those with a continuous volume of ≤ 1.1 ml (1.2–1.4 ml: OR 1.329; 95% CI 1.160–1.523; > 1.6 ml: OR 1.346; 95% CI 1.164–1.556) in the second 24 h. Patients in other groups of total volume of infusion had more inadequate analgesic than patients with total volume of infusion ≤ 27 ml (28–34 ml: OR 1.809; 95% CI 1.592–2.056; 35–43 ml: OR 4.158; 95% CI 3.674–4.707; > 43 ml: OR 14.909; 95% CI 12.898–17.233) in the first 24 h. Patients in other total volume of infusion groups had more inadequate analgesic compared with patients with total volume of infusion ≤ 30 ml (31–37 ml: OR 1.373; 95% CI 1.157–1.629; 38–46 ml: OR 3.864; 95% CI 3.306–4.516; > 46 ml: OR 17.313; 95% CI 14.725–20.357) in the second 24 h.
The most frequent adverse event in the first 24 h postoperatively was uroschesis (n = 9138, 80.3%) and the least frequent event was pruritus (n = 12, 0.1%); this was also the case for the adverse events in the second 24 h after surgery (uroschesis: n = 9445, 83.0%; pruritus: n = 13, 0.1%). The details could be found in Table S3 in the electronic supplementary material.
Discussion
In this large retrospective study, we investigated the proportions of postoperative pain among patients with cancer and explored associated risk factors, with a special interest focusing on PCA infusion, both continuous volume and total volume. Several risk factors were observed to be related to postoperative cancer pain, among which intravenous PCA use after surgery, either continuous or total volume of infusions, was significantly associated with the occurrence and severity of postoperative pain both in the first and second 24 h postoperatively. To our knowledge, our present study is among the first to explore cancer pain and risk factors within 48 h after operation and summarize the variations between the first and second 24 h, both of which were the critical periods for analgesic management.
Exploring appropriate analgesic dose is always of great importance in the management of narcotic and psychotropic substances. Postoperative pain is acute pain that occurs immediately after surgery, lasting usually approximately 2–3 days. Then timely pain assessment of patients by healthcare professionals is an important part of effective postoperative pain management. Previous articles [10, 11] examining postoperative pain have involved observation of patients in the PACU for 48 h, assessing pain intensity at specified times, and using 48-h postoperative outcomes as the primary endpoint. There is evidence suggesting that opioid-containing anesthesia does not reduce postoperative pain [12]. Inadequate analgesia may negatively impact patient health on multiple levels: decreased quality of life, impaired sleep, harm to physical function, increased financial burden, and more [11]. Our study found postoperative pain even after high-dose medication treatment. Drugs require 4–5 half-lives to reach steady state, e.g., immediate-release opioids reach steady state in about 24 h, while extended-release opioids take about 2–3 days to reach steady state [13]. Comparative analysis of postoperative pain by days after operation is thus of great significance. We considered that during the first 24 h patients were still under the influence of intraoperative anesthesia while during the latter 24 h the anesthetic effect present in the first 24 h was eliminated so that it is feasible to observe the pain impact of PCA individually.
Postoperative pain and opioid needs may vary by more than tenfold between individuals, thus a fixed “one-size-fits-all” dosing schedule can be an underdose for some patients and an overdose for others [14]. PCA is an effective and safe method of administering anesthetics to the appropriate patient population [15], while it is also important to encourage patients to be treated with PCA only when necessary. Epidemiological studies have shown that a large number of patients appropriately given strong opioids for acute pain management fail to discontinue them for long periods of time [16]. From our results, we found that risk factors associated with moderate to severe pain were more significant, especially in the groups with 1.2–1.4 ml of continuous volume and 1.6 ml, both of which showed a higher risk than receiving ≤ 1.1 ml of continuous volume. The total volume of infusion showed a higher risk of moderate to severe pain only in the highest group (> 43 ml or > 46 ml). Although PCA is a safe and effective treatment for pain in patients with cancer, more prospective studies are needed to evaluate the safety and efficacy of this management strategy [6]. To better evaluate the pain effect, we used the number of intravenous PCA pump compressions performed by patients themselves and NRS evaluated by healthcare professionals in parallel. A high degree of consistency was found: the risk of inadequate analgesia occurring is significantly higher with high doses of continuous volume or total volume of infusion based on both ways of evaluating pain. Combining the NRS with the patient’s self-reported number of compressions better reflects the consistency of postoperative analgesic outcomes [17]. In addition to the Chinese study, other studies have also demonstrated that analgesic effect could be measured by pain scale, number of PCA uses, and medication consumption [18, 19].
Although our results were suggestive of insufficient pain control, we must consider the possibility of opioid-induced hyperalgesia (OIH), especially considering the established dose–response relationship for infusion volume and pain risk: the highest dosage incurred with the highest pain risk. A previous study found a significant increase in acute pain 24 h postoperatively after giving patients a high intraoperative dose of remifentanil, which also resulted in an increased need for morphine on postoperative day 1 [20]. Therefore, we suspected that the patients in this study had OIH. If hyperalgesia due to opioid medication occurs, it cannot be overcome by increasing its dose because this would actually exacerbate the hyperalgesia [21]. The mechanisms leading to the development of OIH are complex and controversial. Also, drug tolerance needs to be considered depending on the pharmacokinetic or pharmacodynamic changes [22]. When the opioid dose is increased, pain from tolerance usually improves. In contrast, for OIH, pain tends to worsen with increasing opioid doses. Therefore it is a challenging dilemma for the pain physician or clinician to differentiate between the two disorders of OIH and tolerance. Reducing opioid doses in order to reduce patients’ hyperalgesia can sometimes lead to mild withdrawal symptoms [23], and we will have to consider this in future long-term studies. However, what we have done in this study is to avoid opioids with short half-lives [24], reduce the dose of opioids, and focus on examining psychological and psychiatric factors in patients, which may reduce the occurrence of hyperalgesia.
Younger patients were reported to be more likely to be in the stable moderate to severe pain group [25]. Younger patients are biologically more sensitive to low-intensity noxious stimuli and may have higher central nervous system reactivity. Second, from a physiological perspective, older adults are more conservative in pain perception and reporting and are more reluctant to report pain when it occurs [26]. In our study, the effect of age as a determinant factor in patients’ pain risk when referring to the pain-free group was observed for both days after multiple adjustment, but the direction of influence seemed not decisive.
The surgical modes in our study were divided into lumpectomy and non-lumpectomy procedures, and in the original data lumpectomy procedures were overwhelmingly composed of laparoscopic and thoracoscopic procedures. The hypothesis that pain from some laparoscopic procedures is underestimated was reported in a prospective cohort study that included 50,523 patients [27], which was also supported by the findings in other reports [28, 29]. In our study on the second 24 h, patients who underwent lumpectomy surgery had a higher risk of pain than those who underwent non-lumpectomy surgery. We speculate that this could be partially due to the presence of intraoperative anesthesia in patients in the first 24 h. It is also possible that because lumpectomy has been shown to be a less painful procedure in previous studies or practice, there is laxity on the part of a few healthcare providers in the preoperative examination and postoperative care of patients, resulting in inflammation of the patient’s incision, etc.
In our study, the surgical site was systematically divided according to human anatomy. Patients with cancer undergoing respiratory surgery experienced more moderate to severe pain, whether in the first or second 24 h after surgery, whether for continuous or total volume of PCA infusion. Our results are supported by several studies in which some patients who underwent pulmonary lobectomy experienced higher levels of pain in the first 3 days postoperatively [10, 30]. However, there may also be another reason in that some of the surgeries were carried out using a thoracotomy or a thoracoscopy approach which constitutes the worst pain.
This study has some limitations: it is a retrospective study. Patients were not randomly assigned, and some risk characteristics such as medication classification, surgical mode, and surgical site may lead to uncontrolled bias. Other risk factors, such as psychological distress (anxiety, depression) and mental state, were not included in this analysis. There is also a lack of some preoperative pain information that limits the generalization of the results of this study. However, we believe the strength of our study lies in the large number of patients studied. The possible uneven distribution of pre-existing pain by covariables could at least partially have been alleviated by the large sample size of this study. Currently, most clinical studies on PCA use and postoperative pain have small sample sizes [9, 17, 19, 31], and the evidence supporting its use is thus limited. The present study benefited from a large sample, enabling stratification of important factors and adjustment for confounders as well. We collected raw data from the Rehn Medtech analgesic pump system, which has a mobile ward check function to understand the patient’s analgesic effect and to assess and record it in a timely manner. Moreover, both postoperative 24 h and postoperative 48 h are prime times for acute pain recovery, and pain is generally more pronounced in the first 24 h. Our study considered the second 24 h to exclude the effect of intraoperative anesthesia present in the first 24 h, so it is particularly important to extend the observation of pain to the second 24 h. Additionally, we used the NRS for pain scoring because of its clear classification, relative simplicity, ease of use, and greater ease of understanding and completion by subjects. We also used the number of analgesic pump compressions as an indicator for comparison with NRS.
Conclusion
Postoperative pain relief remains a major medical challenge. Our study found that younger age, lumpectomy, site of surgery being respiratory, and high continuous volume or total volume of infusion may be risk factors for the occurrence of moderate to severe pain. Furthermore, the study regarding either high continuous volume or high total volume of PCA infusion presented a high concordance of results between the risk of developing moderate to severe pain and associated risk factors. Our main findings may suggest the possibility of inadequate analgesia. Simultaneously, the possibility of OIH could not be ruled out, which warrants further study. Avoidance of opioids with short half-lives, reduction of opioid doses, and attention to examination of psychological and psychiatric factors in patients warrant more clinical attention.
References
McNicol ED, Ferguson MC, Hudcova J. Patient controlled opioid analgesia versus non-patient controlled opioid analgesia for postoperative pain. Cochrane Database Syst Rev. 2015(6):CD003348.
Zejun N, Wei F, Lin L, He D, Haichen C. Improvement of recovery parameters using patient-controlled epidural analgesia for video-assisted thoracoscopic surgery lobectomy in enhanced recovery after surgery: a prospective, randomized single center study. Thorac Cancer. 2018;9(9):1174–9.
Grass JA. Patient-controlled analgesia. Anesth Analg. 2005;101(5 Suppl):S44–61.
Shin S, Min KT, Shin YS, Joo HM, Yoo YC. Finding the ‘ideal’ regimen for fentanyl-based intravenous patient-controlled analgesia: how to give and what to mix? Yonsei Med J. 2014;55(3):800–6.
Chen W, Zheng R, Baade PD, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Nijland L, Schmidt P, Frosch M, et al. Subcutaneous or intravenous opioid administration by patient-controlled analgesia in cancer pain: a systematic literature review. Support Care Cancer. 2019;27(1):33–42.
KorkmazskyM, Ghandehari J, Sanchez A, Lin H-M, Pappagallo M. Feasibility study of rapid opioid rotation and titration. Pain Physician. 2011;14(1):71–82.
Chen L, Wu Y, Cai Y, et al. Comparison of programmed intermittent bolus infusion and continuous infusion for postoperative patient-controlled analgesia with thoracic paravertebral block catheter: a randomized, double-blind, controlled trial. Reg Anesth Pain Med. 2019;44(2):240–5.
Lin R, Lin S, Feng S, et al. Comparing patient-controlled analgesia versus non-PCA hydromorphone titration for severe cancer pain: a randomized phase III trial. J Natl Compr Canc Netw. 2021;19:1–8. https://doi.org/10.6004/jnccn.2020.7699.
Wang L, Liu D, Lu J, Zhang S, Yang X. The feasibility and advantage of uniportal video-assisted thoracoscopic surgery (VATS) in pulmonary lobectomy. BMC Cancer. 2017;17(1):75.
Sinatra R. Causes and consequences of inadequate management of acute pain. Pain Med. 2010;11(12):1859–71.
Frauenknecht J, Kirkham KR, Jacot-Guillarmod A, Albrecht E. Analgesic impact of intra-operative opioids vs. opioid-free anaesthesia: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):651–62.
Scarborough BM, Smith CB. Optimal pain management for patients with cancer in the modern era. CA Cancer J Clin. 2018;68(3):182–96.
Abrolat M, Eberhart LHJ, Kalmus G, Koch T, Nardi-Hiebl S. Patient-controlled analgesia (PCA): an overview about methods, handling and new modalities. Anasthesiol Intensivmed Notfallmed Schmerzther. 2018;53(4):270–80.
Mitra S, Carlyle D, Kodumudi G, Kodumudi V, Vadivelu N. New advances in acute postoperative pain management. Curr Pain Headache Rep. 2018;22(5):35.
Alam A, Gomes T, Zheng H, Mamdani MM, Juurlink DN, Bell CM. Long-term analgesic use after low-risk surgery: a retrospective cohort study. Arch Intern Med. 2012;172(5):425–30.
Xu J, Pu M, Xu X, Xiang J, Rong X. The postoperative analgesic effect of intercostal nerve block and intravenous patient-controlled analgesia on patients undergoing lung cancer surgery. Am J Transl Res. 2021;13(8):9790–5.
Andziak M, Beta J, Barwijuk M, Issat T, Jakimiuk AJ. Efficacy and tolerability of intravenous morphine patient-controlled analgesia (PCA) in women undergoing cesarean delivery. Ginekol Pol. 2015;86(6):453–6.
Aydin ON, Kir E, Ozkan SB, Gursoy F. Patient-controlled analgesia and sedation with fentanyl in phacoemulsification under topical anesthesia. J Cataract Refract Surg. 2002;28(11):1968–72.
Fletcher D, Martinez V. Opioid-induced hyperalgesia in patients after surgery: a systematic review and a meta-analysis. Br J Anaesth. 2014;112(6):991–1004.
Yu EH, Tran DH, Lam SW, Irwin MG. Remifentanil tolerance and hyperalgesia: short-term gain, long-term pain? Anaesthesia. 2016;71(11):1347–62.
Mercadante S, Arcuri E, Santoni A. Opioid-induced tolerance and hyperalgesia. CNS Drugs. 2019;33(10):943–55.
Yi P, Pryzbylkowski P. Opioid induced hyperalgesia. Pain Med. 2015;16(Suppl 1):S32-36.
Mamie C. Prevention of postoperative hyperalgesia. Ann Fr Anesth Reanim. 2012;31(1):e39-42.
Vasilopoulos T, Wardhan R, Rashidi P, et al. Patient and procedural determinants of postoperative pain trajectories. Anesthesiology. 2021;134(3):421–34.
Zhang Y, Zhou R, Hou B, et al. Incidence and risk factors for chronic postsurgical pain following video-assisted thoracoscopic surgery: a retrospective study. BMC Surg. 2022;22(1):76.
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–44.
Iamaroon A, Tangwiwat S, Nivatpumin P, Lertwacha T, Rungmongkolsab P, Pangthipampai P. Risk factors for moderate to severe pain during the first 24 hours after laparoscopic bariatric surgery while receiving intravenous patient-controlled analgesia. Anesthesiol Res Pract. 2019;2019:6593736.
Lindberg M, Franklin O, Svensson J, Franklin KA. Postoperative pain after colorectal surgery. Int J Colorectal Dis. 2020;35(7):1265–72.
Liu Z, Yang R, Shao F. Comparison of postoperative pain and recovery between single-port and two-port thoracoscopic lobectomy for lung cancer. Thorac Cardiovasc Surg. 2019;67(02):142–6.
Luan H, Zhang X, Feng J, Zhu P, Li J, Zhao Z. Effect of dexmedetomidine added to ropivacaine on ultrasound-guided transversus abdominis plane block for postoperative analgesia after abdominal hysterectomy surgery: a prospective randomized controlled trial. Minerva Anestesiol. 2016;82(9):981–8.
Acknowledgements
The corresponding author would like to thank all the co-workers for collecting, managing, and maintaining the data used in this analysis. We also appreciate funders for providing the financial support to conduct the present study.
Funding
This study was jointly funded by the Social development-Clinical Frontier Technology Project of China Jiangsu Provincial Department of Science and Technology (BE2018669); the Health Research Funds of Nantong, China (2020JCC046); General program from Nantong Commission of Health (MB2021050); Scientific Research Foundation for Talented Scholars in Soochow University, China; Suzhou medical and industrial integration collaborative innovation research project (Project number SLJ202012); Suzhou clinical trial institution capacity enhancement project (Project number SLT202003); The Nuclear Energy Development Project, China (Project number 2016-1295); and A Project of the Priority Academic Program Development of Jiangsu Higher Education Institutions China. The Rapid Service Fee was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work, and have given their approval for this version to be published.
Author Contributions
Conception and design: Xiaohong Chen, Jiazhen Yao, Xiaochen Shu, and Hanzhong Cao. Financial support: Xiaochen Shu and Hanzhong Cao. Provision of study materials or patients: Xiaohong Chen, Genshan Ma, Yan Yu, Yuan Yang, and Hanzhong Cao. Collection and assembly of data: Jiazhen Yao, Yirong Xin, Genshan Ma, Yan Yu, and Yuan Yang. Data analysis and interpretation: Jiazhen Yao, Yirong Xin, and Xiaochen Shu. Manuscript drafting: Xiaohong Chen, Jiazhen Yao, Yirong Xin, Genshan Ma, Yan Yu, Yuan Yang, Xiaochen Shu, and Hanzhong Cao. Final approval of manuscript: Xiaohong Chen, Jiazhen Yao, Yirong Xin, Genshan Ma, Yan Yu, Yuan Yang, Xiaochen Shu, and Hanzhong Cao.
Disclosures
Xiaohong Chen, Jiazhen Yao, Yirong Xin, Genshan Ma, Yan Yu, Yuan Yang, Xiaochen Shu and Hanzhong Cao declare that they have no conflict of interest.
Compliance with Ethics Guidelines
Our research protocols were approved by the institutional review boards of Nantong Tumor Hospital (IRB2018-010). For the safety and rationality of the research, we signed the informed consent for all the participants. The implementation of the current study adhered to the tenets of the Declaration of Helsinki of the World Medical Association with regard to scientific research on human subjects. In order to preserve anonymity, individual records of all participants were de-identified before the analysis.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Chen, X., Yao, J., Xin, Y. et al. Postoperative Pain in Patients Undergoing Cancer Surgery and Intravenous Patient-Controlled Analgesia Use: The First and Second 24 h Experiences. Pain Ther 12, 275–292 (2023). https://doi.org/10.1007/s40122-022-00459-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00459-w