Abstract
Introduction
This study aimed to investigate the effects of progressive postural control exercise (PPCE) vs core stability exercise (CSE) in patients with chronic low back pain (CLBP).
Methods
A total of 34 young-adult participants with CLBP were randomly assigned to two groups (the PPCE group and the CSE group). They received instructions for two different exercise training regimens persisting over 8 weeks. Before, after, and at 6 months after the intervention, the participants were evaluated on the basis of pain intensity (VAS), degree of dysfunction (ODI and RMDQ), contractility of transversus abdominis (TrA) and lumbar multifidus (MF), as well as the ability to control static posture.
Results
There was no significant difference between the results of the PPCE group and the CSE group. At the 6-month follow-up after the 8-week treatment, the scores of VAS, ODI, and RMDQ in the two groups decreased significantly compared to before (p < 0.05). The percentage change in thickness of bilateral TrA and left MF (p < 0.05) was elevated and the sway area of center of pressure during static stance tasks with eyes opened (p < 0.05) was decreased in both groups.
Conclusion
In the short term, PPCE provides positive effects similar to those of core stability exercise in patients with CLBP. The effective mechanism of PPCE might be the consequence of neuromuscular plasticity and adaptation adjustments. PPCE enriches the choices of treatment for CLBP.
Clinical Trial Registration
The trial was registered at www.chictr.org.cn, identifier ChiCTR2100043113.
Plain Language Summary
Chronic low back pain (CLBP) is a widespread disorder with highly recurrent prevalence. As of now, the treatment effects are not satisfactory, leading to a search for novel therapies that might work better in patients with CLBP. This study comprehensively explored the effects of progressive postural control exercise, as compared to core stability exercise, on patients with CLBP. The outcomes included pain intensity, disability of daily life, contractility of trunk muscles, and postural control. The results of the study showed that the efficacy of exercises in patients in the experimental group was similar to that of the control group and both exercise treatments improved the pain intensity, the disability, the contractile function of trunk muscle, as well as postural control in patients with CLBP in the short term. The mechanism of the effects of progressive postural control exercise might be the consequence of “neuromuscular plasticity” and adaptation adjustments.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
CLBP is a multifactorial disorder with a high morbidity. The treatment effects of CLBP, as of now, are not satisfactory. |
PPCE is a novel exercise treatment that includes motor control exercise and resistance training. |
PPCE was supposed to have better effects in patients with CLBP than the standard exercise strategy. This study aimed to explore the effects of PPCE comprehensively. |
What was learned from the study? |
On the basis of the findings of this study, we concluded that PPCE has positive short-term effects on patients with CLBP but with few obvious advantages over CSE. |
PPCE can improve pain intensity and disability, contractility of trunk muscle, as well as postural control in patients with CLBP. |
PPCE, as a novel treatment, enriches the treatment choices in patients with CLBP. |
Introduction
Low back pain (LBP) is a common multifactorial disorder around the world [1]. Among the patients with LBP, chronic LBP (CLBP) is the highest incidence rate [2]. The lifetime prevalence of LBP was reported to be as high as 84% and that of CLBP was about 23% [3]. CLBP brings huge burdens to patients with unsatisfactory effects of treatments [2, 4]. Although there has been some progress in the assessment and treatment of this disorder in recent years, obtaining satisfactory effects of treatment for CLBP remains a challenge for researchers and clinicians [5, 6].
According to the latest US Department of Veterans Affairs and US Department of Defense (VA/DoD) clinical practice guideline for LBP, supervised exercise has been noted as a favored and recommended method of conservative therapeutic programs by researchers [5]. Medical evidence of moderate certainty shows that exercise could be an effective treatment for patients with CLBP as compared to groups given no treatment, usual care, or placebo for pain [7]. It was also found to have improved pain and functional limitations outcomes via core stability exercises (CSE) or general exercises [7]. Reports have also shown that CSE can improve the activity of deep abdominal muscles and elevated postural control in patients with CLBP [8, 9]. As compared to general exercise, CSE is more effective in reducing pain and improving physical function in patients with CLBP in the short term [10]. However, CSE has some limitations. The long-term effects of CSE on patients with CLBP are still controversial. No significant long-term differences in pain were observed between CSE and general exercise [10], although there is not much medical evidence for these treatment options. It is unclear as to which exercise program provides better and longer effects in patients with CLBP [11, 12]. A report by Lederman suggested that CSE had no better effects than other forms of manual or physical therapy or general exercise [13]. Therefore, it is necessary to identify and popularize a universally adaptive and effective training program for CLBP.
Progressive postural control exercise (PPCE) is a novel strategy for patients with CLBP. It originates from motor control exercise and resistance training with a theme of challenging postural control with phased progression. Searle et al. suggested that a beneficial effect for strength or resistance and coordination or stability exercise programs over other interventions be used in the treatment of CLBP [14]. Motor control exercises were also reported to produce slightly better short-term function and perceptions of an effect than general exercise in patients with chronic non-specific back pain [15]. The progression of the training load was suggested to improve postural control in young individuals as it was better on neuromuscular plasticity than general exercise [16]. Progressive resistance training also has multiple positive effects on postural control and gait in patients with Parkinson’s disease [17], as well as in improved balance and walking speed in patients with chronic stroke [18]. On the basis of these studies [12, 17, 19], PPCE is supposed to have positive effects on patients with CLBP.
The morphology of the trunk muscle and postural control as well as pain intensity and daily function are commonly used to evaluate the efficacy of treatment in patients with CLBP. In 1992, Panjabi proposed the neutral zone and instability hypothesis [20]. He argued that weakness of muscles might result in spinal instability or a low-back problem. Among the trunk muscles, the deep muscles, such as transversus abdominis (TrA) and lumbar multifidus (MF), were suggested to play important roles in core stability [21]. Structural changes of TrA and MF were typically used to assess the effects of the treatment on patients with CLBP [22]. Postural control is a series of neuromuscular control activities to achieve spatial positioning of the limbs [23]. The postural control system is a complex process involving proprioception, visual, and vestibular senses [24, 25]. Previous studies suggested that patients with CLBP had impaired postural control under various conditions, such as standing on an unstable support surface or with visual deprivation [25, 26]. Further, researchers tended to study the function of trunk muscles and postural control to explore the mechanism of LBP [27]. Exercise therapy can also improve the contractility of muscles and postural control [28, 29].
This study sought to investigate the effects of PPCE on patients with CLBP by comparing PPCE with traditional CSE using pain intensity, disability, morphology of trunk muscle, and postural control at different time points as indicators.
Methods
Study Design and Randomization
This was a randomized controlled trial (RCT) with single-blinded parallel groups of young-adult patients with CLBP. The examiners and the physiotherapists in the study, except for the experimental designer, were blinded to the participants. The participants in either group were also blinded to the intervention given to the other group. Ethical approval was obtained and the trial is registered at ChiCTR 2100043113.
Participants
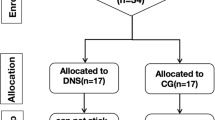
Participants had been recruited through advertisements on a social platform and outpatient service. The study began on July 1, 2020 and ended on June 30, 2021. The inclusion criteria for the CLBP participants were as follows: (1) medical diagnosis of non-specific LBP with pain and symptoms persisting for more than 3 months and (2) visual analog scale (VAS) > 3 cm; (3) patients aged between 18 and 40 years; (4) patients with non-specific CLBP; (5) no history of lumbar disc herniation or trauma. Participants were excluded if they had any of the following: (1) pregnant; (2) chronic LBP of traumatic or structural origin or LBP with neurological symptoms or pain radiation in the lower leg(s); (3) previous back surgery, spinal tumors or infections, or neurological and/or musculoskeletal disorders unrelated to LBP like stroke, Parkinson’s disease, demyelination, multiple sclerosis, and so on [30]. The diagnosis of CLBP was based on the diagnostic guidelines published by the American College of Physicians and the American Pain Society [31]. The details of the recruiting process are illustrated in Fig. 1.
Interventions
A total of 34 participants (10 male, 24 female) were enrolled and divided randomly into two groups of 17. The individuals in the PPCE group were treated with the strategy of an 8-week progressive postural control exercise, while those in the CSE group underwent an 8-week intervention with core stability exercise. If the participants did not accomplish the treatment or finish the 6-month follow-up, they would be treated as dropouts. Every participant should provide written consent before data collection.
Progressive Postural Control Exercise
PPCE consisted of three stages:
-
1.
In the first stage, participants were mainly trained with their core muscles against gravity on a stable platform. The exercise program consisted of six movements: pelvic retroversion, crunches, glute bridge, bird-dog, bear crawl, and contralateral arm lifting. The first stage persisted for 2 weeks.
-
2.
In the second stage, they were mainly trained with the trunk muscle against gravity and a Swiss ball for training on an unstable surface. This stage persisted for 3 weeks.
-
3.
In the third stage, the movements of the exercise performed with the help of a Swiss ball and a stretch band or a 5-kg sandbag helped train them on an unstable and less supporting surface with resistance training. The third stage persisted for 3 weeks. Each stage consisted of six movements each persisting for about 5 min and performed for 30 min. Each movement of PPCE is illustrated in Fig. 2.
Core Stability Exercise
The participants in the CSE group were instructed to receive the intervention of a classic core stability exercise program. Core stability exercise consists of the prone-plank, single leg-bridge, side-plank, double leg-bridge, and bird-dog [16]. The exercise program was also performed over 8 weeks, three times a week, with each session lasting 30 min [32]. The movements of CSE in this study are shown in Fig. 3.
Measurements and Outcomes
Evaluation of Pain Intensity and Disability of Daily Life
To understand the pain intensity and daily function of the patients, participants in the two groups were instructed to complete a Visual Analogue Scale (VAS), Oswestry Disability Index (ODI), and Roland Morris Disability Questionnaire (RMDQ) before and after the treatments as well as 6 months after the treatments. VAS was applied to measure the self-reported pain intensity of the patients which requires the participants to place a marker on a 10-cm-long straight line with stops at each end; the left stop indicated no pain while the right stop indicated the worst pain imaginable [33].
The function of the daily life of the patients with CLBP was evaluated with the questionnaires, ODI [34] and RMDQ [35]. The ODI covered activities of daily living that might be disrupted by low back pain [36]. This included 10 items: one item on pain and nine items on activities of daily living. Each item was measured on a six-point ordinal scale, ranging from the best scenario to the worst scenario. The reliability and validity of this study have already been established [34]. ODI was considered an appropriate instrument for assessing chronic back pain-related disability in Chinese patients.
RMDQ was a short and simple self-rated assessment of physical function in patients with back pain with the advantage of ease of use, making it suitable for follow-ups on the progress of individual patients in clinical settings. RMDQ was different from ODI in some content [36, 37]. Participants were asked to check the statements that represented their status on that day. Each statement was awarded one point if checked, giving a score out of 24.
Assessment of Thickness and Contractility of Transversus Abdominis and Lumbar Multifidus
Musculoskeletal ultrasound was used to measure the morphologic changes of the transversus abdominis (TrA) and lumbar multifidus (MF) of the participants. Ultrasound imaging was reliable and reproducible for the evaluation of muscle structure, function, and activity [38]. In the present study, the examination device was a rehabilitative ultrasound (SONIMAGE HS1, Konica Minolta Inc., Japan) with a linear transducer at 18.0 MHz for TrA and a curvilinear transducer at 4.0 MHz for MF.
The method of TrA examination was as follows: instruct the participants to lie supine with arms crossed over the chest, hips flexed to 50°, and knees flexed to 90° so that the abdomen was relaxed and fully exposed. The linear transducer (L18-4) with B-mode was placed at the intersection between the level of the umbilicus and the axillary front on one side. The parameter recorded during the period where the participant relaxed was the thickness at rest state and was repeated three times. Then, three repetitions of the abdominal draw-in maneuver (ADIM) were performed and assigned as the maximum voluntary isometric contraction (MVIC) state [39]. The same method was used to measure the other side of TrA.
The methods of MF examination are as follows: the participant adopts the prone position and puts the head (relaxed) in the hole of the physical therapy bed. An inclinometer was placed longitudinally over the lumbo/sacral junction and pillows were used to flatten the lumbar curve to less than 10°. The curvilinear transducer (C5-2) with B-mode was placed longitudinally along the spine with the mid-point over the L4 spinous process. It was moved laterally and angled slightly medially until the L4/5 zygapophyseal joint could be identified. This scan point is directly over the MF and measurement from this landmark to the plane between the muscle and subcutaneous tissue was used for the linear measurement of the LM at rest, and the thickness recorded during the contralateral arm lifting tasks was performed in the same plane as the MVICs. Every state of each side of the MF was repeated three times.
Considering differences in gender, body weight, height, and age, the percentages of changes in average muscle thickness from three measurements underwent statistical analysis. The percentage change in muscle thickness was calculated as follows [40]:
Postural Control Measurements
Before and after the treatments, each participant was asked to do four static stance tasks to test their postural control ability. The balancing instrument applied in the present study was PRO-KIN Version, PK252P, TecnoBody, made in Italy. These testing tasks consisted of stance with eyes opened (EO), stance with eyes closed, right single leg stance (RSL), and left single leg stance (LSL). These tasks were as follows:
-
(a)
Static stance with eyes opened task (EO): Participants were instructed to stand up straight on a stable pressure plate with bare feet with their hands placed vertically at each side of the body. After a signal from the examiner, the participants were instructed to keep the posture static for 30 s with their eyes looking forward horizontally.
-
(b)
Static stance with eyes closed task (EC): This task was similar to the EO task but the participants were asked to keep their eyes closed while standing.
-
(c)
Right single leg stance task (RSL): Participants were instructed to stand up straight on a stable pressure plate with bare feet with their hands placed vertically at each side of the body. After a signal, participants lift their left leg with the knee flexion at 90° and had the right foot standing up straight on the pressure plate, and persisted for 30 s with the eyes looking forward horizontally.
-
(d)
Left single leg stance task (LSL): This task was similar to the RSL task, except for the participants being asked to change the supporting foot to the left with a right leg lift.
After resting for 2 min, the participants were instructed to repeat the measurements three times. The mean values of the three measurements were included in the statistics. The displacement area of the center of pressure (COP), average displacement velocity of COP on the X-axis, and average displacement velocity of COP on the Y-axis were recorded as the statistical parameters.
Sample Size Calculation
The sample size calculation was based on the results of the primary outcome of VAS. A difference of an average of 3.00 points in the score was considered clinically significant. The sample size was determined using the G*Power 3.1 version with α = 0.05 (two-sided) and (1 − β) = 0.8, with an effect size of 0.4. The total sample size was 34 patients.
Statistical Analysis
All the parameters were performed by statistical analysis by SPSS version 26.0 (IBM Statistics, New York, USA). Continuous data are presented as the mean ± standard according to normal distribution. The Kolmogorov–Smirnov test was used to determine the normality of the data. When the variables fit a normal curve, independent samples t tests were used to compare the continuous variables between groups, and the chi-square test was used to compare in terms of sex and presented as a number (proportion). One-way repeated measures analysis of variance (ANOVA) was applied to analyze differences in the interaction effects between groups and time points. When the variables did not fit a normal curve, the Mann–Whitney U test and the Kruskal–Wallis test were used for the analysis between groups and time points. p < 0.05 indicated statistical significance.
Results
Basic Characteristics of Participants
Thirty-four participants with CLBP, aged 18 to 40 years (10 male and 24 female) voluntarily participated in the study. The distribution of sex, age, height, weight, BMI, and pain duration of the participants in the PPCE group was similar to the CSE group. At baseline, the demographic and clinical characteristics of participants between the PPCE group and the CSE group showed no significant difference (p > 0.05). The results of the data were illustrated in Table 1.
Primary Outcome
Scores of VAS, ODI, and RMDQ Decreased After PPCE
The scores of the pain intensity and disability of daily life decreased after 8-week interventions.
VAS
As shown in Fig. 4a, a comparison of the scores of VAS between the groups found no difference at the three time points (p > 0.05). Compared to baseline (PPCE group, 5.45 ± 1.19; CSE group 5.02 ± 1.13), the scores of VAS in the two groups reduced significantly after the 8-week treatments (PPCE group, 2.18 ± 1.96; CSE group 1.82 ± 1.54) (p < 0.01). Six months after the interventions, the score of VAS persisted (PPCE group, 3.18 ± 1.78; CSE group 2.59 ± 1.91) (p < 0.01) with a significant difference to the scores at baseline (p < 0.01).
Scores of VAS, ODI, and RMDQ at three different time points. No significant difference appeared in the groups. PPCE progressive postural control exercise, CSE core stability exercise. *Compared to the scores before treatments, PPCE group, p < 0.05; #Compared to the scores before treatments, CSE group, p < 0.05; **, ##, p < 0.01
ODI
As shown in Fig. 4b, a comparison of the scores of ODI between the groups found no difference at the three time points (p > 0.05). The scores of ODI decreased significantly in the CSE group after treatments (p < 0.05) but not significantly in the PPCE group (p = 0.054). The mean values of ODI at baseline were 7.12 ± 3.10 in the PPCE group and 8.47 ± 3.81 in the CSE group; after 8-week treatments, the scores were 4.71 ± 2.78 in the PPCE group (p < 0.01) and 3.53 ± 2.55 in the CSE group; and at the 6-month follow-up, the scores of ODI (5.06 ± 2.28 in the PPCE group; 5.06 ± 3.83 in the CSE group) showed significant difference from baseline (p < 0.05).
RMDQ
As shown in Fig. 4c, a comparison of the scores of RMDQ between the groups found no difference at the three time points (p > 0.05). The scores in each group significantly reduced from baseline (PPCE group, 4.41 ± 3.20; CSE group 2.88 ± 2.29) to 8 weeks after treatment (PPCE group, 2.21 ± 2.87; CSE group 1.18 ± 1.45) (p < 0.05). At the 6-month follow-up (PPCE group, 2.24 ± 1.99; CSE group 2.41 ± 2.81), the scores of RMDQ in the PPCE group persisted (vs after treatment, p > 0.05).
Secondary Outcomes
Thickness and Contractility of TrA and MF Changed After Interventions
The thickness of TrA and MF was measured in all but one participant, who missed the examination because of personal reasons. Data from 33 participants were then used for analysis (17 in PPCE, 16 in CSE).
As shown in Fig. 5, the time effects of R-TrA at MVIC, R-TrA change %, L-TrA at MVIC, L-TrA change %, and L-MF change % were significant (p < 0.05). The contractility of bilateral TrA (before treatment, R 70.19 ± 30.64, L 80.93 ± 27.08 in the PPCE group; R 62.56 ± 27.08, L 85.80 ± 37.71 in the CSE group) and left MF (34.32 ± 12.22 in the PPCE group; 30.00 ± 11.72 in the CSE group) improved after the interventions (after treatment, R-TrA 93.40 ± 32.21, L-TrA 108.64 ± 34.90, L-MF 39.00 ± 11.92, in the PPCE group; R-TrA 102.29 ± 45.54, L-TrA 93.41 ± 38.84, L-MF 35.53 ± 15.22, in the CSE group) (p < 0.05). No significant difference appeared between groups and time groups of all the variables of TrA and MF (p > 0.05).
Thickness of the trunk muscles at different states and the percentage change of TrA or MF before and after the interventions. No significant difference appeared between the groups (p > 0.05). PPCE progressive postural control exercise, CSE core stability exercise, TrA transversus abdominis, MF multifidus. *Compared to the scores before treatment in the PPCE group, p < 0.05; #Compared to the scores before treatment in the CSE group, p < 0.05; ** and ## mean p < 0.01
Postural Control Changed During Static Stance Tasks
As shown in Fig. 6, the sway area of COP decreased after the interventions during the four static stance tasks. The time effects of the sway area of COP during EO, RSL, and LSL tasks were significant (p < 0.05). During the EC task, the time effect of the sway area was not significant (p = 0.317). However, there was no significant difference between the groups and time groups of all the variables in these four stance tasks (p > 0.05).
Sway area of COP changed during different static stance tasks after the interventions. *Compared to the scores before treatment in the PPCE group, p < 0.05; #Compared to the scores before treatment in the CSE group. PPCE progressive postural control exercise, CSE core stability exercise. No significant difference appeared between the groups (p > 0.05)
Discussion
The present study aimed to comprehensively evaluate the effects of 8-week PPCE vs 8-week CSE on patients with CLBP. The results showed that both these interventions improved the pain intensity and disability of CLBP in the short term. Further, PPCE and CSE enhanced the contractility of deep trunk muscles and elevated postural control in patients with CLBP.
In this study, PPCE presented effects similar to CSE in pain reduction and disability improvement. CSE was also reported to reduce pain intensity and disability in patients with CLBP in the short term. Kim and Yim examined the effects of CSE and hip muscle stretching exercises on physical function (i.e., pain, instability, hip muscle flexibility) and activity (i.e. disability, balance, quality of life) in patients with CLBP [9]. In our study, the significant reductions of VAS, ODI, and RMDQ in the CSE group after the intervention are consistent with previous studies on core stability exercise [9]. The effects persist in the short term for 6 months (Fig. 4).
On the other hand, researchers tended to study the function of trunk muscles and postural control in order to evaluate the effects of treatments on patients with CLBP [27]. We found that PPCE enhanced the contractility of TrA and MF. In this study, the percentage change of bilateral TrA and left MF increased in the PPCE group. The improvement of these deep trunk muscles should have a positive effect on core stability [41]. Core stability was supposed to be an important factor in causing LBP [13]. Previous studies demonstrated a change in the onset timing of the trunk muscles in back injury and patients with CLBP [42] leading to impaired postural control [43]. Abnormal recruitment patterns of trunk muscles have also been reported to appear in patients with CLBP [44]. These studies suggest a correlation between the function of trunk muscles in patients with CLBP and impaired postural control [45]. This effective mechanism might be the consequence of “neuromuscular plasticity” and adaptation adjustments. In this study, the percentage change of right MF did not change significantly after the treatments compared to before as a result of the right-handed lifestyle of the volunteers. The right multifidus muscle has decreased its plasticity with years of favorable handed lifestyle. Patients with CLBP have also been reported to exhibit a higher asymmetry for trunk muscle activity in some functional tasks [46, 47], affecting the effect of exercise therapy on these participants. Another explanation might be a bias of samples.
Postural control is important in our daily life [24]. Concerning the role of the neuromuscular control system, an increased body sway has been found in patients with low back pain, indicating a less efficient muscle control system with a decreased ability to provide the needed spinal stability [48]. Static stance tasks were usually applied to evaluate the postural control in patients with CLBP [49]. Sway area is one of the most common parameters for presenting the displacement of COP. The smaller the area is, the less the body sways. In this study, the sway area of COP decreased during EO, RSL, and LSL tasks after the exercise treatments. These results indicated that both PPCE and CSE enhanced the ability of static postural control in patients with CLBP. A comparison of the results under these four different conditions revealed that these balance enhancements during the eyes open task and single leg stance tasks were possibly attributed to improvements in the motor control of the deep trunk muscles and adaptation adjustments; the conclusions were also consistent with those of Page et al. [28]. However, no significant improvements in the sway area happened during the EC task, suggesting that there is a limited effect of PPCE on proprioception without vision. Further studies are needed to elucidate the therapeutic mechanism of PPCE.
Limitations
This study contains serval limitations. Firstly, the sample size is small such that the SD values of the parameters might be too large to find a significant difference between the two groups. Secondly, the recruiting methods could be associated with a selection bias. Since the participants included in the study are young adults with nonspecific CLBP, it does not represent aging patients. PPCE treatment requires relatively high strength and might hurt old patients, which needs further studies. Thirdly, the effects of the interventions were evaluated only up to 6 months in this study. There is also a lack of evaluation of long-term effects. Future studies should conduct a long-term follow-up test to understand how the patients maintain exercise programs and how the effects persist. This could provide medical evidence for training in the treatment of CLBP.
Conclusion
PPCE has positive short-term effects on patients with CLBP which were similar to those of CSE. PPCE improves pain intensity and disability of the patients, enhances the contractility of TrA and MF, and elevates postural control ability. The mechanism of the effects of PPCE is complicated and might be the consequence of “neuromuscular plasticity” and adaptation adjustments. However, PPCE as a novel exercise strategy for CLBP enriches the choices of treatments for clinicians. Future research should focus on the long-term effects of PPCE on patients with CLBP.
References
Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–602.
Vlaeyen JWS, Maher CG, Wiech K, et al. Low back pain. Nat Rev Dis Primers. 2018;4(1):52.
Balagué F, Mannion AF, Pellisé F, Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482–91.
Cohen SP, Vase L, Hooten WM. Chronic pain: an update on burden, best practices, and new advances. Lancet. 2021;397(10289):2082–97.
Pangarkar SS, Kang DG, Sandbrink F, et al. VA/DoD clinical practice guideline: diagnosis and treatment of low back pain. J Gen Intern Med. 2019;34(11):2620–9.
Qaseem A, Wilt TJ, McLean RM, Forciea MA, et al. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2017;166(7):514–30.
Hayden JA, Ellis J, Ogilvie R, Malmivaara A, van Tulder MW. Exercise therapy for chronic low back pain. Cochrane Database Syst Rev. 2021;9:CD009790.
Hwangbo G, Lee CW, Kim SG, Kim HS. The effects of trunk stability exercise and a combined exercise program on pain, flexibility, and static balance in chronic low back pain patients. J Phys Ther Sci. 2015;27(4):1153–5.
Kim B, Yim J. Core stability and hip exercises improve physical function and activity in patients with non-specific low back pain: a randomized controlled trial. Tohoku J Exp Med. 2020;251(3):193–206.
Wang XQ, Zheng JJ, Yu ZW, et al. A meta-analysis of core stability exercise versus general exercise for chronic low back pain. PLoS ONE. 2012;7(12):e52082.
Sipaviciene S, Kliziene I. Effect of different exercise programs on non-specific chronic low back pain and disability in people who perform sedentary work. Clin Biomech (Bristol, Avon). 2020;73:17–27.
Hayden JA, Ellis J, Ogilvie R, et al. Some types of exercise are more effective than others in people with chronic low back pain: a network meta-analysis. J Physiother. 2021;67(4):252–62.
Lederman E. The myth of core stability. J Bodyw Mov Ther. 2010;14(1):84–98.
Searle A, Spink M, Ho A, Chuter V. Exercise interventions for the treatment of chronic low back pain: a systematic review and meta-analysis of randomised controlled trials. Clin Rehabil. 2015;29(12):1155–67.
Ferreira ML, Ferreira PH, Latimer J, et al. Comparison of general exercise, motor control exercise and spinal manipulative therapy for chronic low back pain: a randomized trial. Pain. 2007;131(1–2):31–7.
Vera-Garcia FJ, Irles-Vidal B, Prat-Luri A, Garcia-Vaquero MP, Barbado D, Juan-Recio C. Progressions of core stabilization exercises based on postural control challenge assessment. Eur J Appl Physiol. 2020;120(3):567–77.
Santos L, Fernandez-Rio J, Winge K, et al. Effects of progressive resistance exercise in akinetic-rigid Parkinson’s disease patients: a randomized controlled trial. Eur J Phys Rehabil Med. 2017;53(5):651–63.
Vahlberg B, Cederholm T, Lindmark B, Zetterberg L, Hellstrom K. Short-term and long-term effects of a progressive resistance and balance exercise program in individuals with chronic stroke: a randomized controlled trial. Disabil Rehabil. 2017;39(16):1615–22.
Gabriel DA, Kamen G, Frost G. Neural adaptations to resistive exercise: mechanisms and recommendations for training practices. Sports Med. 2006;36(2):133–49.
Panjabi M. The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord. 1992;5(4):390–6 (discussion 7).
Goubert D, De Pauw R, Meeus M, et al. Lumbar muscle structure and function in chronic versus recurrent low back pain: a cross-sectional study. Spine J. 2017;17(9):1285–96.
Shamsi M, Sarrafzadeh J, Jamshidi A, Zarabi V, Pourahmadi MR. The effect of core stability and general exercise on abdominal muscle thickness in non-specific chronic low back pain using ultrasound imaging. Physiother Theory Pract. 2016;32(4):277–83.
Hamaoui A, Do MC, Bouisset S. Postural sway increase in low back pain subjects is not related to reduced spine range of motion. Neurosci Lett. 2004;357(2):135–8.
van Dieen JH, Reeves NP, Kawchuk G, van Dillen LR, Hodges PW. Motor control changes in low back pain: divergence in presentations and mechanisms. J Orthop Sports Phys Ther. 2019;49(6):370–9.
Mohammadi M, Ghamkhar L, Alizadeh A, Shaabani M, Salavati M, Kahlaee AH. Comparison of the reliance of the postural control system on the visual, vestibular and proprioceptive inputs in chronic low back pain patients and asymptomatic participants. Gait Posture. 2021;85:266–72.
Zhang Z, Gao Y, Wang J. Effects of vision and cognitive load on anticipatory and compensatory postural control. Hum Mov Sci. 2019;64:398–408.
Russo M, Deckers K, Eldabe S, et al. Muscle control and non-specific chronic low back pain. Neuromodulation. 2018;21(1):1–9.
Page S, Maheu M, Landry SP, Champoux F. The effects of brief swaying on postural control. NeuroReport. 2017;28(17):1119–21.
Lopes S, Correia C, Felix G, Lopes M, Cruz A, Ribeiro F. Immediate effects of Pilates based therapeutic exercise on postural control of young individuals with non-specific low back pain: a randomized controlled trial. Complement Ther Med. 2017;34:104–10.
Lamoth CJC, Meijer OG, Daffertshofer A, Wuisman PIJM, Beek PJ. Effects of chronic low back pain on trunk coordination and back muscle activity during walking: changes in motor control. Eur Spine J. 2005;15(1):23–40.
Chou R, Qaseem A, Snow V, et al. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147(7):478–91.
Bagheri R, Parhampour B, Pourahmadi M, et al. The effect of core stabilization exercises on trunk-pelvis three-dimensional kinematics during gait in non-specific chronic low back pain. Spine (Phila Pa 1976). 2019;44(13):927–36.
Yoo JH, Kim SE, Lee MG, et al. The effect of horse simulator riding on visual analogue scale, body composition and trunk strength in the patients with chronic low back pain. Int J Clin Pract. 2014;68(8):941–9.
Chow JH, Chan CC. Validation of the Chinese version of the Oswestry Disability Index. Work. 2005;25(4):307–14.
Lin J-D, Su S-F, Lin L-P, Hsu S-W, Wu J-L, Chu CM. The Roland-Morris disability scale for the assessment of non-specific low back pain outcomes among disability sector workers. Res Autism Spectr Disord. 2014;8(12):1635–40.
Koc M, Bayar B, Bayar K. A comparison of back pain functional scale with Roland Morris Disability Questionnaire, Oswestry Disability Index, and short form 36-health survey. Spine (Phila Pa 1976). 2018;43(12):877–82.
Roland M, Fairbank J. The Roland-Morris disability questionnaire and the Oswestry disability questionnaire. Spine (Phila Pa 1976). 2000;25(24):3115–24.
Ehsani F, Arab AM, Salavati M, Jaberzadeh S, Hajihasani A. Ultrasound measurement of abdominal muscle thickness with and without transducer fixation during standing postural tasks in participants with and without chronic low back pain: intrasession and intersession reliability. PM R. 2016;8(12):1159–67.
Whittaker JL, McLean L, Hodder J, Warner MB, Stokes MJ. Association between changes in electromyographic signal amplitude and abdominal muscle thickness in individuals with and without lumbopelvic pain. J Orthop Sports Phys Ther. 2013;43(7):466–77.
Zhang S, Xu Y, Han X, Wu W, Tang Y, Wang C. Functional and morphological changes in the deep lumbar multifidus using electromyography and ultrasound. Sci Rep. 2018;8(1):6539.
Hubley-Kozey CL, Vezina MJ. Muscle activation during exercises to improve trunk stability in men with low back pain. Arch Phys Med Rehabil. 2002;83(8):1100–8.
Hodges PW, Richardson CA. Inefficient muscular stabilization of the lumbar spine associated with low back pain. A motor control evaluation of transversus abdominis. Spine (Phila Pa 1976). 1996;21(22):2640–50.
Radebold A, Cholewicki J, Polzhofer GK, Greene HS. Impaired postural control of the lumbar spine is associated with delayed muscle response times in patients with chronic idiopathic low back pain. Spine. 2001;26(7):724–30.
Osuka S, Koshino Y, Yamanaka M, et al. The onset of deep abdominal muscles activity during tasks with different trunk rotational torques in subjects with non-specific chronic low back pain. J Orthop Sci. 2019;24(5):770–5.
Wang H, Zheng J, Fan Z, et al. Impaired static postural control correlates to the contraction ability of trunk muscle in young adults with chronic non-specific low back pain: a cross-sectional study. Gait Posture. 2022;92:44–50.
Rose-Dulcina K, Genevay S, Dominguez D, Vuillerme N, Armand S. O105: Asymmetry of lumbar muscle activity during sit-to-stand task in patients with chronic non-specific low back pain compared to healthy participants. Gait Posture. 2017;57:184–5.
Rose-Dulcina K, Armand S, Dominguez DE, Genevay S, Vuillerme N. Asymmetry of lumbar muscles fatigability with non-specific chronic low back pain patients. Eur Spine J. 2019;28(11):2526–34.
Panjabi MM. Clinical spinal instability and low back pain. J Electromyogr Kinesiol. 2003;13(4):371–9.
Zhang C, Zhang Z, Li Y, et al. Pain catastrophizing is related to static postural control impairment in patients with nonspecific chronic low back pain: a cross-sectional study. Pain Res Manage. 2020;2020:9629526.
Acknowledgements
The authors would like to thank Tingni Li, Cheng Xue, and Yang Jiajia for their useful advice on the study design. We would also like to express our gratitude to Professor Hanjun Liu for his assistance in statistical analysis.
Funding
This work and journal’s Rapid Service Fee was supported by the National Natural Science Foundation of China, Major plan grant number 82172532, 81972147; Young Scientists fund number 82102677, 82002398.
Authorship
All the authors have reviewed the final version of the manuscript, have approved it to be published, and have agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. H.J. Wang, Z.Y. Fan, and X. Liu contributed equally to the study. The corresponding authors are C.H. Wang and X. Chen.
Author Contributions
All authors contributed to the study conception and design. C. H. Wang and X. Chen designed the study and revised the main manuscript text. H.J. Wang and X. Liu analyzed the data and wrote most of the manuscript. Z.Y. Fan and J. X. Zheng wrote the rest and were the physiotherapists who instructed the participants in the exercise training. S. S. Zhang and S. Y. Zhang examined the contractility of TrA and MF measured the postural control presentations of the patients in the study. Q. H. Yu helped analyze the data and gave revised advice. Wai L. A. Lo helped with the language editing.
Disclosures
Hongjiang Wang, Ziyan Fan, Xin Liu, Jiaxuan Zheng, Shanshan Zhang, Siyun Zhang, Qiuhua Yu, Wai Leung Ambrose Lo, Xi Chen, Chuhuai Wang have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Human Subjects Ethics Subcommittee of the first affiliated hospital of Sun Yat-sen University (grant number 2020425). This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. The study was also enrolled in the Chinese Clinical trial, registration number ChiCTR2100043113. All participants provided written consent before they were recruited. The participants recruited in the study were also made aware of their role in the study. Consent was obtained from individuals to publish their images.
Data Availability
The datasets analyzed during the current study are available from the corresponding authors upon reasonable request.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, H., Fan, Z., Liu, X. et al. Effect of Progressive Postural Control Exercise Versus Core Stability Exercise in Young Adults with Chronic Low Back Pain: A Randomized Controlled Trial. Pain Ther 12, 293–308 (2023). https://doi.org/10.1007/s40122-022-00458-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00458-x