Abstract
Introduction
Opioids may be necessary for guideline-concordant acute perioperative pain management, but their use carries risks for unintended prolonged use and addiction. Guidelines recommend use of validated non-pharmacological pain care (NPPC) approaches in conjunction with prescribed opioids and other analgesics. Our protocol outlines a population-level, pragmatic trial that will test a bundled intervention comprised of an electronic health record (EHR) portal-based conversation guide, EHR clinical decision support (CDS), and a suite of self-management educational and support materials to encourage and advance NPPC use.
Methods
We are conducting a stepped-wedge, cluster-randomized pragmatic trial spanning seven surgical specialties across six geographically diverse locations within the Mayo Clinic Enterprise. Thirty two surgical practices across six locations (Rochester, Minnesota; Mankato, Minnesota; La Crosse, Wisconsin; Eau Claire, Wisconsin; Phoenix, Arizona; Jacksonville, Florida) comprise 22 distinct practice clusters that are randomly assigned to one of five steps using constrained randomization. Steps “go live” by initiating the intervention at 7-month intervals between March 2021 and July 2023. Patients over 18 years of age who are scheduled for qualifying procedures within “live” consenting practices are sent a Healing After Surgery guide via their patient portals pre-operatively, directing them to identify their preferred NPPC modalities among 13 approaches. These selections create CDS options for care teams to support patients with self-management materials that reinforce safe NPPC use.
Planned Outcomes
Patients’ clinical, demographic, and outcome data will be abstracted from the Epic EHR. Primary outcomes will be the Patient Reported Outcomes Measurement Information System (PROMIS) pain interference and physical functioning computer adaptive tests (CAT) collected at 1, 2, and 3 months postoperatively via the patient portal. We will mail printed versions of the 6-item PROMIS short forms to portal non-responders to minimize bias. Secondary outcomes will include the PROMIS anxiety CAT, opioid consumption, and self-reported NPPC use.
Trial Registration
ClinicalTrials.gov identifier, NCT04570371.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Perioperative pain management should incorporate non-pharmacologic pain care options in conjunction with pain medication to achieve guideline concordance |
Providing patients with autonomy to choose their preferred non-pharmacologic pain care strategies and develop their own pain management plan, with support from their care team and self-management educational resources, may enhance effective pain control and improved function |
This protocol describes the designed cluster-randomized, stepped-wedge NOHARM trial, which seeks to test the effectiveness of such an intervention by leveraging patient-facing components of the electronic health record along with clinical decision support non-pharmacologic pain management strategies to support healing after surgery |
We hypothesize this bundled intervention will reduce pain and improve functioning postoperatively, which in turn may reduce postoperative anxiety and opioid consumption |
Introduction
Background (6a)
The USA faces a deadly opioid crisis, which the federal and state governments have attempted to curb by altering the supply, manufacturing, and prescribing of opioids [1]. However, many patients receive opioid prescriptions postoperatively that are poorly matched to pain’s presence or intensity, a practice that diverges from the much more conservative prescribing trends of other countries [2]. This may place patients at risk for unintended, prolonged opioid use leading to potential misuse and abuse [3]. Rates of prolonged opioid use (filling a prescription around 90–180 days postsurgery after an earlier opioid prescription) ranged from 3% to 6.5% in postoperative patients [4, 5]. Furthermore, many adults reporting opioid misuse indicated receiving opioids from family or friends [6], suggesting that prescribing practices may put others besides the patient at risk from informal or deliberate diversion. To reduce these risks, the Centers for Disease Control and Prevention, along with others, have encouraged the use of non-opioid medications and non-pharmacological pain care (NPPC) approaches for treating postoperative pain, with opioids reserved for the acute postoperative period [7,8,9].
NPPC modalities, including movement [10, 11], touch/physical [12], and relaxation modalities [12], are effective in reducing postoperative pain, but have not been readily adopted in most surgical practices. Thus, setting appropriate pain expectations and helping patients develop a multimodal pain management plan that includes non-pharmacological options are crucial in curbing postoperative opioid use and implementation of such a practice is a critical clinical need [13]. Importantly, patient-driven decision-making has been found to predict a decreased likelihood of reporting frequent pain [14], underscoring the importance of letting patients actively choose and initiate their pain management plan.
The Non-pharmacologic Options in postoperative Hospital-based And Rehabilitation pain Management (NOHARM) pragmatic clinical trial will test an intervention intended to help patients develop an individualized postoperative pain management plan preoperatively that incorporates NPPC approaches and provides resources to actualize and advance this planning. The intervention was designed to seamlessly integrate into clinical and electronic health record (EHR) workflows across a variety of specialties and settings with emphasis on scalability and sustainability. The present protocol was prepared in accordance with the SPIRIT 2013 checklist [15] and numbered headings indicate correspondence with the numbered items in the checklist.
Objectives (7)
The overarching objective of this trial is to test an EHR-based intervention to provide patients with perioperative education and support for using validated non-pharmacologic options for managing postoperative pain in conjunction with necessary medication prescribed by their care teams. We aim to help patients to develop a preoperative pain management plan that includes non-pharmacologic options and provide support for their use of these modalities throughout their continuum of care. We hypothesize that this intervention will improve patients’ pain management and physical functioning and lessen their anxiety. We also hypothesize this approach will help patients better control their pain and thus reduce their consumption of opioids.
Methods
Study Design
Trial Design (8)
The NOHARM trial uses a stepped-wedge, cluster-randomized trial design [16] (Fig. 1). The trial will include all patients receiving a qualifying procedure from 32 practice groups that form 22 clusters. Clusters were randomized into one of five steps in the stepped-wedge design, each with a pre-specified start date at 7-month intervals beginning March 1, 2021. The last step will go live on July 1, 2023. After go live, each step remains live until the trial ends on January 31, 2024. Under the stepped-wedge design, each cluster will serve as its own control by collecting baseline data prior to go live.
We chose a stepped-wedge cluster randomized design to balance rigor and practicality. A stepped-wedge design supports the inference of causal relationships as with a parallel design randomized control trial while at the same time incorporating the convenience of a one-time pre–post intervention deemed more acceptable to surgical practices accustomed to quality improvement projects. This design also reduces the staffing and training burdens associated with simultaneous go live across a large number of sites. The primary limitation of a stepped-wedge design relative to a parallel randomized design is potential confounding by calendar time; however, calendar time will be directly measured and accounted for in the analysis. A stepped-wedge design can adjust for temporal trends, and also typically produces greater statistical power when compared with similarly sized parallel designs [17].
Choice of Comparators (6B)
Each cluster will serve as its own control by collecting baseline data via questionnaires delivered prior to a cluster’s go live. Clusters that have a later go live date during the trial will also serve as controls for clusters that have an earlier go live date.
Setting (9)
NOHARM will occur in seven surgical specialties across six hospital locations within the Mayo Clinic Health System Enterprise that vary in size, geographic setting, and rurality (Fig. 1). Mayo Clinic in Rochester, Minnesota; Mayo Clinic in Jacksonville, Florida; and Mayo Clinic in Phoenix, Arizona are large teaching hospitals in urban settings. Mayo Clinic’s Eau Claire, Wisconsin; La Crosse, Wisconsin; and Mankato, Minnesota sites are community hospitals within the Mayo Clinic Health System drawing largely rural patient populations. About 50% of patients receiving qualifying NOHARM procedures will have their surgeries performed at Mayo Clinic Rochester, 25% will have their surgeries performed at Mayo Clinic Florida or Arizona, and the remaining 25% of patients receiving qualifying NOHARM procedures will have their surgeries performed at the Mayo Clinic Health system locations.
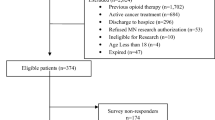
Eligibility Criteria (10)
Patients 18 years or older undergoing a qualifying surgical procedure (see Table 1) from a cluster in an active step will be automatically enrolled in the trial. No exclusion criteria will be applied. However, patients treated in Minnesota, who have requested their medical records not be used for research, will have their files redacted from research analysis in accordance with Minnesota state law. Patients who are citizens of the European Union or China or Hong Kong will also have their files redacted from all research analyses (following the European Union General Data Protection Regulation and similar protections in some East Asian countries).
Risk–Benefit Determination, Consent, and Human Subjects Protection (26a)
This trial meets the definition of a “standard of care” trial in which an enhanced version of standard of care is compared to usual care. Moreover, clinical decision support was designed to prompt and support care teams in having perioperative discussions about non-pharmacologic options with patients, which is an existing element of guideline-concordant care [7,8,9]. While providers will help deliver the intervention, clinical decision support was designed to integrate with—and not disrupt—existing workflows, and individual providers are not being evaluated. All modalities included in the intervention were chosen because of their demonstrated safety and effectiveness. Furthermore, the chosen modalities are readily available, so patient educational materials developed for this study promote safe modality use and provide patients with important information about contraindications and precautions. Thus, this trial received a designation of minimal risk research for both patients and clinicians. Under certain circumstances, e.g., standard of care research conducted on a large scale that also satisfies a minimal risk or less designation, alternatives to individual patient consent authorization may be permissible [18].
Given these factors, the Mayo Clinic Institutional Review Board (IRB) reviewed and approved this protocol. The IRB endorsed waiving individual patient and clinician consent, citing the intervention’s congruence with standard of care, practicability constraints, a robust practice engagement, and written endorsement plan as a substantive alternative authorization. This trial complies with the Helsinki Declaration of 1964 and its amendments.
Care Team Engagement
In lieu of consenting potentially hundreds of individual care team members per patient, we sought advanced endorsement from all proposed Mayo Clinic practice leadership. Engagement of key stakeholders (e.g., site principal investigators, practice administration, and other staff) occurred months (and sometimes years) before the cluster’s go live date, ensuring ample preparation time. More specifically, months before go live, the trial’s principal investigators present at each surgical practice’s meeting for physician awareness, discussion, and engagement. Once surgeons have been briefed on the trial, a written endorsement is solicited from each practice’s surgical chair, and members of the study team reach out to operations administrators and other site champions (e.g., site principal investigators and clinical study personnel) to determine the appropriate hospital staff leadership contacts (e.g., outpatient and inpatient nursing managers) to schedule an initial overview meeting and discuss staff training needs. During these meetings, staff leaders also identify other key personnel who should be included in pre-go live discussions (e.g., nursing managers, adminstrators/leadership, education specialists, clinical nurse specialists). This ongoing engagement work typically consists of assigning brief role-specific online training modules to staff and holding question and answer sessions or joining existing staff meetings or huddles. In the weeks before go live, members of the study team also conduct site walk-throughs. A similar engagement process is followed for engaging physical and occupational therapy leaders and training their staff.
Intervention
Healing After Surgery Guide (11a)
This study leverages the Epic EHR to identify and assign a Healing After Surgery guide to eligible patients. Enrolled patients receive an automated patient portal message with a link to the Healing After Surgery guide, initiating the intervention. The guide discusses realistic pain expectations, opioid safety, and 13 different NPPC modalities (Fig. 2). Patients indicate their NPPC modality preferences via the guide, which are recorded as structured data elements in the EHR to drive clinical decision support described below. The guide is only available in English. Figure 3 describes the intervention from the patient’s perspective.
Clinical Decision Support (CDS)
Easy identification of NOHARM patients. To help inpatient, postoperative, and post-anesthesia care unit (PACU) nurses, physical and occupational therapists, and preoperative evaluation clinic staff identify and support NOHARM patients, a hot pink banner appears in the patient’s EHR with an embedded link to a portable document format (PDF) document with just-in-time education for teams (e.g., screenshots, instructions, and training clips).
Prompts to support NPPC selection and use. NOHARM patient charts include the patient’s pre-selected modalities in multiple locations (e.g., on the Summary View, Admission Navigator, and in flowsheet rows) if the patient made selections in their guide prior to hospitalization. Appropriate NPPC orders (with precautions) will also be automatically presented to inpatient nurses if the patient made selections. Every time an inpatient nurse documents pain greater than one (on a ten point scale) for the first time in a 12-h period, a best practice alert (BPA) informs them to complete outstanding education on the patient’s NPPC selections or to elicit patient selections. This BPA continues to deploy per shift until the patient has made NPPC selections and received all corresponding education. A BPA also appears for physical and occupational therapists directing them to either elicit NPPC selections or incorporate existing selections into treatment as appropriate.
Support for NPPC education. CDS elements prompt Education Points in Epic, corresponding to a patient’s selected NPPC modalities, to populate the nursing Education Tab. The NPPC content includes talking points and links to educational handouts and videos. Printable handouts within Epic’s Education Tab augment one-page handouts describing the NPPC modalities stocked on nursing units. Video content, accessible through hospital televisions and bedside tablets, reinforces precautions and potential modifications needed to safely perform the modalities. Nursing tasks reinforce education goals.
Encouraging post-discharge use of NPPC. The discharge summary, called an After Visit Summary (AVS), is automatically populated with information corresponding to the patient’s NPPC selections and supportive post-discharge resources.
Healing After Surgery Patient Resources
A Healing After Surgery website expands on content in the portal-based Healing After Surgery guide by providing videos and resources to support pre-admission preparation and post-discharge modality use. Further, knowledgeable clinicians lead triweekly Healing After Surgery group Zoom calls and cover a Healing After Surgery toll-free number to support perioperative non-pharmacologic modality use and answer patient questions in a timely manner. Patients receive information about these resources via the patient portal in a message that includes educational materials.
Patient resources that do not require portal use or broadband access. Nursing units have video resources available via the hospital’s television system that patients can view during their hospital stay. They also have a stock of print materials (including 1-page modality flyers and a planning workbook) and Healing After Surgery DVDs (with similar video content to the Healing After Surgery website) to distribute to patients. The print materials list the toll-free number patients can call with questions. Patients interested in joining the Healing After Surgery group Zoom-based calls, who lack broadband access, can join by phone.
Portal Message Triggered by Opioid Refill Request
In addition, patients requesting any opioid refill within 3 months of surgery, regardless of how they solicit it, will receive a portal message encouraging them to use non-pharmacologic options and the Healing After Surgery Zoom calls and toll-free number.
Discontinuation (11b)
Individuals will remain enrolled in the trial for 3 months following their index procedures by virtue of being cared for in a consenting practice. At the 3-month point after surgery, they will be considered no longer active on the protocol.
Adherence (11c)
Preoperative care teams encourage patients to complete the portal-based Healing After Surgery guide. If patients have still not completed the guide within 4 days of their surgery (and the surgical request was placed a minimum of 8 days before their scheduled surgery), they receive a reminder portal message. Inpatient teams may also ask patients about their non-pharmacologic preferences and enter these selections in patients’ electronic charts, but patients choosing not to select, learn about, or use NPPC modalities despite encouragement will not be required to do so.
CDS banners, prompts, alerts, and educational materials help care teams deliver NOHARM content, using their discretion. In-person NOHARM support for inpatient floors is provided by a “boots on the ground” point person for each study site to ensure that staff feel comfortable. Epic discrete data elements in the inpatient flowsheet will allow us to track staff adherence to modality education and delivery objectives.
Concomitant Care (11d)
The intervention will be turned on for all qualifying surgical procedures performed by surgeons within practices that have gone live with the intervention and may include patients participating in other trials or treatments. Every other dimension of their care should remain the same for the duration of the trial.
Ancillary and Post-trial Care (30)
The trial includes Mayo Clinic patients who will have the same access and availability to care at Mayo Clinic when the trial is over. There are no patient incentives or compensation for participating.
Sample Selection
The study sample was selected to provide a diverse, large, and population-based representation of the Mayo Clinic surgical practice. We included both surgical procedures requiring an inpatient stay and less invasive ones, including same-day procedures, to understand the effectiveness of the intervention across different surgical populations.
Participant Timeline (13)
The sequence of enrollment through all steps of the intervention and assessment is depicted in Fig. 3.
Sample Size (14)
We aim to recruit 86,726 patients, an estimate based on 2018 surgical volumes of qualifying procedures. To estimate detectable effects we used simulation, randomly allocating clusters 5000 times to the five non-baseline steps and calculated the detectable effect for each allocation [17]. On the basis of this approach we estimate a detectable effect of 0.085 standard deviations in the primary outcomes.
Recruitment (15)
Epic assignment logic will use Current Procedural Terminology (CPT) surgery codes, when placing an initial procedure order (see Appendix 1 in the Supplementary Material), and location to add eligible patients to the NOHARM registry, which triggers the automatic delivery of the Healing After Surgery guide to a patient’s portal.
Allocation (16a–c)
As a result of the nature of the trial’s stepped-wedge design, allocation is only relevant for a cluster’s go live date because all clusters will eventually receive the intervention. We used constrained randomization to account for differences in clusters in terms of group (orthopedic/gynecologic/colorectal/obstetrics, pulmonary-thoracic/cardiac, transplant), site, surgical volume, and number of teams (1, 2, or 4) [19]. In constrained randomization, randomization is simulated a large number of times, and a metric is calculated which reflects the balance across all factors of interest; the final randomization is selected from among those simulated randomizations which have maximum balance. We simulated 100,000 different allocations, and from these calculated a balance metric for each allocation, and then randomly selected an allocation sequence with the smallest balance metric. Clusters learn their step assignment when we engage practice supervisors in the months prior to their go live. We will not actively conceal the allocation sequence.
Blinding (17a)
As a function of the stepped-wedge design, the intervention will be “off” or “on” for all qualifying surgical procedures within a practice (cluster). NOHARM patients have clear chart identifiers to prompt their care team to deliver the intervention. We will not actively conceal the fact that patients are participating in a study, but patients will not be explicitly told they are part of a research study and will likely think the Healing After Surgery resources and support they receive for NPPC use are standard perioperative care for qualifying procedures.
Measurements
Data Collection (18a, b)
This study will leverage existing Epic functionality to collect all patient data. All trial locations use the same iteration of the Epic EHR which has provider and patient-facing components. Patients can create a patient portal account to view treatment notes and test results, message their care teams, complete assigned questionnaires, and manage billing and prescription refills, among other tasks. Standardized Epic data gathering and viewing capabilities across all trial sites facilitates data abstraction for research purposes.
Participants’ sociodemographic and clinical information will be abstracted from the curated Epic Clarity database. Sociodemographics will include age, gender, educational level, zip code, marital status, and disability status. Clinical characteristics will include the Elixhauser comorbidity index, comorbid conditions, oral morphine equivalents (OMEs) consumed during the 24 h prior to hospital admission, medications at hospital registration for index procedure, index surgical procedure, and ICU stay. Additional characteristics will include patients’ Epic portal use during the month prior to their surgical procedure.
Patient Reported Outcomes Measurement Information System (PROMIS) computer adaptive tests (CATs) will be automatically assigned to patients enrolled in NOHARM at set intervals using Epic logic. Additionally, patients who undergo surgeries from practices that are part of NOHARM but have not gone live with the intervention yet will contribute control data by completing PROMIS CATs assigned to them at baseline, 1, and 3 months postsurgery. Non-active and active clusters will both also be asked self-reported opioid use at baseline and 3 months postsurgery. Active clusters will report on NPPC use at 1, 2, and 3 months postsurgery. See Table 2 for a list of the measures assigned at each timepoint.
PROMIS CATs can be completed online via the MyChart patient portal or on Welcome tablets available in clinic during any follow-up visit in the 3 months following their surgery. Patients receive a maximum of three reminder portal messages, sent every 4 days or until survey completion. Patients who do not complete the PROMIS CATs (pain and function) via their portal 1 month postoperatively will be mailed a paper version of the pain and function measures at 2 months and 3 months postoperatively along with a prepaid return envelope. (An accompanying cover letter in the mailed version will instruct patients to complete these measures in either paper or online format.)
Planned Outcomes (12)
Primary Outcomes
The NOAHRM trial’s primary outcomes, physical functioning and pain interference, will be collected via PROMIS CATs at baseline, 1 month, 2 months, and 3 months postoperatively for the intervention group and at baseline, 1 month, and 3 months postoperatively for the control group.
Secondary Outcomes
Anxiety
Anxiety will be measured using PROMIS CATs administered at baseline and 3 months postoperatively. An additional single-item measuring anxiety from the four-item Patient Health Questionnaire (PHQ-4) [20] will be administered via the Healing After Surgery guide in the patient portal in order to inform tailored intervention delivery.
Inpatient Pain Scores
Additionally, all patients’ numerical rating scale pain intensity scores are recorded by hospital nurses every shift during their inpatient stay and pain catastrophizing scale scores will be extracted from the EHR.
Opioid Consumption
We will measure opioid consumption during the inpatient stay and opioid prescriptions after discharge. Inpatient opioid use, including intraoperative opioids, will be captured by extracting daily in-hospital consumption of OMEs [21,22,23] from the medication administration log in the EHR. Post-discharge opioid prescriptions will be captured by extracting data from the patient’s EHR for opioids (transdermal and oral, converted to oral morphine equivalents) prescribed by their Mayo Clinic clinicians at discharge and over the subsequent 3 months. Documentation of opioids prescribed (not necessarily consumed) in the year preceding surgery will also be extracted from the EHR. Patients will also complete a subscale of a validated opioid consumption survey [23] 3 months postoperatively to capture opioids not documented in the EHR. Medication use is measured with the Tobacco, Alcohol, Prescription medication, and other Substance use (TAPS) [24] prescription medication use item and an opioid prescribing survey.
NPPC Use
Care team provision of and/or education about a patient’s selected modalities documented in Epic flowsheets will be extracted from the EHR to count the number of instances of NPPC provision/education documented.
Patients will also receive a portal-based survey at 1, 2, and 3 months postoperatively, asking them to select which of the 13 NPPC modalities they have used. For each modality that the patient reports having used, they will be administered a follow-up question via branching logic that asks, “How many times per week, on average, do you use [modality]?”.
Healthcare Utilization
Data on healthcare utilization will be extracted from the EHR, including administrative and billing records of hospitalization (including procedures and admission/discharge diagnoses), post-acute care, emergency department visits (including procedures and diagnoses), surgical clinical outpatient visits (including billing, CPT, and International Classification of Diseases-Tenth Revisions (ICD-10) codes), and surgical care team calls and post-acute care.
Management (19)
All data for this study will be recorded in the EHR by clinical providers per routine care documentation or from MyChart patient portal questionnaires. Our team will perform all data extraction. To ensure extraction is working correctly, every 2–3 months we will extract data for around 2–5% of patients from the most recently activated cluster and compare the extracted data to the EHR. Once the study is complete, we will extract data on individual covariates (described in the “Measurements” section) and comorbidities (collected with the Elixhauser comorbidity index), and treatment and outcome data needed for analyses.
Data Analysis
Statistical Methods (20a, c)
All analyses will be appropriate for cluster-randomized stepped-wedge trials [25]. All patients will be analyzed on an intention-to-treat basis; this principle will be extended to the cluster status, so that delays in implementation of an intervention will not affect the intervention status of patients. First, we will summarize patient characteristics and outcomes by intervention status and assess balance by reporting standardized differences. Then, to test the primary hypotheses of the study, we will estimate a series of mixed effects generalized linear models. All analyses will account for intra-cluster correlations (e.g., using standard errors adjusted by cluster) and any patient characteristics identified as being imbalanced across intervention status as determined by a standardized mean difference greater than 0.1. Models will contain intervention status, calendar time defined as elapsed months, cluster as a random intercept effect, cluster level factors, and imbalanced patient characteristics. We will exclude patients who had previously requested their information not be used for research purposes. All analyses will be on an intention-to-treat basis, with patients analyzed according to the status of their cluster at time of treatment.
The EHR-based approach to data collection, though designed to optimize complete and balanced collection of primary and secondary measures, will almost certainly result in some missing data. We will carefully examine whether there is evidence for differential dropout across the clusters. We will compare clusters and participants with missing and captured outcomes with respect to baseline characteristics in order to gauge the missing data mechanism (e.g., missing at random vs. likely nonignorable). While definitive tests for nonignorability are not available because of the nature of the problem (the likelihood of missing data is dependent upon the unobserved outcome value), we will take advantage of sophisticated sensitivity analyses [26, 27] to determine the robustness of study results and conclusions. In addition, we will use modern techniques for multiple imputation to generate predicted values for missing outcomes and incorporate them into the primary analyses.
Patients who do not report NOHARM primary and secondary patient reported outcome measures (PROMs) during the 3 month postsurgical interval will be treated as “lost to follow-up” in the analyses. We will ascertain vital status and postsurgical healthcare utilization to distinguish whether patients are deceased, have had no postoperative Mayo Clinic encounters, remain institutionalized in post-acute care facilities, or are non-responders to the NOHARM PROMs.
Anxiety, Pain, Physical Functioning
We will explore anxiety, pain, and physical functioning continuous scores, measured preoperatively and at 1, 2, and 3 months postoperatively, using the following model, separately, for each outcome:
In this model, \({Y}_{ij}\) signifies the tth postoperative measure for the patient i belonging to cluster j; Yij0 is the patient’s baseline measure. Next, Iij represents intervention vs. control group membership, T represents time, Xij accounts for patient characteristics (e.g., type of surgery), and Zj accounts for cluster characteristics. The error terms uj~N(0,τ2) account for random effects of cluster, wij~N(0,η2) account for within-patient correlation, and eijt~ N(0,σ2) represents residual patient error. We will test whether βI = 0 to determine whether the intervention affects the outcome. In secondary analyses we will dichotomize each outcome and estimate a model analogous to Eq. (1) with a logit link.
NPPC Use
We will assess differences in NPPC use between intervention and control patients at 1, 2, and 3 months postoperatively. We will primarily rely on self-reported frequency of use for each modality. We will specify modality use several ways in an effort to gauge the impact of any use, frequency of use, use of specific modalities, and by creating a count of the number of patient-reported non-pharmacologic modalities used. We will conduct mediator analyses to estimate the degree to which self-reported modality use explains changes in the primary and secondary outcomes among the intervention group. All mediator analyses will be exploratory. The following example equation illustrates how we will explore this. The model differs slightly from the first by removing the inclusion of the patient’s baseline measurement \({Y}_{ij0}:\)
We will explore whether βI = 0 to determine if the intervention had an effect on NPPC use.
Opioid Use During Hospital Stay
We will use the following model to explore inpatient opioid use, as oral morphine equivalents consumed daily (continuously and then categorically), accounting for days since surgery, represented by \({D}_{ij}\):
where Yijd is the number of oral morphine equivalents consumed on day d.
Amount of Opioids Prescribed Post-discharge
We will measure daily oral morphine equivalents prescribed at and following discharge, using model (3), with \({D}_{ij}\) representing number of days since discharge.
Number of Opioid Prescriptions Post-discharge
We will estimate whether the intervention had an effect on the number of opioid prescriptions given in the 3 months after surgery, using a modified version of model (2) that includes a link function appropriate for count data. Using an empty model to obtain Akaike information criterion (AIC) values for the distribution, we will identify the appropriateness of using a Poisson distribution or negative binomial and whether it should be zero-inflated.
Daily Opioid Use
Whether the intervention influences patient reported prescription of daily opioids (yes or no) 3 months after their surgery will be evaluated with a modified version of model (2) that uses the logit link.
Monitoring (21a)
A Data Safety Monitoring Board will provide oversight in accordance with National Institute of Aging (NIA) guidelines. We may conduct interim analysis if requested by the Data and Safety Monitoring Board (DSMB) or if any unplanned study modifications occur. We have not specified any stopping rules for this minimal risk intervention.
Harms (22)
Adverse events due to our intervention will likely be rare because NOHARM promotes guideline-concordant postoperative NPPC use. Educational materials include appropriate precautions and contraindications, and the patient toll-free number and group Zoom calls offer additional safety. We do not anticipate any adverse events or harm to provider participants as they will choose how to use and promote the guideline-concordant resources we have developed and are encouraged to use their clinical discretion.
Surgical teams will monitor for postoperative adverse events as part of standard postoperative care and report to us any events that could reasonably be attributed to the intervention. Additionally we will compare the number of falls recorded in the EHR, as well as the assignment of ICD-10 codes for burn, skin irritation, and muscle aches and compare them between groups. We will follow appropriate procedures outlined in our IRB document for investigation, documentation, and reporting such events and receive oversight from the NIA appointed DSMB.
Auditing (23)
We do not plan on formally auditing trial conduct, but the intervention’s many touch points with clinical providers (e.g., ambulatory staff, inpatient nursing, physical therapists) may act as a check. Further, NOHARM “boots on the ground” study staff use Epic report data to identify staff who may need assistance or have questions about NOHARM. We also may share some report data with managers for awareness of their staff’s engagement with the intervention.
Strengths and Limitations
The large-scale pragmatic nature of this trial will enable us to test the effectiveness of a low-touch, highly scalable intervention for systematically aligning care with the guideline-endorsed standard for managing postoperative pain through preoperative planning and support for use of non-pharmacological modalities. We leveraged and adapted the existing Epic EHR system to deliver this intervention and seamlessly integrated CDS into clinical workflows to promote sustainability. Moreover, we were able to develop an intervention that can be implemented at multiple health system sites that differ in geographic area, size, and rurality, and within diverse surgical disciplines, extending its potential reach. However, all sites participating in this trial belong to the Mayo Clinic enterprise, which may limit the generalizability of our findings to other health systems.
Our intervention has been designed to reduce clinical burden. We will regularly and proactively engage with practices to assess the acceptability and usability of the system, but the intervention itself should not intrude on practice workflows, particularly for prescribing physicians and advanced practice providers. Surgeons will be encouraged to convey support of the intervention to patients during preoperative visits. Ambulatory staff will also be asked to encourage patients to utilize the Healing After Surgery guide as part of routine preoperative education and reinforce postoperative modality use during routine postoperative follow-up phone calls. However, these activities are at their discretion. Inpatient nurses and physical and occupational therapists will be most hands-on in supporting the modalities. This is consistent with their existing role and compatible with existing workflows. We also do not expect inpatient staff to become experts in the modalities.
As a result of the low-touch nature of the intervention, the planned modest effect size is warranted. Patients will likely vary in motivation and commitment to using the educational resources provided. To pre-emptively address this, we created Healing After Surgery workbooks to help patients address common barriers and to create a plan for NPPC use. NOHARM group Zoom calls and a patient toll-free number also provide ongoing access to support; however, these require patients to actively seek support, and those most likely to reach out with questions may be those who are already highly motivated to use NPPC. Furthermore, because this trial will recruit all patients receiving a qualifying surgical procedure without applying any exclusion criteria, the large-scale nature makes it challenging to tailor the intervention to different subsets of patients. For instance, the EHR and patient portal lack Spanish translation as do Healing After Surgery educational resources. Thus, patients who only speak Spanish may have more difficulty engaging with the intervention. But such is the reality of the support currently present in the organization conducting the trial. Efforts to translate paper-based educational materials into Spanish are currently underway. Nonetheless, our high-volume, low-touch intervention has the potential to reach many patients, conferring value even if the effects are more modest than resource-intensive, high-touch interventions that reach fewer patients [28].
Ethics
We received Mayo Clinic Institutional Review Board approval (IRB #20-004839) prior to participant enrollment. We also proactively engaged the Ethics and Regulatory Core of the National Institutes of Health (NIH) Clinical Trials Collaboratory. The NIH Clinical Trials Collaboratory provides an opportunity to discuss ideas and challenges with an unbiased group of medical and research professionals. Additionally, we met regularly with the Mayo Clinic IRB prior to trial initiation. Subsequent protocol changes will be submitted for approval as an amendment before enactment.
References
Soelberg CD, Brown RE Jr, Du Vivier D, Meyer JE, Ramachandran BK. The US opioid crisis: current federal and state legal issues. Anesth Analg. 2017;125(5):1675–81.
El Moheb M, Mokhtari A, Han K, et al. Pain or no pain, we will give you opioids: relationship between number of opioid pills prescribed and severity of pain after operation in US vs non-US patients. J Am Coll Surg. 2020;231(6):639–48.
Hah JM, Bateman BT, Ratliff J, Curtin C, Sun E. Chronic opioid use after surgery: implications for perioperative management in the face of the opioid epidemic. Anesth Analg. 2017;125(5):1733–40.
Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017;152(6):e170504.
Clarke H, Soneji N, Ko DT, Yun L, Wijeysundera DN. Rates and risk factors for prolonged opioid use after major surgery: population based cohort study. BMJ. 2014;348:g1251.
Han B, Compton WM, Blanco C, Crane E, Lee J, Jones CM. Prescription opioid use, misuse, and use disorders in U.S. Adults: 2015 National Survey on Drug Use and Health. Ann Intern Med. 2017;167(5):293–301.
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Postsurgical Pain. Available from: https://www.cdc.gov/acute-pain/postsurgical-pain/index.html. Accessed 1 Dec 2021.
Bree Collaborative and Washington State Agency Medical Directors’ Group. Prescribing opioids for post-operative pain—supplemental guidance. Available from: http://www.agencymeddirectors.wa.gov/Files/FinalSupBreeAMDGPostopPain091318wcover.pdf. Accessed 1 Dec 2021.
Michigan OPEN. Acute care opioid treatment and prescribing recommendations: Summary of selected best practices. Available from: https://michigan-open.org/wp-content/uploads/2022/03/Surgery-Best-Practices.pdf. Accessed 13 May 2022.
Monticone M, Ferrante S, Rocca B, et al. Home-based functional exercises aimed at managing kinesiophobia contribute to improving disability and quality of life of patients undergoing total knee arthroplasty: a randomized controlled trial. Arch Phys Med Rehabil. 2013;94(2):231–9.
Moffet H, Collet JP, Shapiro SH, Paradis G, Marquis F, Roy L. Effectiveness of intensive rehabilitation on functional ability and quality of life after first total knee arthroplasty: a single-blind randomized controlled trial. Arch Phys Med Rehabil. 2004;85(4):546–56.
Tick H, Nielsen A, Pelletier KR, et al. Evidence-based nonpharmacologic strategies for comprehensive pain care: the Consortium Pain Task Force white paper. Explore (NY). 2018;14(3):177–211.
Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain. 2016;17(2):131–57.
Borders TF, Xu KT, Heavner J, Kruse G. Patient involvement in medical decision-making and pain among elders: physician or patient-driven? BMC Health Serv Res. 2005;5(1):4. https://doi.org/10.1186/1472-6963-5-4.
Chan AW, Tetzlaff JM, Gotzsche PC, et al. SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials. BMJ. 2013;346:e7586.
Mdege ND, Man MS, Taylor Nee Brown CA, Torgerson DJ. Systematic review of stepped wedge cluster randomized trials shows that design is particularly used to evaluate interventions during routine implementation. J Clin Epidemiol. 2011;64(9):936–48.
Woertman W, de Hoop E, Moerbeek M, Zuidema SU, Gerritsen DL, Teerenstra S. Stepped wedge designs could reduce the required sample size in cluster randomized trials. J Clin Epidemiol. 2013;66(7):752–8.
McKinney RE Jr, Beskow LM, Ford DE, et al. Use of altered informed consent in pragmatic clinical research. Clin Trials. 2015;12(5):494–502.
Li F, Lokhnygina Y, Murray DM, Heagerty PJ, DeLong ER. An evaluation of constrained randomization for the design and analysis of group-randomized trials. Stat Med. 2016;35(10):1565–79.
Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics. 2009;50(6):613–21.
Thiels CA, Ubl DS, Yost KJ, et al. Results of a prospective, multicenter initiative aimed at developing opioid-prescribing guidelines after surgery. Ann Surg. 2018;268(3):457–68.
Thiels CA, Anderson SS, Ubl DS, et al. Wide variation and overprescription of opioids after elective surgery. Ann Surg. 2017;266(4):564–73.
Wyles CC, Hevesi M, Trousdale ER, et al. The 2018 Chitranjan S. Ranawat, MD Award: developing and implementing a novel institutional guideline strategy reduced postoperative opioid prescribing after TKA and THA. Clin Orthop Relat Res. 2019;477(1):104–13.
McNeely J, Wu LT, Subramaniam G, et al. Performance of the Tobacco, Alcohol, Prescription Medication, and Other Substance Use (TAPS) tool for substance use screening in primary care patients. Ann Intern Med. 2016;165(10):690–9.
Hussey MA, Hughes JP. Design and analysis of stepped wedge cluster randomized trials. Contemp Clin Trials. 2007;28(2):182–91.
Troxel AB, Ma G, Heitjan DF. An index of local sensitivity to nonignorability. Stat Sin. 2004;14:1221–37.
Ma G, Troxel A, Heitjan D. An index of local sensitivity to nonignorable dropout in longitudinal modeling. Statist Med. 2005;24:2129–50.
von Thiele SU, Aarons GA, Hasson H. The value equation: three complementary propositions for reconciling fidelity and adaptation in evidence-based practice implementation. BMC Health Serv Res. 2019;19(1):868.
Acknowledgements
Marcel Salive, MD, NIA; Theresa Cruz, PhD, National Institute of Child Health and Human Development (NICHD); and Scott Wright, MD, Mayo Clinic IRB; as well as the Biostatistics & Design as well as the Ethics & Regulatory Cores of the Healthcare Systems Collaboratory all provided invaluable feedback in the construction of this protocol. Becky Fulton, P.T., also played a valuable role in this work.
We would like to acknowledge our dear colleague and friend, Dr. Aaron Leppin, for his thoughtful contributions to this manuscript and tireless commitment to the NOHARM trial until his passing on November 3, 2021. He is included in the group authorship because of his significant contribution to this work before his passing.
Funding
This work was supported by the NIH through the NIH HEAL Initiative under award numbers UG3AG067593 and UH3AG067593 from the NIA and the National Institute of Neurological Disorders and Stroke (NINDS). This work also received logistical and technical support from the PRISM Resource Coordinating Center under award number U24AT010961 from the NIH through the NIH HEAL Initiative. The funders provided funding for the trial and Rapid Service Fee. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or its HEAL Initiative.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Dr. Sarah Redmond, the Mayo Clinic NOHARM Research Team, Dr. Andrea Cheville, and Dr. Jon Tilburt contributed to the study concept and design. Dr. Andrea Cheville and Dr. Jon Tilburt acquired funding for the study. Dr. Sarah Redmond prepared the first draft of this manuscript. All authors contributed to and approved of the final version of this manuscript.
List of Investigators
The Mayo Clinic NOHARM Research Team includes the following authors who provided substantial and equal contributions to this work: Matthew P. Abdel, M.D., Jeffrey Basford, M.D., Raenell Campbell, Robert Cima, M.D., Sue Custhall, APRN, CNS, D.N.P., Sean Dowdy, M.D., Halena Gazelka, M.D., Amanda Glasgow, M.H.A., Elizabeth Habermann, Ph.D., Ian Hargraves, Ph.D., Sarah Harper, Jane Hein, P.T., Jeph Herrin, Ph.D., Michael Hooten, M.D., Lina Ibarra Figueroa, P.T., D.P.T, Amanika Kumar, M.D., Susan Launder, M.S.N, RN, BMT-CN, Aaron L., Leppin, M.D., MSc, Mary McGough, Amanda Nelson, Joel Pacyna, M.A., Karin Pyan, Jewel Podratz, M.B.A., Cathi Rhodes, Marguerite Robinson, M.A., Angela Severson, Mark Stanfield, M.A., Kristi Swanson, M.S., Cindy Tofthagen, Ph.D., and Natalie Wegner.
Disclosures
Dr. Sarah Redmond, Dr. Andrea Cheville, Dr. Jon Tilburt, and the Mayo Clinic NOHARM Study Team have nothing to disclose.
Compliance with Ethics Guidelines
The Mayo Clinic IRB reviewed and approved this protocol (IRB #20-004839). The IRB endorsed waiving individual patient and clinician consent, citing the intervention’s congruence with standard of care, practicability constraints, a robust practice engagement, and written endorsement plan as a substantive alternative authorization. This trial complies with the Helsinki Declaration of 1964 and its amendments.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study. All study data will be kept confidential and conform to strict Mayo Clinic Policy Guidelines for handling protected health information (PHI). Collected data will be stored within Epic until its extraction for analyses at the end of the study. Extracted data will be transferred to Mayo Clinic research servers protected by password and encryption. Identifiable data will only be accessible by IRB-approved study personnel. If the Mayo Clinic IRB, NIA, or other governmental regulatory agencies need to access this data for audits, inspections, or monitoring purposes, access will be granted. Data shared outside the Mayo Clinic firewall will follow all Mayo Clinic guidelines and precautions (removing PHI, de-identification of data, and adding encryption).
Prior Presentation
A version of this protocol and preliminary process data were accepted for presentation at the International Congress on Integrative Medicine and Health, May 23–26, 2020 in Phoenix, AZ.
Author information
Authors and Affiliations
Consortia
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Redmond, S., Mayo Clinic NOHARM Research Team., Tilburt, J. et al. Non-pharmacological Options in Postoperative Hospital-Based and Rehabilitation Pain Management (NOHARM): Protocol for a Stepped-Wedge Cluster-Randomized Pragmatic Clinical Trial. Pain Ther 11, 1037–1053 (2022). https://doi.org/10.1007/s40122-022-00393-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40122-022-00393-x