Abstract
Introduction
As a disorder of the brain in adults and children, traumatic brain injury (TBI) is considered the major cause of mortality and morbidity. As a serious complication of TBI, post-traumatic hydrocephalus (PTH) is commonly identified and significantly associated with neurocognitive impairment, motor dysfunction, and growth impairment. The long-term functional outcomes after shunt dependence are totally not clear.
Methods
This study included 6279 patients between 2012 and 2022. To identify the unfavorable functional outcomes and the PTH-related factors, we carried out univariable logistic regression analyses. To identify the occurrence time of PTH, we conducted the log-rank test and Kaplan–Meier analysis.
Results
Mean patient age was 51.03 ± 22.09 years. Of the 6279 patients with TBI, 327 developed PTH (5.2%). Several PTH development-associated factors, such as intracerebral hematoma, diabetes, longer initial hospital stay, craniotomy, low GCS (Glasgow Coma Scale), EVD (external ventricular drain), and DC (decompressive craniectomy) (p < 0.01), were identified. We also analyzed the factors of unfavorable outcomes after TBI including > 80 years, repeated operations, hypertension, EVD, tracheotomy, and epilepsy (p < 0.01). Ventriculoperitoneal shunt (VPS) itself is not an independent factor of the unfavorable outcome but shunt complication is a strong independent factor of unfavorable outcome (p < 0.05).
Conclusion
We should emphasize the practices that can minimize the risks of shunt complications. Additionally, the rigorous radiographic and clinical surveillance will benefit those patients at high risk of developing PTH.
Trial registration
ClinicalTrials.gov identifier, ChiCTR2300070016.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
As an acute brain damage, in adults and children, traumatic brain injury (TBI) is considered the major cause of mortality and morbidity. Globally, the annual incidence of TBI is estimated at 27–69 million. |
This study identified the PTH predictors after TBI and clarified the functional outcomes after PTH shunt dependence. |
What was learned from the study? |
Although ventriculoperitoneal shunt itself is not an independent factor of the unfavorable outcome, reducing shunt complications is still an important way to improve the prognosis of patients. |
Therefore, we believe that practices for minimizing the risks of shunt complications should be emphasized. Patients with an elevated risk for developing PTH may also benefit from more rigorous clinical and radiographic surveillance. |
Introduction
As the major cause of mortality and morbidity amongst the general population, traumatic brain injury (TBI) is considered as an medico-social issue of importance and usually results in heavy financial burden [1]. As one kind of sequela of TBI, post-traumatic hydrocephalus (PTH) is frequently identified in patients with severe brain trauma. Therefore, to prevent the occurrence of neurological compromise, early treatment and diagnosis of PTH are necessary for patients with recurrent TBI [2].
PTH incidence ranges from 0.7% to 29% [3]. Several factors, such as poor neurological condition, intraventricular hemorrhage (IVH), and acute hydrocephalus, were reported as independent risk factors of the occurrence of hydrocephalus [4]. For example, the chronic hydrocephalus of PTH can be predicted by the decompressive craniectomy [5, 6]. However, the long-term functional outcomes after shunt dependence are totally unclear. This study aimed to (1) define the predictors of shunt-dependent hydrocephalus after TBI and (2) determine the effect of shunt dependence on functional outcomes of patients with TBI.
Methods
Study Design
A comprehensive institutional database was employed to evaluate data of all patients with TBI. The study was registered at clinicaltrials.gov (ChiCTR2300070016). All the enrolled patients were administrated from 2012 to 2022 at a single center. Through direct chart review, we obtained the data. All the information of the enrolled patients was de-identified. The approval of this study was obtained from the institutional review board.
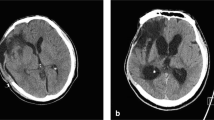
The patients (1) hospitalized for TBI, (2) with sufficient treatment characteristics and baseline clinical information, and (3) having the outcome data about the necessity of a shunt or lack thereof were enrolled in this study. PTH was defined as persistent symptomatic hydrocephalus after TBI that required permanent cerebrospinal fluid (CSF) diversion. Ventricular enlargement (defined as Evans’ index [EI] > 0.3) was required on imaging. Patients with symptoms attributable to ventricular enlargement (new-onset neurological deficits, raised intracranial pressure, and fullness of the scalp defect) were defined to have PTH.
Data and Variables
Imaging, clinical, and demographic data collected at follow-up, during the hospital stay, and at admission were employed in this study. General condition and background disease data include patient age (years), GCS (Glasgow Coma Scale) (3–15), GOS (Glasgow Outcome Scale) (1–5), hypertension, diabetes, coronary heart disease (CHD), and trauma mechanism (motor vehicle accidents, falls, strikes, other); imaging characteristics include whether there was epidural hematoma (epidural hematoma without subdural and intracerebral hematoma), intracranial hemorrhage, subtentorial hemorrhage, intraventricular hemorrhage, subarachnoid hemorrhage (SAH), and open craniocerebral injury occurs; treatment includes whether craniotomy, repeated operations (more than one surgery during the initial hospitalization), DC (decompressive craniotomy), EVD (external ventricular drain), and tracheotomy were performed; hospitalization complications include whether postoperative meningitis, cerebral ischemia, deep venous thrombosis (VET), and epilepsy occurred and initial hospital stay (days).
For patients with DC, we collected the operation-related data including surgical method (bifrontal, unilateral, or bilateral fronto-temporo-parietal craniectomy [FTP]), surgical type (DC with or without evacuation of hematoma), and surgical time (< 24 h or > 24 h). For patients with ventriculoperitoneal shunt (VPS), we collected the time of hydrocephalus development, shunt complications, shunt revision, whether the shunt was placed in initial hospitalization, and 1-year functional outcome since VPS surgery.
Follow-up
For the follow-up, we excluded patients who died during the initial hospitalization. Patients with intact follow-up information were evaluated in this study. The functional outcomes were obtained from clinical notes and hospital records from the local primary care physicians, referring institutions, and study center. At the end of the follow-up, GOS was employed to evaluate the functional outcomes of each patient. At the 1-year follow-up, GOS grade of 4–5 was set as a favorable functional outcome and a GOS grade of 1–3 (such as dead or functionally dependent) was set as an unfavorable functional outcome. For patients with VPS, GOS was followed up for 1 year after VPS surgery.
Ethics Approval and Consent to Participate
During this study, the relevant regulations and guidelines were strictly applied. A named licensing and institutional committee of USTC approved all of our experimental protocols before the initiation of this study. All patients signed a protocol upon admission informing them that clinical data may be included in the study. The data for this study were obtained from the clinical records system at the time of this study. According to the Helsinki Declaration, the informed consent forms were signed by all the enrolled participants before the initiation of this study. The ethical approval number is 2021RE146.
Statistical Analysis
Categorical variables were expressed as frequency whereas continuous variables were expressed as mean ± SD. For the comparison of the continuous variables, Student’s t test was employed. For the comparison of the categorical variables, Fisher’s exact test and Pearson’s χ2 test were conducted. To identify the unfavorable functional outcomes and the PTH-associated factors, we performed univariable logistic regression. Factors with a p value less than 0.20 were further analyzed by multivariable logistic regression. To identify the occurrence time of PTH, we performed Kaplan–Meier analysis and the log-rank test. A p value less than 0.05 was set as the statistical significance threshold. SPSS 26 was applied for the analysis of the collected data.
Results
Study Participants
As shown in Fig. 1, we included 6487 patients with spontaneous TBI in this study from 2012 to 2022 (Fig. 1). Of these patients, 208 were excluded because of incomplete follow-up data or death during initial hospitalization, and 6279 patients were employed to evaluate the long-term functional outcomes. The mean age was 51.03 ± 22.09 years and 4412 were male (70.27%).
Incidence and Prediction Factors of PTH
The etiological details of patients with TBI are summarized in Table 1. The main cause of trauma in our study was motor vehicle accidents (31.31%) and falls (56.27%). Of the 6279 patients with TBI, 327 developed PTH (5.2%) (Table 1).
The characteristics of patients with TBI without or with PTH are compared in Table 2. The mean age of patients was 51.03 ± 22.09. Patients younger than 14 years were more likely to have PTH (p < 0.05). Patients with PTH were more likely to have low GCS (9.19 ± 3.78 vs 11.10 ± 3.54, p < 0.01), diabetes (6.42% vs 3.36%, p < 0.05), intracerebral hematoma (64.83% vs 55.91%, p < 0.01), subtentorial hemorrhage (6.42% vs 2.71%, p < 0.01), intraventricular hemorrhage (3.36% vs 1.13%, p < 0.01), undergo craniotomy (57.19% vs 29.02%, p < 0.01), repeated operations (13.15% vs 5.80%, p < 0.01), EVD placement (22.63% vs 1.55%, p < 0.01), DC (36.70%, 12.03, p < 0.01), postoperative meningitis (0.66% vs 2.75%, p < 0.01), cerebral ischemia (8.24% vs 4.59%, p < 0.05), and longer initial hospital stay (24.31 ± 19.94 vs 16.54 ± 20.41, p < 0.01) (Table 2).
Details of the PTH predictors after TBI are summarized in Table 3. According to multivariable analysis, significant low GCS (p < 0.01), diabetes (p < 0.01), intracerebral hematoma, DC (p < 0.01), EVD (p < 0.01) placement, and longer initial hospital stay (p < 0.01) were observed. After DC (odds ratio [OR] 2.578), EVD presence (OR 13.392) can be used as the strongest independent predictor for shunt dependence. Furthermore, only epidural hematoma tends to be a significant protective factor (OR 2.046) (Table 3).
Table 4 compares the characteristics of patients with PTH without or with EVD placement. Of 327 patients with PTH, 74 (22.62%) of them underwent EVD during the initial hospitalization.
During the initial hospitalization, the patients with shunt-dependence and subjected to EVD placement were more likely to have a lower GCS score at presentation (mean 7.27 ± 2.78 vs 9.75 ± 3.85; p < 0.01), subtentorial hemorrhage (14.86% vs 3.95%; p < 0.01), intraventricular hemorrhage (9.46% vs 1.58%, p < 0.01), SAH (45.45% vs 27.03%, p < 0.01), postoperative meningitis (8.11% vs 1.19%, p < 0.01), longer initial hospital stay (35.81 ± 25.76 vs 20.95 ± 16.50, p < 0.01), and to undergo repeated operations (25.68% vs 9.49%, p < 0.01) and tracheotomy (36.49% vs 16.21%, p < 0.01).
Table 5 compares the characteristics of patients with PTH without or with DC. During the initial hospitalization, a DC was performed in 836 patients with TBI and 74 (44.58%) of them eventually underwent shunt placement. Of 327 patients with PTH, 120 (36.69%) of them underwent EVD.
The patients with shunt-dependence and who underwent DC were more likely to be older (12.50% vs 4.37%, p < 0.05), were more likely to have a lower GCS score at presentation (mean 6.53 ± 2.45 vs 10.72 ± 3.56; p < 0.01), were less likely to have intracerebral hematoma (1.67% vs 4.35%, p < 0.01), were more likely to undergo repeated operations (30.00% vs 3.38%, p < 0.01) and tracheotomy (39.17% vs 10.14%, p < 0.01), and were more likely to have postoperative epilepsy (11.67% vs 3.38%, p < 0.01) and longer initial hospital stay (29.62 ± 22.22 vs 21.24 ± 17.84, p < 0.01).
Table 6 compares the characteristics of the patients without or with VPS who underwent DC during the initial hospitalization. Shunt-dependent patients were more likely have an unfavorable GOS (1–3) on admission (27.81% vs 12.5%, p < 0.01). Surgical method (bifrontal, unilateral FTP, or bilateral FTP), surgical type (DC with or without evacuation of hematoma), and surgical time (< 24 h or > 24 h) showed no significant differences.
Time Survival Analysis of PTH
According to the above research results, the patients were subdivided into different subgroups including GOS 1–3 vs GOS 4–5, diabetes vs no diabetes, intracerebral hematoma vs no intracerebral hematoma, EVD vs no EVD, DC vs no DC, and craniotomy vs no craniotomy. The corresponding Kaplan–Meier curves for these subgroup analyses are shown in Fig. 2. Log-rank tests showed a significant difference in all subgroups (p < 0.01).
Functional Outcomes in Patients with TBI
Table 7 compares the characteristics of shunt-dependent patients with TBI according to unfavorable and favorable outcomes. There were 3813 (55.7%) patients with favorable outcomes (GOS 4–5) and 2466 (44.3%) patients with unfavorable (GOS 1–3) outcomes. Those with favorable outcomes had less VPS placement (3.3% vs 8.1%; p < 0.01), shorter initial hospital stay (mean 14.83 ± 20 vs 20 ± 29.12 days; p < 0.01), were less likely to have low GCS (7.26 ± 2.37 vs 13.43 ± 1.57, p < 0.01), were less likely to be over 80 years old (6.56% vs 8.27%; p < 0.05), were less likely to have diabetes (5.77% vs 7.02%, p < 0.05) and hypertension (12.51% vs 15.90%, p < 0.01) , were less likely to have an intracerebral hematoma (0.45% vs 2.47%, p < 0.01) and SAH (37.84% vs 46.55%, p < 0.01), were less likely to undergo repeated operations (2.62% vs 11.68%, p < 0.01), EVD placement (1.05% vs 5.11%, p < 0.01), DC (3.51% vs 23.44%, p < 0.01), and tracheotomy (7.08% vs 36.24%, p < 0.01), were less likely to have postoperative meningitis (0.61% vs 1.97%, p < 0.01), VET (1.42% vs 4.49%, p < 0.01), and epilepsy (4.29% vs 8.71%, p < 0.05).
The details of the unfavorable outcomes-related factors after TBI are summarized in Table 8. Multivariable analysis revealed a significant trend of low GCS (p < 0.01), age over 80 years (p < 0.01), DC (p < 0.01), EVD placement (p < 0.01), tracheotomy (p < 0.01), and hypertension (p < 0.01) After repeated operations (OR 2.199), tracheotomy (OR 7.219) can be used to predict the unfavorable outcomes strongly and independently. VPS was not an independent predictor of unfavorable outcomes.
Follow-up was available for 115 patients with PTH and VPS was performed at our center at a mean duration of 24.3 months. Shunt complication occurs in 17 of these patients and four underwent revision surgery.
Functional Outcomes in Patients with PTH
Table 9 compares the characteristics shunt-dependent patients with VPS according to unfavorable or favorable outcomes. There were 71 (61.7%) patients with favorable outcomes (GOS 4–5) and 44 (38.3%) patients with unfavorable (GOS 1–3) outcomes. Those with favorable outcomes had fewer VPS complications (8.45% vs 25.00%; p < 0.05), less VPS revision (0.00% vs 9.09%; p < 0.05), and higher GCS (11.28 ± 3.46 vs 8.82 ± 4.50, p < 0.01). The age, gender, and whether the shunt was placed in initial hospitalization were not significantly different between the two groups (p > 0.05).
The details of the predictors for unfavorable (GOS 1–3) outcomes in patients with PTH are summarized in Table 10. Multivariable analysis revealed a significant trend of low GCS (p < 0.05) and shunt complications (p < 0.05).
Discussion
In line with the previous reports [7,8,9], we observed a 5.2% shunt dependency rate. For the shunt dependency, many independent risk factors, such as DC, EVD, low GCS, craniotomy, longer initial hospital stay, diabetes, and intracerebral hematoma, were identified (p < 0.01). Epidural hematoma (without subdural and intracerebral hematoma) tends to be a significant protective factor (p < 0.01).
EVD represents the development of acute hydrocephalus. The factors leading acute hydrocephalus to become chronic hydrocephalus have been discussed mostly in aneurysmal SAH and less so in TBI [10,11,12,13]. In this study, EVD was identified as a strong independent factor for the prediction of shunt dependence after TBI (p < 0.01, OR 13.392). Therefore, we identified the difference of the shunt-dependent patients without and with EVD placement. As expected, a high percentage of EVD placement was observed in those patients with worse baseline clinical status, such as lower GCS score, longer initial hospital stay, tracheotomy, and imaging findings (i.e., subtentorial hemorrhage, SAH, intraventricular hemorrhage). Postoperative meningitis, which may be caused by EVD or repeated operations, indicated that the infection is closely related to hydrocephalus. This also suggests that reducing EVD infection may be an important way to reduce PTH.
The relationship between DC and PTH has been widely discussed [14,15,16,17]. It is believed that the impaired venous drainage into the sagittal sinus, loss of pulsatile intracranial CSF dynamics, and the disruption of CSF drainage due to arachnoid adhesions in the basal cisterns are causative factors [18]. In this study, the difference of the shunt-dependent patients without and with DC was identified. We observed that a high percentage of DC happens in those patients with a worse baseline clinical status (p < 0.01), while the occurrence of hydrocephalus does not seem to be related to the DC procedures. Currently, the effect of DC on hydrocephalus is also not clear [19, 20]. DC may result in many complications, such as subdural effusion, infection, CSF leakage through the scalp incision, herniation of the cortex through a bone defect, epilepsy, and hematoma expansion or contusion, which may influence the result. However, our research indicates that the main cause of PTH could be primary severe craniocerebral trauma that requires DC rather than DC surgery itself.
Most hydrocephalus were observed 1–3 months after the surgery and the onset time may be related to the patient’s prognosis [21]. According to the above research results, we looked at the survival curve of hydrocephalus in the different subgroups. Patients with GOS 4–5, diabetes, intracerebral hematoma, EVD, DC, and craniotomy had a high rate of PTH.
Moreover, the connection between PTH and the functional outcomes was also evaluated here. In patients with aneurysmal SAH, shunt dependency was identified as a unfavorable outcome-associated, independent, and strong variable [22]. In patients with TBI, the role of shunt dependency in the functional status has not been not extensively studied. In our study, VPS is significantly different between favorable and unfavorable outcomes. Nevertheless, the significance was not observed in the multivariable logistic regression. The unfavorable outcome was frequently observed in patients with poorer baseline clinical status, such as > 80 years, repeated operations, hypertension, EVD, tracheotomy, and epilepsy. However, as a result of death of more seriously ill patients or the appearance of irreversible brain function damage before the onset of hydrocephalus, this connection might be confounded [23].
Of 115 patients who received VPS in our center, shunt complication occurred in 17 patients (14.7%) and 4 patients (3.4%) underwent shunt revision. The occurrence of shunt complications was a strong independent factor of unfavorable outcomes. Therefore we believe the impact of VPS may come from VPS complications. A study of 17,035 patients who underwent VPS surgery reported a 23.8% complication rate during a mean follow-up of 3.9 (± 1.8) years [24]. Another multicenter research study showed that 861 of 5092 VPS failed within 90 days and overall about a third of early failures are potentially preventable [25].
For the patient with TBI, the initial cerebral damage is often decisive. After TBI, secondary hydrocephalus can be caused by the deposition of the hemorrhage over the subarachnoid space surface or by the extension of the hemorrhage into the ventricular system. Therapeutic measures such as DC and ETV are often associated with PTH but were also necessary at the time. Some related therapeutic strategies of IVH- and SAH-associated hydrocephalus may be valuable in the treatment of TBI [22]. However, the development and application of the practices to minimize the risk of shunt complications should receive more attention.
To prevent damage to the periventricular temporal brain, it is particularly important to determine ventricular enlargements as early as possible, well before EI becomes positive. Unlike primary hydrocephalus, a very sensitive sign of secondary ventricular enlargement is the dilatation of the temporal horns and posterior horns [26]. Moreover, the width of the third ventricle increases so that it is no longer slit-shaped but rather ballooned or laterally bowed. Callosal angle is also a recent imaging factor that has been suggested to be associated with hydrocephalus [27]. Cella media ratio and frontal horn ratio are also well-used indexes [28]. Joint measures of frontal distances, temporal horn widths, and other relevant indicators should be performed routinely in neuroimaging analyses to facilitate the rapid diagnosis and treatment of acute or subacute secondary ventricular enlargement.
Limitations
This study has several limitations. The referral, treatment, and selection biases of its physicians and the institution exist because all the patients came from a single center, although we accrued a large cohort of patients with TBI. Additionally, some of the patients (8%) were lost to follow-up. However, of 327 patients with PTH, only 115 (35%) received the VPS placement and were followed up in our center.
Conclusion
This study identified several factors for the development of PTH and for unfavorable outcomes after TBI. VPS itself is not an independent factor of the unfavorable outcome but shunt complications are a strong independent factor for the unfavorable outcome. Therefore, we should emphasize the practices to minimize the shunt complications risks. The rigorous radiographic and clinical surveillance will benefit those patients at high risk of developing PTH.
References
Maas AIR, Menon DK, Adelson PD, et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987–1048.
Guyot LL, Michael DB. Post-traumatic hydrocephalus. Neurol Res. 2000;22(1):25–8.
Matsushita H, Takahashi K, Maeda Y, et al. A clinical study of posttraumatic hydrocephalus. No Shinkei Geka Neurol Surg. 2000;28(9):773–9.
Kammersgaard LP, Linnemann M. Hydrocephalus following severe traumatic brain injury in adults, incidence, timing, and clinical predictors during rehabilitation. NeuroRehabilitation. 2013;33(3):473–80.
Mavrovounis G, Kalogeras A, Brotis A, et al. Incidence of post-traumatic hydrocephalus in traumatic brain injury patients that underwent DC versus those that were managed without DC: a systematic review and meta-analysis. Brain Spine. 2021;1:100303.
Fattahian R, Reza Bagheri S, Sadeghi M. Development of posttraumatic hydrocephalus requiring ventriculoperitoneal shunt after decompressive craniectomy for traumatic brain: injury a systematic review and meta-analysis of retrospective studies. Med Arch. 2018;72(3):214–9.
De Bonis P, Anile C. Post-traumatic hydrocephalus: the Cinderella of Neurotrauma. Expert Rev Neurother. 2020;20(7):643–6.
Lalou AD, Levrini V, Czosnyka M, et al. Cerebrospinal fluid dynamics in non-acute post-traumatic ventriculomegaly. Fluids Barriers CNS. 2020;17(1):24.
Merkler AE, Ch’ang J, Parker WE, et al. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017;98:654–8.
Yang TC, Chang CH, Liu YT, et al. Predictors of shunt-dependent chronic hydrocephalus after aneurysmal subarachnoid hemorrhage. Eur Neurol. 2013;69(5):296–303.
Sanusi TD, McLarnon M, Abouharb A. Risk factors of chronic shunt dependent hydrocephalus following aneurysmal subarachnoid hemorrhage. Clin Neurol Neurosurg. 2020;198: 106095.
Hao X, Wei D. The risk factors of shunt-dependent hydrocephalus after subarachnoid space hemorrhage of intracranial aneurysms. Medicine (Baltimore). 2019;98(27):e15970.
Lenski M, Biczok A, Huge V, et al. Role of cerebrospinal fluid markers for predicting shunt-dependent hydrocephalus in patients with subarachnoid hemorrhage and external ventricular drain placement. World Neurosurg. 2019;121:e535–42.
Faleiro RM, Faleiro LC, Caetano E, et al. Decompressive craniotomy: prognostic factors and complications in 89 patients. Arq Neuropsiquiatr. 2008;66(2B):369–73.
De Bonis P, Sturiale CL, Anile C, et al. Decompressive craniectomy, interhemispheric hygroma and hydrocephalus: a timeline of events? Clin Neurol Neurosurg. 2013;115(8):1308–12.
Vedantam A, Yamal JM, Hwang H, et al. Factors associated with shunt-dependent hydrocephalus after decompressive craniectomy for traumatic brain injury. J Neurosurg. 2018;128(5):1547–52.
Kim H, Lee HS, Ahn SY, et al. Factors associated postoperative hydrocephalus in patients with traumatic acute subdural hemorrhage. J Korean Neurosurg Soc. 2017;60(6):730–7.
Waziri A, Fusco D, Mayer SA, et al. Postoperative hydrocephalus in patients undergoing decompressive hemicraniectomy for ischemic or hemorrhagic stroke. Neurosurgery. 2007;61:489–94.
Wang QP, Ma JP, et al. Impact of operation details on hydrocephalus after decompressive craniectomy. Neurosciences. 2016;21(1):10–6.
Ding J, Guo Y, Tian H, et al. The influence of decompressive craniectomy on the development of hydrocephalus: a review. Arq Neuropsiquiatr. 2014;72(9):715–20.
Fotakopoulos G, Tsianaka E, Siasios G et al. Posttraumatic hydrocephalus after decompressive craniectomy in 126 patients with severe traumatic brain injury. J Neurol Surg Cent Eur Neurosurg. 2016;77(2):88–92.
Paisan GM, Ding D, Starke RM, et al. Shunt-dependent hydrocephalus after aneurysmal subarachnoid hemorrhage: predictors and long-term functional outcomes. Neurosurgery. 2018;83(3):393–402.
Merkler AE, Ch’ang J, Parker WE, et al. The rate of complications after ventriculoperitoneal shunt surgery. World Neurosurg. 2017;98:654–8.
Abuhadi M, Alghoribi R, Alharbi LA, et al. Predictors and outcome of ventriculoperitoneal shunt infection: a retrospective single-center study. Cureus. 2022;14(7):e27494.
Dave P, Venable GT, Jones TL, et al. The preventable shunt revision rate: a multicenter evaluation. Neurosurgery. 2019;84(3):788–98.
Missori P, Paolini S, Peschillo S, et al. Temporal horn enlargements predict secondary hydrocephalus diagnosis earlier than Evans’ index. Tomography. 2022;8:1429–36.
Gholipour A, Akhondi-Asl A, Estroff JA, Warfield SK. Multi-atlas multi-shape segmentation of fetal brain MRI for volumetric and morphometric analysis of ventriculomegaly. Neuroimage. 2012;60(3):1819–31.
Lee W, Lee A, Li H, et al. Callosal angle in idiopathic normal pressure hydrocephalus: small angular mal-rotations of the coronal plane affect measurement reliability. Neuroradiology. 2021;63(10):1659–67.
Acknowledgements
The study was pre-registered at clinicaltrials.gov (ChiCTR2300070016). 1. The analysis plan was registered prior to beginning data collection at the Center for Open Science (https://www.cos.io/initiatives/prereg). 2. To develop a model, 6000 samples were employed and a > 90% prognostic accuracy (primary clinical outcome) with a p value < 0.01 was yield. 3. We screened a total of 7028 participants, selected 6484 participants, and obtained the data from 6279 participants. 4. The evaluation of the prognosis was not told to the participants. Team members blinded to the participants’ characteristics were employed to conduct the adjudications and final clinical outcome assessments. 5. All surveys and questionnaires used to develop prognostic models are available from the authors. 6. The evaluations of outcome and the key criteria of sample inclusion were conducted and established according to the standards. 7. As part of this study, the study group also performed the replication.
Funding
Project 82101424 is supported by NSFC. The journal’s rapid service fee was funded by the authors.
Medical Writing and/or Editorial Assistance
The authors acknowledge Topedit for providing medical writing assistance in the development of this manuscript. This was funded by the authors.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Hao Xu concepted the study. Hao Xu collected the data, Xiangpin Wei, Dejun Bao, and Yongfei Dong, evaluated and conducted the surgical procedures. Hao Xu analyzed the data and wrote the manuscript. Chaoshi Niu and Xinfeng Liu reviewed and edited the manuscript.
Disclosures
Hao Xu, Yongfei Dong, Dejun Bao, Xiangpin Wei, Chaoshi Niu and Xinfeng Liu have no competing interest to disclose.
Compliance with Ethics Guidelines
The study was pre-registered at clinicaltrials.gov (ChiCTR2300070016). During this study, the relevant regulations and guidelines were strictly applied. A named licensing and institutional committee of USTC approved all of our experimental protocols before the initiation of this study. All patients signed a protocol upon admission informing them that clinical data may be included in the study. The data for this study were obtained from the clinical records system at the time of this study. According to the Helsinki Declaration, the informed consent forms were signed by all the enrolled participants before the initiation of this study. The ethical approval number is 2021RE146.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xu, H., Dong, Y., Bao, D. et al. Shunt-Dependent Post-Traumatic Hydrocephalus: Predictors and Long-Term Functional Outcomes. Neurol Ther 12, 1607–1622 (2023). https://doi.org/10.1007/s40120-023-00511-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40120-023-00511-7