Abstract
Introduction
Tafamidis is the first drug approved by the European Commission for the treatment of wild-type or hereditary transthyretin amyloid cardiomyopathy (ATTR-CM) in adults to reduce cardiovascular mortality and cardiovascular-related hospitalization. Real-world treatment patterns of tafamidis 61 mg in Germany are not well studied in patients with ATTR-CM.
Methods
This was a non-interventional, retrospective, observational cohort study of adult patients in Germany based on the IQVIA pharmacy claims database (IQVIA™ LRx). Patients included in the analysis were statutory insured and received at least one prescription of tafamidis 61 mg between March 1, 2020 and August 31, 2022. Treatment adherence was analyzed using the modified medical possession ratio (mMPR) and proportion of days covered (PDC).
Results
Overall, 1565 adult patients received at least one tafamidis prescription in the study period. Their mean age was 78.3 years, 82.4% were male, and 23.2% were treated by a cardiologist. Persistency rates for patients treated with tafamidis 61 mg were high: 78.0% for 12 months and 65.1% for 24 months after treatment initiation. Patients also had high adherence rate on filling their prescriptions on time: 94.6% and 90.5% of patients had adherence rates of at least 80%, measured by mMPR and PDC, respectively.
Conclusions
In the IQVIA™ LRx database, patients prescribed tafamidis 61 mg in Germany displayed high adherence and persistency rates, which suggest good drug tolerability and ease of use.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Tafamidis 61 mg is the first drug to be approved by the European Commission for the treatment of transthyretin amyloid cardiomyopathy (ATTR-CM) in adults to reduce cardiovascular mortality and cardiovascular-related hospitalization. |
To our knowledge, this retrospective study is the first in Europe to assess medication adherence in patients with ATTR-CM in a real-world setting to provide additional insights into the prescribing and usage patterns of patients prescribed tafamidis 61 mg. |
What was learned from the study? |
Of all patients in the IQVIA™ LRx database included in this study, 94.6% and 90.5% had an adherence rate ≥ 80% for both modified medical possession ratio and proportion of days covered, respectively. |
The high rates of adherence and persistency (65% after 24 months) in patients prescribed tafamidis 61 mg in Germany suggest good drug tolerability and ease of use, which are important factors for disease management. |
Findings from this study showed changes in concomitant medication before and during tafamidis treatment (e.g., a decrease in beta-blocking agents), suggesting potential opportunities for optimizing guideline-recommended concomitant medication in tafamidis-treated patients with ATTR-CM. |
Introduction
Systemic amyloidosis is a rare family of diseases caused by misfolded or misassembled proteins that form amyloid fibrils in various tissues and organs [1, 2]. The specific precursor protein that misfolds to form amyloid fibrils defines the amyloid type and predicts the patient’s clinical course [3]. Cardiac involvement in amyloidosis results in progressive deterioration of diastolic and systolic dysfunction, congestive heart failure, and death [4]. Treatment of cardiac amyloidosis depends on the amyloid type and degree of involvement. Two of the most common types of cardiac amyloidosis are light chain (AL) and transthyretin amyloidosis.
Pivotal clinical data showed tafamidis meglumine is superior to placebo in reducing the combination of all-cause mortality and cardiovascular-related hospitalizations [5]. Tafamidis 61 mg is the first drug to be approved by the European Commission for the treatment of wild-type or hereditary transthyretin amyloid cardiomyopathy (ATTR-CM) to reduce cardiovascular mortality and cardiovascular-related hospitalization in adults. On February 18, 2020, the European Commission approved the tafamidis 61 mg capsule formulation for treatment of adult patients with ATTR-CM. The recommended dosage is either tafamidis 80 mg (four 20-mg tafamidis meglumine capsules) orally once daily (QD) or tafamidis 61 mg (one 61-mg tafamidis capsule) orally QD. In Germany, tafamidis can be prescribed by a physician who specializes in treating amyloidosis or cardiomyopathy.
Real-world evidence (RWE) is useful to describe characteristics of patients in a clinical practice population, which is likely to be more heterogeneous compared with a clinical trial [6]. RWE provides data on a more generalizable population by including patients typically underrepresented or excluded from clinical trials due to sex, race, ethnicity, characteristics of the disease, or other treatments.
Given the relatively recent approval of tafamidis and low overall prevalence of ATTR-CM (up to 1700 adult patients in Germany in 2020), there is limited RWE describing the characteristics of patients on these therapies and medical specialties of the prescribing physicians [7]. Additionally, medication adherence in cardiovascular disease is an important surrogate endpoint to demonstrate the impact on the burden on the healthcare system [8, 9].
To our knowledge, this is the first retrospective study utilizing RWE to assess medication adherence in patients with ATTR-CM in Germany and to provide additional insights into the prescribing and usage patterns of patients who are prescribed tafamidis 61 mg QD.
Methods
Data Source
All analyses were conducted with the German IQVIATM LRx database, which includes longitudinal patient-level prescription data of patients with statutory health insurance (SHI) [1]. The IQVIATM LRx database accesses nationwide pharmacy data collection centers that process prescription data for all German patients within the SHI system for reimbursement purposes. It is based on computerized records derived from pharmacy coding centers for public sick fund prescriptions (no private or cash prescriptions are covered), and in 2021 it covered approximately 80% of the total SHI prescription amount in Germany [10]. All patient information is fully anonymized by the data provider in accordance with data privacy laws. The de-identified patient-level data include dispensed drugs (e.g., brand, substance, package size, and product form) and associated information (e.g., specialty of prescriber, region identifier), as well as patient-level information such as patient age and sex. The collected data contain all Anatomical Therapeutic Chemical [] codes and prescriber specialties, including outpatient centers and authorized physicians in hospitals; therefore, the database provides a holistic view of outpatient treatments received by a patient. Finally, this database has been used effectively in previous studies on persistence [11, 12].
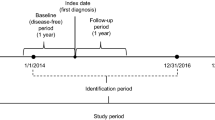
Study Design and Cohort
This study is a non-interventional, retrospective, observational cohort study of German longitudinal prescription data. Included patients were statutory insured, 18 years or older, and received at least one prescription of tafamidis 61 mg between March 1, 2020 and August 31, 2022 (index period). Treatment adherence was analyzed in patients with at least two tafamidis 61 mg prescriptions during the index period.
Patients included in the persistency analysis were sampled up to April 30, 2022, to allow for sufficient time to collect data on therapy. The selection of study cohorts for the different analyses is shown in Fig. 1.
Ethical Approval
The database used for this study includes only anonymized data in compliance with the provisions set forth in the applicable data protection laws. German law allows the use of anonymous electronic medical records for research purposes under certain conditions. In accordance with this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Since all patients were only queried as aggregates and no protected health information was available for queries, no institutional review board approval was required for the use of this database or the completion of this study. IQVIA was contracted by Pfizer in connection with this study. Pfizer did not have permission to access the IQVIATM LRx database at any time during the study, but rather received aggregated results from the database.
Outcomes and Analysis Details
The primary objective of this study was to describe tafamidis 61 mg treatment patterns (i.e., treatment initiation, days of supply, adherence rates, and persistence) among patients with ATTR-CM. The secondary objectives were to analyze demographic characteristics of patients, such as patient age and sex, and to evaluate concomitant medications of patients dispensed prescriptions of tafamidis 61 mg QD.
In this study, the following analyses were conducted: (1) adherence analysis using the modified medical possession ratio (mMPR) and using the proportion of days covered (PDC) method; (2) concomitant medication analysis using McNemar’s test to compare medication prior to and during tafamidis 61 mg treatment; and (3) persistency analysis using the Kaplan–Meier method.
All three analyses utilized IQVIATM LRx data collected up to August 2022. The baseline patient characteristics were assessed descriptively. Adherence was analyzed by using two methods: the mMPR (calculated as the sum of the days’ supply for all prescription fills in the time period divided by the number of days in the time period), which allows for stockpiling so that adherence can go over 1, and PDC (calculated as the sum of days covered over the time period divided by the number of days in the time period), in which patients are classified as adherent based on mMPR/PDC greater than or equal to 80%. Mean, median, standard deviation (SD), and 25th and 75th percentiles were additionally calculated for both methods.
Concomitant medication use was analyzed using the McNemar’s test to compare patient numbers before the first tafamidis 61 mg prescription and during tafamidis 61 mg treatment.
Persistency was calculated using the Kaplan–Meier method allowing for both 90-day and 60-day prescription gaps. A subcohort of these patients was observable for at least 12 months after the first tafamidis 61 mg prescription and used as sensitivity analysis. P values < 0.05 were considered statistically significant. Analyses were carried out using SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Baseline Characteristics
In total, 1565 adult patients received tafamidis 61 mg between March 1, 2020 and August 31, 2022. The baseline characteristics of the study patients are shown in Table 1. Of all adult patients included, 840 (53.7%) were aged 80 years or older (mean age, 78.3 years) and 1290 (82.4%) patients were male. Mean treatment duration was 12.1 months and mean days of tafamidis supply were 411.6 days or 13.5 months. The majority (49.8%) of patients were treated in outpatient centers, which often are found at university hospitals and did not involve overnight stays. The specialty of the physicians is unknown in the dataset.
Patient Adherence
Descriptive statistics of adherence to tafamidis 61 mg treatment and the distribution of patient adherence, respectively, for differing adherence measures are shown in Table 2 and Fig. 2. Among 1439 patients who received at least two prescriptions of tafamidis 61 mg within the study time period, the mean mMPR was 1.02 (SD 0.48), and mean PDC was 0.89 (SD 0.12). Overall, 94.6% of patients had an adherence rate of at least 80% for mMPR, and 90.5% of patients had an 80% or higher adherence for PDC.
Concomitant Medication Prior to and During Tafamidis Treatment
The results of medications prior to and during tafamidis 61 mg medication are listed in Table 3. The four most-prescribed drug classes were loop diuretics (73.0%), beta-blocking agents (61.3%), direct factor Xa inhibitors (59.1%), and statins (52.7%). Significant decreases in prescription frequency of beta-blocking agents (P < 0.0001) and statins (P = 0.0005) were found. However, direct factor Xa inhibitor prescriptions were more frequent during than before tafamidis 61 mg treatment (P < 0.0001). Loop diuretics showed no significant differences between the analyzed time periods (P = 0.1201). The same trends were found when restricting data to 1-year follow-up after the first tafamidis 61 mg prescription.
Patient Persistency
Results of the adherence analysis for a 90-day and 60-day allowable gap between end of supply and subsequent tafamidis 61 mg prescriptions are shown in Fig. 3, and detailed results of patient persistency with a 90-day gap are shown in Table 4. In total, 1368 patients were included in the persistency analysis. In the 90-day gap, 78.0% of patients remained on tafamidis 61 mg after 12 months and 65.1% of patients remained after 24 months. In the 60 day-gap, 76.5% and 62.3% of patients remained on tafamidis 61 mg after 12 months and 24 months, respectively. For the 90-day prescription gap, patients remaining at risk decreased by more than half (from 1368 to 645 patients) within 1 year of therapy. After 24 months, only 170 patients remained at risk.
The sensitivity analysis of patients who were observable for at least 12 months in the IQVIATM LRx database after initiation of tafamidis 61 mg resulted in a persistence rate of 86.3% after 12 months and 72.2% at 24 months for the 90-day gap, which were both higher than the base case.
Discussion
The present retrospective study of longitudinal prescription data in Germany showed that tafamidis 61 mg patients were, on average, 78.3 years old and 82.4% were male. A previously conducted US Medicare real-world study on tafamidis for patients with ATTR-CM found very similar patient characteristics in the USA. In that study, the mean age was 75 years and 83.2% of the included patients were male [14]. Similarly, another claims study that analyzed ATTR-CM incidence and prevalence in France found a slightly lower proportion of male patients (66.9%) and a numerically higher mean age of 81 years at diagnosis [15].
The current study found patient adherence rates of over 90% for both calculation methods. The mMPR was 94.6%, similar to the mMPR of 96% and 92% in a Japan and US study of patients treated with tafamidis, respectively [1, 14]. These patient adherence rates are higher than the estimated 57% reported in a meta-analysis for other cardiovascular drugs [16]. Since ATTR-CM is a severe and progressive disease, early and continuous management is of high importance [5, 17]. Poor adherence rates lead to a lower efficacy and worse outcomes regarding quality of life and increased healthcare costs [14].
To our knowledge, this study is the first in Europe to study treatment persistence of tafamidis 61 mg patients in a real-word setting. The results of this study showed a high and similar persistence rate for both allowable treatment gaps. After 12 months, 78.0% of the patients remained on tafamidis 61 mg and 65.1% remained after 24 months. This percentage of patients remaining on tafamidis 61 mg is considerably high compared with other studies. For example, a study evaluating the persistence of several antihypertensive treatments showed that, at 39% after 1 year and 28% after 2 years, angiotensin II receptor blockers had the highest persistence rate compared with other treatments [18]. As persistency is an indicator of drug safety and ease of use, it is an important factor for disease management. Aligned with published clinical data, these results suggest that tafamidis 61 mg is well tolerated by patients included in this study [19]. The daily dose of one capsule may also have contributed to the high persistency rate.
In this study, we observed changes in concomitant medication when comparing prior to treatment with during treatment with tafamidis 61 mg. Specifically, a decrease in beta-blocking agents compared with their use prior to tafamidis initiation was noted. Beta-blocking agents are not recommended for patients with ATTR-CM as their use can lead to hypotension, fatigue, and worsening of bradyarrhythmia and are often poorly tolerated [13, 20, 21]. Therefore, a decrease from 67.8% prior treatment to 61.3% during tafamidis 61 mg therapy is a significant (P < 0.0001) decrease in prescriptions. However, following the current guidelines, this number remains high and shows opportunities for improvement [20]. The significant increase in direct factor Xa inhibitors (from 55.0% to 59.1%) is expected and recommended as it is prescribed to prevent symptoms common to patients with ATTR-CM [13, 20]. Loop diuretics, which are frequently used to manage heart failure in patients with ATTR-CM, showed no statistically significant changes during tafamidis treatment [21]. As patients who require diuretics have a worse prognosis in terms of hospitalization and mortality compared with patients without need for treatment with diuretics, an increase in loop diuretics can be used as an indicator of disease progression [22]. Thus, the absence of an increase in loop diuretics suggests stability in those patients.
This study has limitations due to the general limitations of the IQVIATM LRx database and the nature of the disease. For this dataset, patients are from SHI alone, and no information is available on diagnosis, indications, clinical parameters, laboratory data, or inpatient hospital data. Therefore, we conducted the sensitivity analysis on persistency with patient’s post observable to account for patient dropoffs in the database. Also, as ATTR-CM is a rare disease that clinically manifests with symptoms similar to other diseases, misdiagnoses could not be ruled out [23]. Moreover, many patients with ATTR-CM were identified in the outpatient sector, for which no further detailed information on prescriber specialties is available. Other limitations include the incomplete coverage of all pharmacies in Germany and a lack of continuous enrollment. Furthermore, there is a risk of selection bias as study samples obtained from claims data are not randomly selected.
Conclusions
Patients with ATTR-CM who were prescribed tafamidis 61 mg in Germany displayed high adherence rates, thus confirming results of an earlier study in the USA. Furthermore, we found high treatment persistency rates in these patients, which suggests good drug tolerability and ease of use.
On the basis of professional society recommendations and using real-world data, we identified opportunities for concomitant medication optimization in patients with ATTR-CM treated with tafamidis 61 mg QD.
Data Availability
The datasets analyzed during the current study are not publicly available but will be made available on reasonable request.
References
Kato T, Ines M, Minamisawa M, et al. Tafamidis medication adherence and persistence in patients with transthyretin cardiac amyloidosis (ATTR-CM) in Japan. ESC Heart Fail. 2024. In press.
Lachmann HJ, Hawkins PN. Systemic amyloidosis. Curr Opin Pharmacol. 2006;6:214–20. https://doi.org/10.1016/j.coph.2005.10.005.
Sipe JD, Benson MD, Buxbaum JN, et al. Nomenclature 2014: amyloid fibril proteins and clinical classification of the amyloidosis. Amyloid. 2014;21:221–4. https://doi.org/10.3109/13506129.2014.964858.
Dubrey SW, Hawkins PN, Falk RH. Amyloid diseases of the heart: assessment, diagnosis, and referral. Heart. 2011;97:75–84. https://doi.org/10.1136/hrt.2009.190405.
Maurer MS, Schwartz JH, Gundapaneni B, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379:1007–16. https://doi.org/10.1056/NEJMoa1805689.
Hall PS. Real-world data for efficient health technology assessment. Eur J Cancer. 2017;79:235–7. https://doi.org/10.1016/j.ejca.2017.04.003.
Gemeinsamen Bundesausschuss (G-BA). [Beschluss - des Gemeinsamen Bundesausschusses über eine Änderung der Arzneimittel-Richtlinie (AM-RL): Anlage XII – Nutzenbewertung von Arzneimitteln mit neuen Wirkstoffen nach § 35a SGB V Tafamidis (neues Anwendungsgebiet: Amyloidose bei Kardiomyopathie)]. 2020. https://www.g-ba.de/downloads/39-261-4421/2020-08-20_AM-RL-XII_Tafamidis_D-510_BAnz.pdf. Accessed Nov 1, 2023.
Piña IL, Di Palo KE, Brown MT, et al. Medication adherence: importance, issues and policy: a policy statement from the American Heart Association. Prog Cardiovasc Dis. 2021;64:111–20. https://doi.org/10.1016/j.pcad.2020.08.003.
Leslie KH, McCowan C, Pell JP. Adherence to cardiovascular medication: a review of systematic reviews. J Public Health (Oxf). 2019;41:e84–94. https://doi.org/10.1093/pubmed/fdy088.
Richter H, Dombrowski S, Hamer H, Hadji P, Kostev K. Use of a German longitudinal prescription database (LRx) in pharmacoepidemiology. Ger Med Sci. 2015;13:Doc14. https://doi.org/10.3205/000218.
van den Boom L, Kostev K. Persistence with insulin pump therapy among children and young adults with type 1 diabetes in Germany: an update. Diabetes Obes Metab. 2022;24:948–50. https://doi.org/10.1111/dom.14647.
Eisen C, Lulic Z, Palacios-Moreno JM, et al. Persistence and adherence to dutasteride/tamsulosin fixed-dose versus free-combination alpha blocker/5ARI therapy in patients with benign prostate hyperplasia in Germany. Int J Clin Pharmacol Ther. 2020;58:37–49. https://doi.org/10.5414/CP203549.
Siddiqi OK, Ruberg FL. Cardiac amyloidosis: an update on pathophysiology, diagnosis, and treatment. Trends Cardiovasc Med. 2018;28:10–21. https://doi.org/10.1016/j.tcm.2017.07.004.
Roy A, Peterson A, Marchant N, et al. Baseline characteristics and secondary medication adherence patterns among patients receiving tafamidis prescriptions: a retrospective analysis using a national specialty pharmacy dispensing database. Patient Prefer Adherence. 2022;16:1115–29. https://doi.org/10.2147/ppa.S352332.
Damy T, Bourel G, Slama M, et al. Epidemiology of transthyretin amyloid cardiomyopathy (ATTR-CM) in France: EPACT, a study based on the French nationwide claims database SNDS. Value Health. 2020;23:S498–9.
Naderi SH, Bestwick JP, Wald DS. Adherence to drugs that prevent cardiovascular disease: meta-analysis on 376,162 patients. Am J Med. 2012;125(882–887): e881. https://doi.org/10.1016/j.amjmed.2011.12.013.
Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: its importance in cardiovascular outcomes. Circulation. 2009;119:3028–35. https://doi.org/10.1161/CIRCULATIONAHA.108.768986.
Kostev K, Yakkali B, Chaudhari S, et al. Persistence with first-line antihypertensive therapy in Germany: a retrospective cohort study with 2,801,469 patients. Int J Clin Pharmacol Ther. 2023. https://doi.org/10.5414/CP204358.
European Medicines Agency. Annex I summary of product characteristics Vyndaqel (tafamidis). https://www.ema.europa.eu/en/documents/product-information/vyndaqel-epar-product-information_en.pdf. Accessed Nov 1, 2023.
Garcia-Pavia P, Rapezzi C, Adler Y, et al. Diagnosis and treatment of cardiac amyloidosis. A position statement of the European Society of Cardiology Working Group on Myocardial and Pericardial Diseases. Eur J Heart Fail. 2021;23:512–26. https://doi.org/10.1002/ejhf.2140.
Witteles R. Cardiac amyloidosis. 2016 (last update: July 7, 2016). https://www.acc.org/latest-in-cardiology/articles/2016/07/07/14/59/cardiac-amyloidosis. Accessed Nov 1, 2023.
Pavlusova M, Miklik R, Spacek R, et al. Increased dose of diuretics correlates with severity of heart failure and renal dysfunction and does not lead to reduction of mortality and rehospitalizations due to acute decompensation of heart failure; data from AHEAD registry. Cor Vasa. 2018;60:e215–23. https://doi.org/10.1016/j.crvasa.2017.09.007.
Rozenbaum MH, Large S, Bhambri R, et al. Impact of delayed diagnosis and misdiagnosis for patients with transthyretin amyloid cardiomyopathy (ATTR-CM): a targeted literature review. Cardiol Ther. 2021;10:141–59. https://doi.org/10.1007/s40119-021-00219-5.
Kemner J, Attal S, Rozenbaum M, et al. Abstract 10136: Tafamidis patient characteristics and adherence: a retrospective analysis of German statutory health insurance data. Circulation. 2022;146:10136. https://doi.org/10.1161/circ.146.suppl_1.10136.
Acknowledgements
The authors thank everyone who has contributed to this study.
Medical Writing/Editorial Assistance
Manuscript formatting support was provided by April Cabang and Jennifer Bodkin of Engage Scientific Solutions and was funded by Pfizer; no contribution was made to editorial content.
Funding
This study was supported by Pfizer Inc, New York, NY, USA. The journal’s Rapid Service Fee was supported by Pfizer Inc.
Author information
Authors and Affiliations
Contributions
Sepideh Attal, Jason Kemner and Jose Alvir were responsible in the conceptualization, supervision, and review. Sebastian Barth supported the statistical analysis plan. Sofia Schuessler supported the analysis, writing-review and editing.
Corresponding author
Ethics declarations
Conflict of Interest
Sepideh Attal, Jason Kemner, Jose Alvir, are employees of Pfizer and own stock and/or stock options. Sebastian Barth is an employee of IQVIA Commercial GmbH & Co. OHG, which received funding from Pfizer to assist in the conduct of this study and for manuscript development. Sofia Schuessler worked at IQVIA GmbH & Co. OHG at the time of the study and was a paid consultant to Pfizer in connection with this study.
Ethical Approval
The database used for this study includes only anonymized data in compliance with the provisions set forth in the applicable data protection laws. German law allows the use of anonymous electronic medical records for research purposes under certain conditions. In accordance with this legislation, it is not necessary to obtain informed consent from patients or approval from a medical ethics committee for this type of observational study that contains no directly identifiable data. Since all patients were only queried as aggregates and no protected health information was available for queries, no institutional review board approval was required for the use of this database or the completion of this study. IQVIA was contracted by Pfizer in connection with this study. Pfizer did not have permission to access the IQVIATM LRx database at any time during the study, but rather received aggregated results from the database.
Additional information
Prior Presentation: The contents of this manuscript were presented at the American Heart Association Scientific Sessions 2022, November 5–7, 2022 at McCormick Place Convention Center in Chicago, IL, USA. The conference abstract was published in Circulation [24].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Attal, S., Kemner, J., Alvir, J. et al. Tafamidis 61 mg Patient Characteristics and Persistency? A Retrospective Analysis of German Statutory Health Insurance Data (IQVIA™ LRx). Cardiol Ther 13, 369–378 (2024). https://doi.org/10.1007/s40119-024-00365-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-024-00365-6