Abstract
Introduction
Although ablation of typical atrial flutter (AFL) can be easily achieved with radiofrequency energy (RF), no studies compare the effectiveness of different ablation catheters. Our study aimed to compare the efficacy of various types of ablation catheters in treating typical AFL.
Methods
We analyzed patients with AFL who underwent RF ablation by a single operator at our institution. Successful ablation was evidenced by a bidirectional conduction block (trans-isthmus conduction time ≥ 130 ms or double potentials ≥ 90 ms). Logistic regression was used to compare success rate and linear regression to compare lesion time.
Results
Out of 222 patients, only six did not meet the success criteria (2.7%). The catheters used were non-irrigated, large-tip, internally irrigated (Chili II Boston Scientific), and externally irrigated (non-force-sensing) catheters (Cool Path, Abbott). An externally irrigated force-sensing catheter (TactiCath, Abbott) was used with > 10 gm of force and (LPLD) setting (30 W− 45 °C− 60 s), and high-power short-duration (HPSD) setting (50 W− 43 °C − 12 s). No complications were encountered. The catheter type had no statistically significant association with ablation success. With the use of externally irrigated catheter with contract force-sensing and HPSD settings, statistically significantly shortening of lesion time was achieved 758.3 s, [CI − 1128.29, − 388.35 s] followed by LPLD by 419.0 s [CI − 808.49, − 29.47 s].
Conclusions
The typical atrial flutter radiofrequency ablation procedure had a high success rate, which was not influenced by the type of ablation catheter. Contact force ablation catheter and HPSD are associated with shorter total lesion time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
No studies directly compare different ablation catheters for ablation of typical atrial flutter. |
We are comparing the effectiveness of four different ablation catheters to assess success rates and procedural time. |
What was learned from the study? |
We found no difference in the effectiveness of achievement of successful lesion set. High-power short-duration strategy shortens the ablation time. |
Based on the current set of data, evolving catheter technology has not resulted in substantial improvement in outcomes of typical atrial flutter ablation. |
Introduction
Atrial flutter (AFL) is a common arrhythmia frequently and very effectively treated with catheter ablation. The overall incidence of AFL is approximately 88 per 100,000 person-years and increases with age [1]. Catheter ablation is a first-line treatment method. A meta-analysis of 21 studies examining atrial flutter success rate suggested a single procedure success of 92% and multiple procedure success rates of 97% [2]. Radiofrequency energy is commonly used, but cryoablation has also been employed [3]. The quest to develop better, safer, and faster ablation of atrial fibrillation techniques has resulted in new catheter development applicable to atrial flutter ablation. Although some randomized clinical trials have been published to assess the effectiveness of different large-tip catheters vs. irrigated catheters, they provided conflicting results [4, 5]. Furthermore, there are no comparative studies on force-sensing catheters and various ablation settings [5]. Therefore, we undertook a retrospective analysis of consecutive patients undergoing AFL ablation using different ablation catheters to assess the effectiveness of these catheters and different ablation settings in treating the AFL.
Methods
Settings and Population
We included patients undergoing typical atrial flutter ablation as a standalone procedure in our institution from July 2007 to December 2021. Patients with missing data and demographic information were excluded. All procedures were done by a single operator using fluoroscopy and 3D mapping (using a different generations of the Ensite mapping system from Abbott, Minneapolis, MN, USA). Previously published criteria of ablation success were used [6]. Briefly, achievement of bidirectional isthmus conduction time ≥ 130 ms and the presence of double potentials at least 90 ms apart were considered an acute success. Lesion time was the total time of lesion creation.
Analysis
Baseline demographic data, including ethnicity, age, gender, past medical history, and medications use, were collected.
We classified the ablation catheters into the following categories: non-irrigated 8 and 10 mm, (Blazer II Boston Scientific, Marlborough, MA, USA), internally irrigated 4 mm (Chili II, Boston Scientific, Marlborough, MA, USA), externally irrigated 4 mm (Cool Path, Abbott, Minneapolis, MN, USA), and externally irrigated force-sensing 3.5 mm (TactiCath, Abbott, Minneapolis, MN, USA). For non-irrigated catheters, power was set to 70–100 W and maximum temperature of 60 °C, and typically a 60-s application; for internally irrigated catheters, settings were power of 30 W and temperature of 43 °C; externally irrigated catheter for low-power long-duration (LPLD) settings were power of 30 W and temperature of 45 °C or for high-power short-duration (HPSD), power of 50 W and temperature of 43 °C, and 12 s in duration. With force-sensing catheters, lesions were applied with force ranging from 10–20 g. The RF application was made point-by-point in a contiguous fashion. The gaps in the ablation line were most often identified during coronary sinus pacing and ablation catheter mapping. In some cases, the gaps were identified with high-density activation mapping.
Statistical Analysis
Our study compared different catheters in terms of success rate and lesion time. We used logistic regression to compare the success rate between other catheters and linear logistic regression to compare lesion time. The non-irrigated large-tip catheter was the reference point. All statistical analyses were performed using statistical software R version 3.5.0 (R Foundation for Statistical Computing, Vienna, Austria). The study has received a waiver of consent from the Institutional Review Board of SUNY Downstate Health Sciences University study 1650721-1. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Results
We identified a total of 222 patients during the study period. The mean age of the population was 72 (± 14) years old, and 50% were females. Patient characteristics are summarized in Table 1.
Figure 1 shows the breakdown of the catheter used. The most common catheters used were contact force catheters with the two settings (HPSD and LPLD).
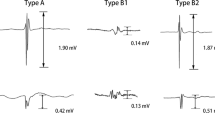
Were we unable to achieve a bidirectional block in only six patients (2.7%), despite employing multiple catheter/sheath configurations. For patients with sinus rhythm, the mean pre-ablation clockwise and counterclockwise times were 55.32 s and 55.67 s, respectively. Conduction time increased after ablation to an average clockwise conduction time of 146.8 s and a counterclockwise time of 147.9 s.
The type of catheter used did not affect the success rate (p value > 0.9). We could not identify factors associated with ablation failure due to the low incidence of unsuccessful cases. Lesion time for non-irrigated catheters was 1162.8 s. Compared with the non-irrigated catheter, the contact force catheter was significantly associated with a shorter lesion time by 629.92 s (− 993.59, − 266.25). When the different settings of contact force catheters were compared with the different types of catheters, the HPSD had the shortest lesion time, followed by the LPLD (Table 2).
Discussion
Our study indicates that HPSD lesions applied with force-sensing catheters achieve the bidirectional CTI block in the shortest time. Our data also show that externally irrigated catheters with force sensing can accomplish a set of effective lesions faster than non-irrigated and internally irrigated catheters.
Our data suggest similar acute effectiveness of all catheters in achieving CTI block. Past studies comparing the efficacy of gold, platinum-iridium, and externally irrigated-tip catheters showed mixed results, with either equivalency of effectiveness and an advantage with gold-tip catheters and irrigated catheters, in the acute success of the procedure [7, 8]. Furthermore, the reported rate of failure to achieve CTI block of 5% with gold and platinum-iridium-tip catheters was similar to our data. The success of 8-mm and 10-mm-sized catheter tips has been demonstrated in multiple trials over the past 10 years. A study performed by Ventura et al. confirmed this by showing successful ablation using 8-mm catheter tips in patients resistant to ablation using 4-mm catheter tips [8]. Shorter procedure times are reported with the larger-tip ablation catheters than standard 4- or 5-mm-tip ablation catheters, with comparable or greater efficacy, no significant increase in complications, and improved quality of life. Larger-tip ablation electrodes do require the use of higher-power radiofrequency generators up to 100 W. A study comparing the efficacy of 8- and 10-mm ablation catheters and high energy (100 W) showed that the actual number of ablations required (i.e., 10 vs. 14) as well as total lesion time was less for the 10-mm-tip catheter, however with almost 7% failure to achieve CTI block [9]. However, it is not unusual to experience difficulty in delivering full power during those ablations due to inadequate catheter cooling, particularly in areas of CTI indentations where blood flow is restricted.
Irrigated-tip catheter technology was designed to cool the electrode tip, prevent excessive temperatures at the electrode tip–tissue interface, and thus allow continued delivery of RF current into the surrounding tissue. This ablation system creates larger and deeper ablation lesions and minimizes steam pops and thrombus formation. Compared to small-tip catheters, irrigated-tip ablation catheters require fewer lesions to achieve CTI block and shorten the procedure [10].
Irrigated catheters can be divided into open and closed types of irrigation. In open irrigation, there are holes in the tip of the catheter through which (typically) normal saline is pumped. Closed-irrigation catheters have a system within the tip that allows 5% glucose solution to pass through the interior and then be removed. Yokoyama et al. compared a closed-irrigation catheter (Chilli®, Boston Scientific, Natick, MA, USA) versus an open-irrigation catheter (ThermoCool) for RF lesion morphology and depth, thrombus formation, and occurrence of steam pops in a dog model [11]. It was found that the resultant ablation lesion was similar to closed- and open-irrigated electrodes yet more thrombus formation on the electrode with closed irrigation [12]. Our data confirm the equivalent performance of closed- and open-irrigated catheters in AFL ablation.
HPSD was designed to limit resistive heating and therefore produces less collateral tissue damage while achieving similar success [13,14,15,16]. In a single non-randomized study, HPSD ablation resulted in a shortened ablation time, as seen in our study [17, 18]. We have not seen a reduction in the number of lesions needed to achieve CTI block, as typically, HPSD ablation creates similar size lesions to traditional irrigated catheter ablation [13].
We could not identify factors associated with ablation failure due to the low incidence of inability to achieve CTI block. Typical predictors of failed ablation are previous atrial fibrillation and presence of complex congenital heart disease (transposition of great arteries, systemic ventricle dilation) [18]. Previous data suggest that HPSD helps achieve CTI block in all patients [17, 19].
The observational nature of the design limits our study. Nevertheless, the presence of a single operator performing the procedure eliminates some of the bias that might be present with multiple operators, even in a randomized study. We do not believe that operator’s experience has influenced the outcomes, as we do not see differences between non-irrigated catheters and internally and externally irrigated catheters (as the latter were available more recently). Having the ability to objectively assess the force exerted by the catheter during ablation is certainly advantageous as evident in our data set. Beyond this feature of the mapping software, we do not believe that different versions of the mapping system have significantly affected outcomes in this study.
Conclusions
Our data strongly suggest that the HPSH technique coupled with a force-sensing catheter is the most efficacious modality for AFL circuit ablation. Furthermore, disappointingly, technological advances in ablation catheters design do not seem to be translating to improved efficacy of the ablation procedures.
Data Availability
Data linked to this study can be found at https://doi.org/10.5061/dryad.ghx3ffbs2.
References
Sok-Sithikun B, Decebal GL, Francis M, Nadir S. Atrial flutter: more than just one of a kind. Eur Heart J. 2015;36(35):2356–63.
Kacprzyk M, Kuniewicz M, Lelakowski J. Trzepotanie przedsionków w praktyce kardiologa [Atrial flutter in cardiology practice]. Pol Merkur Lekarski. 2020;48(285):204–8.
Daubert JP, Budzikowski AS, Feld G. Cryoablation of cavotricuspid valve isthmus-dependent atrial flutter. In: Khairy P, Dubuc M, editors. Cryoablation for cardiac arrhythmias. Vision Communications; 2008. p. 61–81.
Kardos A, Foldesi C, Mihalcz A, Szili-Torok T. Cavotricuspid isthmus ablation with large-tip gold alloy versus platinum-iridium-tip electrode catheters. Pacing Clin Electrophysiol. 2009;32(Suppl 1):S138–40. https://doi.org/10.1111/j.1540-8159.2008.02270.x.
Scavée C, Jaïs P, Hsu LF, Sanders P, Hocini M, Weerasooriya R, Macle L, Raybaud F, Clementy J, Haïssaguerre M. Prospective randomized comparison of irrigated-tip and large-tip catheter ablation of cavotricuspid isthmus-dependent atrial flutter. Eur Heart J. 2004;25(11):963–9. https://doi.org/10.1016/j.ehj.2004.03.017.
Tada H, Oral H, Sticherling C, et al. Double potentials along the ablation line as a guide to radiofrequency ablation of typical atrial flutter. J Am Coll Cardiol. 2001;38(3):750–5. https://doi.org/10.1016/S0735-1097(01)01425-5.
Sacher F, O’Neill MD, Jais P, Huffer LL, Laborderie J, Derval N, Deplagne A, Takahashi Y, Jonnson A, Hocini M, Clementy J, Haissaguerre M. Prospective randomized comparison of 8-mm gold-tip, externally irrigated-tip and 8-mm platinum-iridium tip catheters for cavotricuspid isthmus ablation. J Cardiovasc Electrophysiol. 2007;18(7):709–13. https://doi.org/10.1111/j.1540-8167.2007.00861.x.
Ventura R, Willems S, Weiss C, Flecke J, Risius T, Rostock T, Hoffmann M, Meinertz T. Large tip electrodes for successful elimination of atrial flutter resistant to conventional catheter ablation. J Interv Card Electrophysiol. 2003;8(2):149–54. https://doi.org/10.1023/a:1023665002255.
Feld GK. Radiofrequency ablation of atrial flutter using large-tip electrode catheters. J Cardiovasc Electrophysiol. 2004;15(10 Suppl):S18-23. https://doi.org/10.1046/j.1540-8167.2004.15104.x.
Jaïs P, et al. Mapping and ablation of left atrial flutters. Circulation. 2000. https://doi.org/10.1161/01.CIR.101.25.2928.
Yokoyama K, Nakagawa H, Wittkampf FHM, Pitha JV, Lazzara R, Jackman WM. Comparison of electrode cooling between internal and open irrigation in radiofrequency ablation lesion depth and incidence of thrombus and steam pop. Circulation. 2006;113(1):11–9. https://doi.org/10.1161/circulationaha.105.540062.
Houmsse M, Daoud EG. Biophysics and clinical utility of irrigated-tip radiofrequency catheter ablation. Expert Rev Med Devices. 2012;9(1):59–70. https://doi.org/10.1586/erd.11.42.
Winkle RA, Mohanty S, Patrawala RA, et al. Low complication rates using high power (45–50 W) for short duration for atrial fibrillation ablations. Heart Rhythm. 2019;16:165–9.
Bourier F, Duchateau J, Vlachos K, et al. High-power short-duration versus standard radiofrequency ablation: Insights on lesion metrics. J Cardiovasc Electrophysiol. 2018;29:1570–5.
Bhaskaran A, Chik W, Pouliopoulos J, et al. Five seconds of 50–60 W radio frequency atrial ablations were transmural and safe: an in vitro mechanistic assessment and force-controlled in vivo validation. Europace. 2017;19:874–80.
Leshem E, Zilberman I, Tschabrunn CM, et al. High-power and short-duration ablation for pulmonary vein isolation: biophysical characterization. JACC Clin Electrophysiol. 2018;4:467–547.
Heart Rhythm O2 Volume 1, Issue 5, December 2020, Pages 317–323
Roca-Luque I, Rivas-Gándara N, Dos-Subirà L, Francisco-Pascual J, Pijuan-Domenech A, Pérez-Rodon J, Santos-Ortega A, Roses-Noguer F, Ferreira-Gonzalez I, García-Dorado García D, Moya MA. Predictors of acute failure ablation of intra-atrial re-entrant tachycardia in patients with congenital heart disease: cardiac disease, atypical flutter, and previous atrial fibrillation. J Am Heart Assoc. 2018;7(7): e008063. https://doi.org/10.1161/JAHA.117.008063.PMID:29602766;PMCID:PMC5907589.
Golian M, Ramirez FD, Alqarawi W, Hansom SP, Nery PB, Redpath CJ, Nair GM, Shaw GC, Davis DR, Birnie DH, Sadek MM. High-power short-duration radiofrequency ablation of typical atrial flutter. Heart Rhythm O2. 2020;1(5):317–23. https://doi.org/10.1016/j.hroo.2020.09.002.
Funding
No funding or sponsorship was received for this study or publication of this article. The Rapid Service Fee was funded by the authors.
Author information
Authors and Affiliations
Contributions
Study design was completed by Adam S. Budzikowski. Data collection was completed by Asher Gorantla, Mahmoud Alsaiqali, Johnathan Francois, and Shruthi Sivakumar. Data analysis was completed by Mahmoud Alsaiqali, Leonall Freytes-Santiago, Ahmad Jallad, and Adam S. Budzikowski. Manuscript writing was completed by Adam S. Budzikowski, Asher Gorantla, and Mahmoud Alsaiqali.
Corresponding author
Ethics declarations
Conflict of Interest
Asher Gorantla, Mahmoud Alsaiqali, Johnathan Francois, Shruthi Sivakumar, Leonell Freytes-Santiago, Ahmad Jallad, and Adam S. Budzikowski have nothing to disclose.
Ethical Approval
The study has received a waiver of consent from the Institutional Review Board of SUNY Downstate Health Sciences University study 1650721-1. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Gorantla, A., Alsaiqali, M., Francois, J. et al. Comparative Effectiveness of Various Radiofrequency Ablation Catheters in the Ablation of Typical Atrial Flutter. Cardiol Ther 12, 741–747 (2023). https://doi.org/10.1007/s40119-023-00336-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-023-00336-3