Abstract
There is growing interest in invasive hemodynamic assessment in cardiogenic shock, primarily due to the widespread adoption of mechanical circulatory support (MCS). Invasive hemodynamic assessment is central to two aspects of cardiogenic shock management: (1) the phenotyping of cardiogenic shock, and (2) the assessment of response to therapy. Phenotyping of cardiogenic shock serves to guide timely therapeutic intervention, and the assessment of hemodynamic response to therapy directs the escalation or de-escalation of therapy, including MCS. This review aims to discuss these two aspects of hemodynamic assessment in cardiogenic shock. Firstly, the physiologic underpinnings of a phenotyping schema, and the implication of the cardiogenic shock phenotype on the MCS strategy in cardiogenic shock will be discussed. Secondly, the concept of cardiac power output and ‘effective’ oxygen delivery will be discussed in relation to hemodynamic response to therapy in cardiogenic shock.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cardiogenic shock is characterized by (i) organ dysfunction related to hypoperfusion; (ii) as a result of circulatory failure primarily due to inadequate cardiac output; (iii) that can be attributed predominantly to an underlying cardiac dysfunction. |
A phenotyping scheme that includes the acuity/severity of cardiogenic shock and characterization of the right and left heart systems can guide therapeutic interventions; and inform prognosis. |
Assessment of the right and left heart systems should include pulmonary and systemic vascular ‘function’. Distributive shock or vasoplegia often complicates cardiogenic shock. |
‘Effective oxygen delivery’ can be used to assess response to therapeutic interventions in cardiogenic shock. |
Introduction
Invasive hemodynamic assessment is enjoying a renaissance in cardiogenic shock (CS), spurred by the growth in critical care cardiology, widespread adoption of temporary mechanical circulatory support (MCS), and recent studies suggesting improved outcomes associated with comprehensive hemodynamic profiling in CS [1]. Many have advocated the use of invasive hemodynamic assessment to characterize the CS phenotype to guide therapy, especially MCS [2]. Therefore, a review of hemodynamic assessment in CS is timely. This review aims to discuss the practical use of hemodynamic assessment, underpinned by physiologic considerations, to phenotype CS to guide the deployment of MCS, and assess the response to therapy in CS. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Defining Cardiogenic Shock
Conceptually, CS is characterized by tissue/organ dysfunction related to inadequate oxygen delivery due to circulatory failure that is primarily (although not solely) related to underlying cardiac dysfunction. Thus, the diagnosis of CS requires evidence of (i) organ dysfunction related to hypoperfusion; (ii) circulatory failure related to inadequate cardiac output; (iii) that can be attributed predominantly to an underlying cardiac dysfunction. The precise clinical and hemodynamic criteria used to define CS have varied between studies (reviewed previously) [3].
Historically, the natural history of CS has been divided into four stages. At the ‘initial’ stage, the reduction in cardiac output may be tolerated with minimal symptoms or hemodynamic compromise. The persistent reduction in cardiac output and oxygen delivery (and frequently hypotension) triggers compensatory mechanisms during the ‘compensatory’ stage, including sympathetic and neurohormonal activation with resultant vasoconstriction and tachycardia. The failure of these compensatory mechanisms to restore blood pressure and oxygen delivery would lead to deteriorating organ function and metabolic derangements in the ‘progressive’ stage. Eventually, without effective intervention, CS becomes ‘refractory’, often accompanied by vascular dysfunction and development of multi-organ dysfunction syndrome.
In practice, the presentation of CS is variable depending on the underlying pathology and often takes a non-linear trajectory, from gradual insidious decline to multi-organ dysfunction and catastrophic circulatory arrest. Early ‘rescue’ with inotropes and MCS may prevent the evolution of CS from a deficiency of convective oxygen delivery to cellular dysoxia and multi-organ failure that characterize ‘refractory’ CS [4].
Hemodynamic Phenotyping of Cardiogenic Shock
Phenotyping of CS has two objectives: (i) to guide timely therapeutic interventions; and (ii) the inform prognosis. Forrester et al. [5] first developed a clinical classification scheme for the assessment of patients with acute myocardial infarction, which has since been translated into the advanced HF population [6]. This simple schema has been widely adopted into practice, but is inadequate for directing management of CS, especially the use of MCS. More recently, Zweck et al. [7] used machine learning to describe three CS phenotypes, but this schema similarly has limited utility in guiding treatment.
To meet the two objectives, the CS phenotyping schema should consider the clinical presentation (acuity and severity) and underlying pathophysiology:
-
1.
There are two widely adopted clinical classification systems to describe the acuity and severity of CS. First, the Interagency Registry for Mechanically Assisted Circulatory Support devices (INTERMACS) profile, ranging from 1 to 7 is commonly used in advanced heart failure. INTERMACS profiles 3, 2 and 1 describe stable CS on inotropes, deteriorating CS despite inotropes and critical “crash and burn” CS. INTERMACS profiles 4–7 refer to advanced heart failure without CS. Second, the more recent Society for Cardiovascular Angiography and Interventions (SCAI) classification system was developed to describe the acuity/severity of CS to guide the urgency of intervention. The SCAI classification is associated with short term clinical outcomes in patients with CS [8]. Criteria for the SCAI stages have been described recently [9] (Table 1). Conceptually, SCAI profiles C, D, and E correspond to INTERMACS 3, 2, and 1, respectively.
-
2.
The phenotype should be aligned with the therapeutic strategy, which necessitates an appreciation for the underlying pathophysiology. Understanding the etiology would assist in the pathophysiologic assessment; but this is often unknown at the point of presentation. In practice, clinicians supplement their clinical assessment with imaging and hemodynamic data to characterize the pathophysiology in CS based on the (i) presence respiratory failure; (ii) function of the left heart system; and (iii) the right heart system. Respiratory physiology will not be discussed for the purpose of this review.
Phenotyping the Left Heart System
The left heart system consists of the venous sub-system (pulmonary venous and left atrial pathology), the left ventricle (LV) and the systemic arteries. Left ventricular ejection fraction (LVEF) is commonly used to assess LV function, but characterization of LVEF as a measure of LV function is misleading. The physiology of LVEF is well illustrated by the use of pressure–volume loop, which are subtended by the relatively linear LV end-systolic elastance (Ees) and arterial elastance (Ea) and the non-linear end-diastolic pressure–volume relationship (EDPVR) (Fig. 1).
Pressure–volume analysis of the left heart. A normal LV loop in shown A. An upward shift in the end-diastolic pressure–volume relation (EDPVR, orange block arrow) increases LVEDP (or PAWP) at the same LVEDV, which may limit recruitable preload (B). The drops in LVEF and stroke volume in B are due to reduction in contractility (Ees). The LVEDP increases at higher LV volume due to the non-linear EDPVR (C, D). At the same LVEF, stroke volumes are higher in C, D compared to B. The maintenance of LVEF and stroke volume in C despite lower contractility (Ees) is related to the lower Ea. Superadded vasoplegia (lower Ea) in the face of low Ees in D maintains stroke volume at the cost of lower ESP (and perfusion pressure) and results in a low ‘gain’ system. In the low ‘gain’ system (D), increase in Ea (e.g., by vasopressor therapy) has a more modest effect on blood pressure due to the lower Ees slope, potentially at greater cost to stroke volume. Simultaneous increase in Ees and Ea are required to increase blood pressure without compromising stroke volume
End-systolic elastance (Ees) describes the slope of the end-systolic pressure–volume relationship and is generally accepted as a relatively load-independent measure of LV contractility, if myocardial properties (mass, geometry, and myocyte-matrix composition) are unchanged. Mathematically, Ees can be expressed as:
where V0 is the maximum ventricular volume at zero pressure, and ESP is end-systolic pressure. The V0 is negligible in normal subjects, but increases significantly with progressive LV remodeling.
Arterial elastance is a lumped parameter that combines steady and pulsatile loading [10]. Mathematically, Ea is the negative slope of the line joining the EDV and ESP (Ea = ESP/stroke volume) [11], sharing the same unit of measurement as Ees. Ventriculo-arterial coupling can thus be expressed mathematically as the dimensionless Ea/Ees ratio, which is a determinant of myocardial oxygen demand and the efficiency of ventricular contraction [12]. In practice, Ea can be derived by measuring stroke volume and estimating ESP from systolic blood pressure [13] (i.e., Ea = (0.9 × systolic blood pressure)/stroke volume).
The EDPVR is a determinant of filling pressure (end-diastolic pressure (EDP) or pulmonary artery wedge pressure (PAWP)). As EDPVR is non-linear, filling pressure increases disproportionately as higher LV end-diastolic volume (LVEDV). Increase in chamber ‘stiffness’ increases the slope of the EDPVR, resulting in greater increase in EDP per unit change in EDV.
Rearranging the equation,
Dividing by EDV,
It is evident that LVEF is a function of LV contractility (Ees), the arterial pressure (ESP), preload (EDV) and LV remodeling (V0); thus reflects the function of the left heart system. Ross described the concept of afterload mismatch [14], i.e., the reduction in stroke volume when afterload is increased in the presence of limited preload reserve (limited venous return or when maximal diastolic fiber length is reached), at any given level of inotropy. Expressed mathematically, at a fixed EDV (limited preload reserve), an increase in ESP/Ees ratio would increase (ESV − V0) and reduce stroke volume. In this regard, LVEF must be interpreted in this wider context of the left heart system.
-
1.
At the same blood pressure and LVEF, patients with smaller LVEDV must by definition have lower stroke volumes; and stroke volume may be higher in patients with higher LVEDV despite a lower LVEF.
-
2.
Impaired contractility is sine quo non of CS. Indeed, in ‘classic’ CS with low systolic blood pressure, low LVEF coupled with normal/high LVEDV must indicate severely impaired LV contractility (low Ees). In non-hypotensive CS (normal ESP) with low Ees, (ESV − V0) must be increased, as Ees = ESP/(ESV − V0). Higher (ESV − V0) at a given EDV would generally indicate lower stroke volume as reduction in V0 is unusual.
-
3.
Low Ea (vasodilatation) in the setting of low Ees would maintain/improve ventriculo-arterial coupling (Ea/Ees ratio) and myocardial efficiency, at the expense of the ‘gain’ in the left heart system (Fig. 1). The consequences of a ‘low gain’ system (low Ea and Ees) are: (a) expansion of central blood volume (increase LVEDV) have only modest effect on systolic blood pressure; (b) a given increase in Ea (e.g., with vasoconstriction) in the setting of low Ees produces smaller increase in systolic blood pressure. A simultaneous increase in Ees and Ea is required to increase the ‘gain’ of the system. Thus, superadded distributive shock or vasoplegia (low Ea) in CS creates a low ‘gain’ system that limits blood pressure response to vasopressors.
Systemic vascular resistance is frequently used to describe vascular tone. Indeed, SVR is the major contributor to Ea, in addition to arterial compliance and heart rate [13]. In the absence of invasive hemodynamic assessment, vascular tone could be inferred from the diastolic blood pressure. During diastole, the exponential decay in arterial blood pressure is characterized by a time constant that is the product of arterial compliance and resistance. Low arterial resistance and compliance shorten the time constant (i.e., more rapid drop in blood pressure), with consequent reduction in diastolic blood pressure [15]. However, diastolic blood pressure is also a function of heart rate (higher diastolic blood pressure at higher heart rate). This is the basis for the diastolic shock index (DSI), which is the ratio of heart rate to diastolic blood pressure (DSI = heart rate/ diastolic blood pressure). In septic shock, high DSI of over > 2.0 has been shown to be associated with increase mortality [16]. The DSI may have utility in early identification of superadded distributive shock, but it has not been studied in CS.
The assessment of systemic vascular resistance and DSI is relevant in the setting of circulatory failure as distributive shock frequently complicates CS. Possible causes include the over-enthusiastic use of neurohormonal antagonists; an inflammatory response triggered by acute myocardial infarction [17] or cardiac arrest [18], or bacterial translocation due to bowel congestion or ischemia [19]. In a study of unselected patients in cardiac intensive care unit, over a third of the patients had two or more features of systemic inflammatory syndrome (abnormal body temperature, abnormal white cell count, elevated heart rate and hyperventilation); with greater requirements for vasopressors and higher mortality [20]. Lower diastolic blood pressure, systemic vascular resistance and high DSI, especially in association with features of systemic inflammatory syndrome should alert clinicians to this syndrome of superadded distributive shock and potential need for earlier support. Indeed, in a single-center study of patients with CS, low diastolic blood pressure was independently associated with 28-day mortality [21].
-
4.
Elevated LVEDP or PAWP in the presence of a small or normal LV chamber volume would indicate an abnormally raised LV EDPVR (Fig. 1). The LV EDPVR is primarily related to intrinsic myocardial and matrix properties (an underlying diastolic or restrictive abnormality); but diastolic ventricular interaction and pericardial constraint (e.g., RV overload) also produces a leftward/upward shift in the EDPVR. The steeper LV EDPVR limits recruitable preload as even a small recruitment of LVEDV would be accompanied a prohibitive increase in LVEDP or PAWP. The clinical relevance of this observation is twofold. Firstly, volume expansion with fluid administration would be inadvisable in patients with elevated filling pressure and small/ normal LV chamber volumes. Secondly, increase in afterload (Ea) in the absence of recruitable preload must reduce stroke volume in the absence of corresponding increase in contractility (Ees). This is analogous to observation (2)—at the limit of LVEDV, increase in Ea without corresponding increase in Ees would increase (ESV-V0). Despite its clinical relevance, LVEDVs are rarely reported in clinical studies.
In summary:
-
(i)
LVEF must be interpreted with LV chamber volume, LVEDP, or PAWP and systolic and diastolic blood pressures to characterize the left heart phenotype.
-
(ii)
Diastolic/restrictive dysfunction limits recruitable preload and cardiac output reserve in response to increased afterload.
-
(iii)
Elevated LVEDP or PAWP in the presence of a small or normal LV chamber volume indicates an abnormality in diastolic property (diastolic/restrictive dysfunction).
-
(iv)
Poor contractile function coupled with vasoplegia creates a low ‘gain’ system, characterized by modest blood pressure to volume expansion and vasoconstriction.
-
(v)
Low diastolic blood pressure, systemic vascular resistance and high diastolic shock index are indicative of concomitant vasoplegia or distributive shock.
Phenotyping the Right Heart System
The right heart system similarly consists of three sub-systems: the central venous system (central venous pressure, CVP), the right ventricle (RV) and the pulmonary circulation [22]. Right heart function is notoriously challenging to assess due to the limitations of non-invasive assessment (imaging) of the RV and the pulmonary circulation [23].
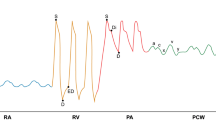
In normal individuals, the CVP is low and the RV is less than 60% the size of the LV with mid-RV diameter of ≤ 35 mm [24]. The RV dilates in response to increased loading and eventual RV–PA uncoupling manifests as a combination of CVP elevation and RV dilatation (Fig. 2). A CVP threshold for right heart failure is difficult to define. Vieillard-Baron et al. used a combination of RV dilatation on echocardiography (RV/LVEDA ≥ 0.6) and CVP ≥ 8 mmHg to define RV failure [25], but this CVP threshold is likely to be too low especially in patients with high positive driving pressure.
Pressure–volume analysis of the right heart. The normal RV loop (A) differs from the LV with a more rounded and early systolic peaking of pressure, but changes into a more rectangular shape analogous to the LV loop in the face of high afterload. The RV dilates in the face of increased afterload to maintain stroke volume (B), and the Ea/Ees and CVP may remain normal despite the increase in RV chamber volume. As the condition progresses, the RV–PA becomes uncoupled (C), which is characterized by increased Ea/Ees, CVP and RVEDP in association with RV dilatation. Features of diastolic ventricular interaction such as septal flattening become evident due to increased RVEDP, RV volume and pericardial constraint. The CVP waveform and Kussmaul physiology emerge as the RV becomes less compliant (steeper EDPVR)
Three CVP-related hemodynamic phenomena provide further evidence of RV–PA uncoupling and right heart failure. First, the elevation of CVP relative to pulmonary artery wedge pressure (PAWP) is indicative of ventricular inter-dependence (typically accompanied by increased RV: LV dimensions and abnormal septal motion) that limit cardiac output reserve [26]. The higher the CVP: PAWP ratio, the poorer the survival in heart failure (CVP: PAWP ratio ≥ 0.62 to ≥ 0.75) [27, 28]. Second, an alteration in CVP waveform to a ‘W-shaped’ morphology is indicative of poor RV compliance (steep EDPVR). The peaks of the ‘W’ are formed by prominent ‘a’ and ‘v’ waves with steep ‘x’ and ‘y’ descents. Where RV pressure is monitored, this ‘W-shaped’ CVP waveform is accompanied by the ‘square-root’ appearance during RV diastole. A more blunted ‘M-shaped’ waveform is sometimes observed in RV infarction related to proximal right coronary occlusion. ‘Ventricularization’ of the CVP waveform is indicative of severe RV dysfunction with concomitant tricuspid regurgitation.
Third, Kussmaul physiology is pathognomonic of right heart failure and associated with poor survival in patients with advanced heart failure [29]. Kussmaul physiology—the absence of a fall in CVP during spontaneous inspiration—is related to increase intra-abdominal pressure produced by diaphragmatic descent, driving venous return in the setting of hypervolemia [30] and reduced compliance of the RV (including pericardial constraint) and the pulmonary vasculature [31].
The relevance of the RV–PA interaction is exemplified by the difference between patients with primary RV disease (e.g., RV infarction) and patients with end-stage pulmonary vascular disease (including combined pre- and post-capillary pulmonary hypertension, cpcPH) [32]: (i) Unlike acute RV infarction, fluid administration is not advisable in patients with right heart failure related to pulmonary vascular disease; (ii) Pulmonary vasodilators may be indicated in the presence of pulmonary vascular disease (especially Group 1 pulmonary hypertension), but has limited role in the setting of intrinsic RV dysfunction. Indeed, routine use of inhaled nitric oxide has not been shown to be of benefit in RHF post-LVAD implantation [33]; (iii) The delivery of continuous pulmonary blood flow with the use of right ventricular assist device (RVAD) in the presence of pulmonary vascular disease may exacerbate ventilation-perfusion mismatch [34].
Pulmonary vascular resistance (PVR), derived as the ratio of transpulmonary pressure gradient to flow (cardiac output) is commonly used to describe the pulmonary circulation, but the interpretation of PVR is nuanced, especially in the presence of pulmonary venous congestion [35]. Increased blood volume in the pulmonary circulation from congestion recruits and distends vessels, with consequent reduction in (Poiseuillian) resistance at the expense of reduced vascular compliance due to the non-linear stress–strain relationship of the vascular wall. The reduction in pulmonary arterial compliance increases the (pulsatile) load on the RV, despite the reduction in Poiseuillian resistance. At reduced pulmonary arterial compliance, pulmonary artery pulse pressure (PAPP) is increased for a given stroke volume; in turn increasing the mean pulmonary artery pressure and mathematically increasing the calculated PVR, even in the absence of vasoconstriction or pulmonary vascular remodeling. This may partly explain the hyperbolic relationship between PVR and compliance, a relationship that is modified by PAWP [36]. Thus, elevation in calculated PVR is inevitable in pulmonary congestion and should not be misconstrued as pulmonary vascular disease. An increase in diastolic pressure gradient (difference between pulmonary artery diastolic pressure and PAWP) is more specific for pulmonary vascular disease. The clinical implication is that LV unloading effectively relieves RV afterload in pulmonary congestion and may obviate the need for additional RV support. In contrast, elevated PVR in conjunction with raised diastolic pressure gradient (> 5 mmHg) may be more specific for intrinsic pulmonary vascular disease, and LV unloading may be insufficient in reducing RV afterload.
Pulmonary artery pulsatility index (PAPI) is a recently described hemodynamic parameter for the assessment of right heart function. Derived as a ratio of PAPP to CVP, PAPI is sensitive to pulmonary artery compliance, and by extension the level of PAWP (reduced compliance at higher PAWP) [37]. Lower PAPI is associated right heart failure. However, due to its dependence on compliance and PAWP, the PAPI threshold would vary with the underlying pathophysiology—PAPI level higher in right heart failure due to pulmonary vascular disease compared to acute RV infarction. Thus, a single PAPI threshold cannot be applied across a range of pathophysiology.
In summary:
-
(i)
RV dilatation with raised CVP (especially with elevated CVP: PAWP ratio and altered waveform morphology and Kussmaul physiology) are indicative of RV–PA uncoupling.
-
(ii)
Pulmonary congestion reduces pulmonary arterial compliance. Reduced pulmonary arterial compliance increases calculated pulmonary vascular resistance, even if Poiseuillian resistance decreases.
-
(iii)
A single PAPI threshold cannot be defined for a range of pathophysiology, but the trend/ trajectory may be used to track the changes in the right heart system.
Phenotype to Guide MCS Strategy in Cardiogenic Shock
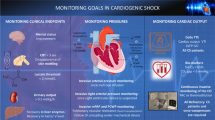
The current phenotyping based on SCAI classification and the broader respiratory-cardiac-circulatory system pathophysiology offers a more comprehensive schema to guide the use of MCS therapy. This phenotype-guided MCS strategy can be incorporated into the management of CS (Fig. 3). Veno-arterial extracorporeal membrane oxygenation is considered the first line MCS modality in patients with severe failure of the right and/or left heart systems, particularly with SCAI E presentation. The use of this schema as part of a protocolized team-based delivery of MCS in CS has been shown to improve survival [38]. Phenotyping of the respiratory-cardiac-circulatory system highlights the importance of considering the wider convective oxygen delivery (DO2) pathway instead of a cardio-centric approach, which aligns with the therapeutic priorities in CS.
Approach to CS. Early recognition of CS requires a high level of clinical suspicion to identify the three components of CS. Organ support and inotropes and/or vasopressors should be initiated early during assessment. Phenotyping follows the recognition of CS, including an assessment of the SCAI profile, right and left heart systems and respiratory failure. The CS phenotype schema informs prognosis, guides the urgency of intervention and directly shapes the MCS strategy. The choice of MCS modality is determined primarily by the phenotype. Changes in hemodynamic parameters provide early assessment of response to treatment, and facilitates almost real-time titration of therapy, including early decision on the escalation of MCS in ‘non-responders’. Lactate clearance over 8–12 h and improvement in organ function are more specific, albeit delayed indicators of response. Early hemodynamic response (e.g., cardiac power output) may predict subsequent lactate clearance. Responders enter a stabilization phase, at which point ‘Exit’ therapy could be considered
Hemodynamic Response in Cardiogenic Shock
Few would disagree that reversal of hypoperfusion is the therapeutic priority in CS. On this basis, many would advocate the use of blood lactate level as the therapeutic target. Lactate clearance is a well-established marker of response and survival in critical care [39] and CS [40]. However, two points in relation to lactate as a therapeutic target are noteworthy. Firstly, despite its undoubted clinical value, lactate clearance over 8 h [41] (or more) is by definition a relatively late measure of response. Early optimization or escalation of support could shape clinical outcomes in CS, and the 8-h ‘feedback loop’ with lactate clearance is too slow. Secondly, there is currently no specific intervention targeting blood lactate that improves outcomes in CS. Treatment that specifically targeted hyperlactatemia has not been shown to improve outcomes [42]. Thus, it is not lactate clearance per se that improves survival; rather, it is the correction of cardiopulmonary failure and consequent failure of oxygen delivery (DO2), that improves lactate clearance and by extension survival in CS.
In practice, clinicians employ hemodynamic parameters, measured in real time for rapid feedback to aid titration of therapy, with the expectation that the hemodynamic parameters would serve as surrogates for perfusion. To that end, many guidelines, position statements and reviews have recommended mean arterial pressure (MAP) of 65 mmHg as the treatment target, extrapolated from septic shock [43,44,45]. However, MAP in isolation is inadequate as a therapeutic target in CS. Firstly, hypotension without shock is often encountered in patients with advanced heart failure [46]; and CS without hypotension is a well-recognized entity [47]. The latter is especially pertinent—MAP of 65 mmHg cannot be the therapeutic target if the BP already exceeded this threshold at presentation with CS.
Secondly, it is not the MAP but the perfusion pressure that is more relevant for tissue perfusion. Perfusion pressure is defined as the difference between the inflow and outflow pressures. Inflow pressure may be lower than MAP due to arterial resistance and may differ between organs, most notably the heart (dependent on diastolic blood pressure as the inflow pressure). The critical closing pressure (Pcc, pressure at zero flow) determines the outflow pressure. In the absence of specific pathological states such as intracranial hypertension or intra-abdominal hypertension, Pcc is dependent on vasomotor tone of arterioles and precapillary sphincters, and is vascular bed-specific. Mass et al. [48] estimated a lumped Pcc of about 45 mmHg in normal healthy adults with MAP of about 85 mmHg (i.e., lumped perfusion pressure of 40 mmHg), but Pcc is likely to be much lower in the cerebral and coronary circulations, and in pathological states. However, Pcc approaches mean systemic filling pressure with the loss of vasomotor tone, which in turn is related to CVP. The CVP is also the main determinant of outflow pressure in some organs (e.g., the heart). Therefore, the CVP must be considered when setting a therapeutic target. These physiologic considerations are exemplified by the adverse effects of vasopressors in low flow states [49].
What is the therapeutic target if lactate and MAP are inadequate? As defined, CS is characterized by inadequate oxygen delivery primarily due to cardiac output limitation from underlying cardiac dysfunction. Thus, it is the failure of DO2, not hypotension that is one of the defining criteria for CS and should be considered in the assessment of therapeutic response in CS. This primacy of DO2 was recently reaffirmed by ELSO, who have highlighted DO2 three times that of oxygen consumption (VO2) as the goal of extracorporeal life support therapy [50].
where CO = cardiac output; Hb = hemoglobin; O2Sat = oxygen saturation.
Although this calculation describes the total DO2, ‘effective’ DO2 is dependent on (regional) vasomotor tone to maintain perfusion pressure, epitomized by the autoregulatory mechanisms to maintain blood flow and oxygen delivery to vital organs. As Pcc is often not known in practice, the MAP-CVP gradient is often used as a surrogate of perfusion pressure. At any given vascular tone, the heart supplies hydraulic energy to maintain the pressure within the circulation; this rate of energy output is termed cardiac power output index (CPOi) [51], calculated as:
CPOi reflects the interaction between cardiac work and vascular function, with low CPOi indicative of circulatory failure—the second defining feature of cardiogenic shock. Thus, the lack of ‘effective’ DO2 (defined by low CPOi and DO2 at less than three times the VO2) encapsulates the central pathophysiology in CS [52].
A CPOi target could be deduced based on the following:
-
(a)
Previous studies [53] have estimated VO2 in critically ill patients at about 110 ml/min/m2
-
(b)
Assume typical Hb of 100 g/l
-
(c)
To achieve target DO2:VO2 of ≥ 3.0 (i.e., DO2 ≥ 300 ml/min/m2), a minimum CI of ≥ 2.23 l/min/m2 would be required
-
(d)
For a target perfusion pressure (MAP-CVP) ≥ 60 mmHg [54, 55]
-
(e)
The minimum CPOi target for the treatment of cardiogenic shock = 60 × 2.23/451 ≈ 0.30 W/m2.
Based on this rationale, an increase in CPOi to ≥ 0.30 W/m2 could be used to define favorable response to treatment in CS. In a recent study, early (< 3 h) hemodynamic response to Impella (defined as post-Impella CPOi ≥ 0.30 W/m2) was associated with greater 12-h lactate clearance and better survival [56]. High dose norepinephrine prior to support was associated with poor hemodynamic response to Impella, emphasizing the relevance of global phenotyping of the left heart system. Based on these data, failure to achieve CPOi ≥ 0.30 W/m2 should prompt consideration for escalation of support in CS. Of note, although Hb is mathematically related to DO2, transfusion of red blood cells does not acutely increase oxygen delivery due to the altered ability of stored red blood cells to carry or deliver oxygen [57].
In summary:
-
(i)
Lactate clearance is associated with clinical outcomes, but provides too slow a ‘feedback loop’ to guide early management of CS.
-
(ii)
MAP as a therapeutic target is inadequate, as hypotension is not a pre-requisite in CS, and it is perfusion pressure and not MAP per se that is more relevant for tissue/ organ perfusion.
-
(iii)
'Effective’ oxygen delivery, taking into consideration DO2 and CPOi may be used to assess hemodynamic response to interventions in CS.
Conclusions
Circulatory failure and inadequate oxygen delivery (resulting in hypoperfusion) are defining pathophysiologic features of CS. Characterization of the respiratory-cardiac-circulatory system reflects this CS pathophysiology; coupled with the SCAI classification, offers a phenotyping schema that aids decision-making and protocolization of MCS therapy. The concept of ‘effective’ oxygen delivery and the corresponding CPOi align with the CS pathophysiology, and may be a useful hemodynamic parameter to assess response to therapy.
References
Garan AR, Kanwar M, Thayer KL, Whitehead E, Zweck E, Hernandez-Montfort J, et al. Complete hemodynamic profiling with pulmonary artery catheters in cardiogenic shock is associated with lower in-hospital mortality. J Am Coll Cardiol HF. 2020;8:903–13.
Thayer KL, Zweck E, Ayouty MA, Garan AR, Hernandez-Montfort J, Mahr C, et al. Invasive hemodynamic assessment and classification of in-hospital mortality risk among patients with cardiogenic shock. Circ Heart Fail. 2020;13: e007099.
Vahdatpour C, Collins D, Goldberg S. Cardiogenic shock. J Am Heart Assoc. 2019;8: e011991.
Lim HS. Cardiogenic shock: failure of oxygen delivery and oxygen utilization. Clin Cardiol. 2016;39:477–83.
Forrester JS, Diamond G, Chatterjee K, Swan HJC. Medical therapy of acute myocardial infarction by application of hemodynamic subsets. N Engl J Med. 1976;295:1404–13.
Nohria A, Lewis E, Stevenson LW. Medical management of advanced heart failure. JAMA. 2002;287:628–40.
Zweck E, Thayer KL, Helgestad OKL, Kanwar M, Ayouty M, Garan AR, Hernandez-Montfort J, Mahr C, Wencker D, Sinha SS, Vorovich E, Abraham J, O’Neill W, Li S, Hickey GW, Josiassen J, Hassager C, Jensen LO, Holmvang L, Schmidt H, Ravn HB, Møller JE, Burkhoff D, Kapur NK. Phenotyping cardiogenic shock. J Am Heart Assoc. 2021;10: e020085.
Naidu SS, Baran DA, Jentzer JC, Hollenberg SM, van Diepen S, Basir MB, Grines CL, Diercks DB, Hall S, Kapur NK, Kent W, Rao SV, Samsky MD, Thiele H, Truesdell AG, Henry TD. SCAI SHOCK stage classification expert consensus update: a review and incorporation of validation studies: this statement was endorsed by the American College of Cardiology (ACC), American College of Emergency Physicians (ACEP), American Heart Association (AHA), European Society of Cardiology (ESC) Association for Acute Cardiovascular Care (ACVC), International Society for Heart and Lung Transplantation (ISHLT), Society of Critical Care Medicine (SCCM), and Society of Thoracic Surgeons (STS) in December 2021. J Am Coll Cardiol. 2022;79(9):933–46.
Kapur NK, Kanwar M, Sinha SS, Thayer KL, Garan AR, Hernandez-Montfort J, Zhang Y, Li B, Baca P, Dieng F, Harwani NM, Abraham J, Hickey G, Nathan S, Wencker D, Hall S, Schwartzman A, Khalife W, Li S, Mahr C, Kim JH, Vorovich E, Whitehead EH, Blumer V, Burkhoff D. Criteria for defining stages of cardiogenic shock severity. J Am Coll Cardiol. 2022;80:185–98.
Sunagawa K, Maughan WL, Burkhoff D, et al. Left ventricular interaction with arterial load studied in isolated canine ventricle. Am J Physiol. 1983;245:H773–80.
Kelly RP, Ting C-T, Yang T-M, Liu C-P, Maughan WL, Chang M-S, Kass DA. Effective arterial elastance as index of arterial vascular load in humans. Circulation. 1992;86:513–21.
Suga H. Ventricular energetics. Physiol Rev. 1990;70:247–77.
Chemla D, Antony I, Lecarpentier Y, Nitenberg A. Contribution of systemic vascular resistance and total arterial compliance to effective arterial elastance in humans. Am J Physiol Heart Circ Physiol. 2003;285:H614–20.
Ross J Jr. Cardiac function and myocardial contractility: a perspective. J Am Coll Cardiol. 1983;1:52–62.
Lim HS. Hemodynamic assessment in cardiogenic shock. Curr Emerg Hosp Med Rep. 2019;7:214–26.
Ospina-Tascón GA, Teboul JL, Hernandez G, et al. Diastolic shock index and clinical outcomes in patients with septic shock. Ann Intensive Care. 2020;10:41.
Kohsaka S, Menon V, Lowe AM, Lange M, Dzavik V, Sleeper LA, Hochman JS, SHOCK Investigators. Systemic inflammatory response syndrome after acute myocardial infarction complicated by cardiogenic shock. Arch Intern Med. 2005;165:1643–1650.
Bro-Jeppesen J, Kjaergaard J, Wanscher M, Nielsen N, Friberg H, Bjerre M, Hassager C. Systemic inflammatory response and potential prognostic implications after out-of-hospital cardiac arrest: a substudy of the target temperature management trial. Crit Care Med. 2015;43:1223–32.
Brunkhorst FM, Clark AL, Forycki ZF, Anker AD. Pyrexia, procalcitonin, immune activation and survival in cardiogenic shock: the potential importance of bacterial translocation. Int J Cardiol. 1999;72:3–10.
Jentzer JC, Lawler PR, van Diepen S, Henry TD, Menon V, Baran DA, et al. Systemic inflammatory response syndrome is associated with increased mortality across the spectrum of shock severity in cardiac intensive care patients. Circ Cardiovasc Qual Outcomes. 2020;13: e006956.
Rigamonti F, Graf G, Merlani P, Bendjelid K. The short-term prognosis of cardiogenic shock can be determined using hemodynamic variables: a retrospective cohort study. Crit Care Med. 2013;41:2484–91.
Mehra MR, Park MH, Landzberg MJ, Lala A, Waxman AB, International Right Heart Failure Foundation Scientific Working Group. Right heart failure: toward a common language. J Heart Lung Transpl. 2014;33:123–6.
Konstam MA, Kiernan MS, Bernstein D, Bozkurt B, Jacob M, Kapur NK, et al. Evaluation and management of right-sided heart failure: a scientific statement from the American Heart Association. Circulation. 2018;137:e578-622.
Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010;23:685–713.
Vieillard-Baron A, Prigent A, Repessé X, Goudelin M, Prat G, Evrard B, Charron C, Vignon P, Geri G. Right ventricular failure in septic shock: characterization, incidence and impact on fluid responsiveness. Crit Care. 2020;24:630.
Omote K, Sorimachi H, Obokata M, Reddy YNV, Verbrugge FH, Omar M, et al. Pulmonary vascular disease in pulmonary hypertension due to left heart disease: pathophysiologic implications. Eur Heart J. 2022;00:1–15.
Grodin JL, Drazner MH, Dupont M, Mullens W, Taylor DO, Starling RC, Tang WHW. A disproportionate elevation in right ventricular filling pressure in relation to left ventricular filling pressure is associated with renal impairment and increased mortality in advanced decompensated heart failure. Am Heart J. 2015;169:806–12.
Drazner MH, Velez-Martinez M, Ayers CR, Reimold SC, Thibodeau JT, Mishkin JD et al. Relationship of right- to left-sided ventricular filling pressures in advanced heart failure. Insights from the ESCAPE Trial. Circ Heart Fail. 2013;6:264–70.
Nadir AM, Beadle R, Lim HS. Kussmaul physiology in patients with heart failure. Circ Heart Fail. 2014;7:440–7.
Takata M, Beloucif S, Shimada M, Robotham JL. Superior and inferior vena caval flows during respiration: pathogenesis of Kussmaul’s sign. Am J Physiol. 1992;262:H763–70.
Alkhunaizi FA, Harowicz MR, Ireland MR, Houston BA, Damico RL, Kolb TM, et al. Kussmaul’s sign in pulmonary hypertension corresponds with severe pulmonary vascular pathology rather than right ventricular dysfunction. Circ Heart Fail. 2021;14: e007461.
Wenger DS, Krieger EV, Ralph DD, Tedford RJ, Leary PJ. A tale of two hearts: patients with decompensated right heart failure in the intensive care unit. Ann Am Thorac Soc. 2017;14:1025–30.
Potapov E, Meyer D, Swaminathan M, Ramsay M, El Banayosy A, Diehl C, et al. Inhaled nitric oxide after left ventricular assist device implantation: a prospective, randomized double-blind, multicenter, placebo-controlled trial. J Heart Lung Transpl. 2011;30:870–8.
Lim HS, Ranasinghe A, Mascaro J. The physiology of percutaneous right ventricular assist device—potential effects on ventilation-perfusion matching. ASAIO J. 2020;66:e32–42.
Naeije R. Pulmonary vascular resistance. A meaningful variable? Intensive Care Med. 2003;29:526–9.
Tedford RJ, Hassoun PM, Mathai SC, Girgis RE, Russell SD, Cingolani OH, et al. Pulmonary capillary wedge pressure augments right ventricular pulsatile loading. Circulation. 2012;125:289–97.
Lim HS, Gustafsson F. Pulmonary artery pulsatility index: physiological basis and clinical application. Eur J Heart Fail. 2020;22:32–8.
Lim HS. How does protocolization improve outcomes in cardiogenic shock due to end-stage heart failure? Int J Cardiol. 2022. https://doi.org/10.1016/j.ijcard.2022.07.045(Epub ahead of print).
Haas SA, Lange T, Saugel B, Petzoldt M, Fuhrmann V, Metschke M, Kluge S. Severe hyperlactatemia, lactate clearance and mortality in unselected critically ill patients. Intensive Care Med. 2016;42:202–10.
Marbach JA, Stone S, Schwartz B, Pahuja M, Thayer KL, Faugno AJ, et al. Lactate clearance is associated with improved survival in cardiogenic shock: a systematic review and meta-analysis of prognostic factor studies. J Card Fail. 2021;27:1082–9.
Fuernau G, Desch S, de Waha-Thiele S, Eitel I, Neumann FJ, Hennersdorf M, et al. Arterial lactate in cardiogenic shock: prognostic value of clearance versus single values. JACC Cardiovasc Interv. 2020;13:2208–16.
Stacpoole PW, Wright E, Baumgartner TG, Bersin RM, Buchalter S, Curry SH, et al. A controlled clinical trial of dichloroacetate for treatment of lactic acidosis in adults. N Engl J Med. 1992;327:1564–9.
McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Coats AJS, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Kathrine Skibelund A; ESC Scientific Document Group. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;2021(42):3599–726.
Obradovic D, Freund A, Feistritzer HJ, Sulimov D, Loncar G, Abdel-Wahab M, Zeymer U, Desch S, Thiele H. Temporary mechanical circulatory support in cardiogenic shock. Prog Cardiovasc Dis. 2021;69:35–46.
Zeymer U, Bueno H, Granger CB, Hochman J, Huber K, Lettino M, Price S, Schiele F, Tubaro M, Vranckx P, Zahger D, Thiele H. Acute Cardiovascular Care Association position statement for the diagnosis and treatment of patients with acute myocardial infarction complicated by cardiogenic shock: a document of the Acute Cardiovascular Care Association of the European Society of Cardiology. Eur Heart J Acute Cardiovasc Care. 2020;9:183–97.
Ambrosy AP, Vaduganathan M, Mentz RJ, Greene SJ, Subacius H, Konstam MA, et al. Clinical profile and prognostic value of low systolic blood pressure in patients hospitalized for heart failure with reduced ejection fraction: insights from the Efficacy of Vasopressin Antagonism in Heart Failure: Outcome Study with Tolvaptan (EVEREST) trial. Am Heart J. 2013;165:216–25.
Menon V, Slater JN, White HD, Sleeper LA, Cocke T, Hochman JS. Acute myocardial infarction complicated by systemic hypoperfusion without hypotension: report of the SHOCK Trial Registry. Am J Med. 2000;108:374–80.
Maas JJ, de Wilde RB, Aarts LP, Pinsky MR, Jansen JR. Determination of vascular waterfall phenomenon by bedside measurement of mean systemic filling pressure and critical closing pressure in the intensive care unit. Anesth Analg. 2012;114:803–10.
Thiele RH, Nemergut EC, Lynch C 3rd. The clinical implications of isolated alpha (1) adrenergic stimulation. Anesth Analg. 2011;113:297–304.
Lorusso R, Shekar K, MacLaren G, Schmidt M, Pellegrino V, Meyns B, et al. ELSO Interim guidelines for venoarterial extracorporeal membrane oxygenation in adult cardiac patients. ASAIO J. 2021;67:827–44.
Lim HS. Cardiac power output revisited. Circ Heart Fail. 2020;13: e007393.
Lim HS. Conceptualizing liberation from venoarterial extracorporeal membrane oxygenation. Circ Heart Fail. 2022;15: e009183.
Chiolero R, Flatt JP, Revelly JP, Jequier E. Effects of catecholamines on oxygen consumption and oxygen delivery in critically ill patients. Chest. 1991;100:1676–84.
Ostermann M, Hall A, Crichton S. Low mean perfusion pressure is a risk factor for progression of acute kidney injury in critically ill patients—a retrospective analysis. BMC Nephrol. 2017;18:151.
Cheatham ML, Malbrain ML, Kirkpatrick A, Sugrue M, Parr M, De Waele J, Balogh Z, Leppaniemi A, Olvera C, Ivatury R, D’Amours S, Wendon J, Hillman K, Wilmer A. Results from the international conference of experts on intra-abdominal hypertension and abdominal compartment syndrome. II. Recommendations. Intensive Care Med. 2007;33:951–62.
Lim HS. Cardiac power output index to define hemodynamic response to Impella support in cardiogenic shock. Int J Artif Organs. 2022;45:598–603.
Lelubre C, Vincent JL. Red blood cell transfusion in the critically ill patient. Ann Intensive Care. 2011;1:43.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article
Author Contributions
This review was conceived and written by Dr. Lim.
Disclosures
Dr Lim had nothing to disclose.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lim, H.S. Phenotyping and Hemodynamic Assessment in Cardiogenic Shock: From Physiology to Clinical Application. Cardiol Ther 11, 509–522 (2022). https://doi.org/10.1007/s40119-022-00286-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40119-022-00286-2