Abstract
Aim
The review summarizes the recent empirical evidence on the efficacy, safety, and community perception of malaria vaccines in Africa.
Methods
Academic Search Complete, African Journals Online, CINAHL, Medline, PsychInfo, and two gray literature sources were searched in January 2023, and updated in June 2023. Relevant studies published from 2012 were included. Studies were screened, appraised, and synthesized in line with the review aim. Statistical results are presented as 95% Confidence Intervals and proportions/percentages.
Results
Sixty-six (N = 66) studies met the inclusion criteria. Of the vaccines identified, overall efficacy at 12 months was highest for the R21 vaccine (N = 3) at 77.0%, compared to the RTS,S vaccine (N = 15) at 55%. The efficacy of other vaccines was BK-SE36 (11.0–50.0%, N = 1), ChAd63/MVA ME-TRAP (− 4.7–19.4%, N = 2), FMP2.1/AS02A (7.6–9.9%, N = 1), GMZ2 (0.6–60.0%, N = 5), PfPZ (20.0–100.0%, N = 5), and PfSPZ-CVac (24.8–33.6%, N = 1). Injection site pain and fever were the most common adverse events (N = 26), while febrile convulsion (N = 8) was the most reported, vaccine-related Serious Adverse Event. Mixed perceptions of malaria vaccines were found in African communities (N = 17); awareness was generally low, ranging from 11% in Tanzania to 60% in Nigeria (N = 9), compared to willingness to accept the vaccines, which varied from 32.3% in Ethiopia to 96% in Sierra Leone (N = 15). Other issues include availability, logistics, and misconceptions.
Conclusion
Malaria vaccines protect against malaria infection in varying degrees, with severe side effects rarely occurring. Further research is required to improve vaccine efficacy and community involvement is needed to ensure successful widespread use in African communities.
Similar content being viewed by others
Introduction
Malaria is prevalent in Africa and poses a significant public health threat with substantial morbidity and mortality [1]. Despite concerted efforts to curb the disease, its persistence can be attributed to socioeconomic inequality, inadequate infrastructure, and the emergence and spread of drug-resistant strains [2]. Control measures such as insecticide-treated nets (ITNs), indoor residual spraying (IRS), and antimalarial drugs are critical, but additional complementary interventions are needed. One of the promising emergent strategies is vaccination, which has been identified as a potentially pivotal measure in the fight against malaria [3].
Developing a malaria vaccine has been an arduous journey, complicated by the inherent complexity of the Plasmodium parasite's life cycle and its diverse antigenic characteristics [4]. Despite these challenges, there has been substantial progress. One particular advancement in this field is the RTS,S/AS01 and the R21/Matrix-M vaccines. These vaccines demonstrated protective efficacy in large-scale clinical trials, and have been recommended by the World Health Organization (WHO) for use in regions with moderate to high P. falciparum transmission, particularly Sub-Saharan Africa [5].
Malaria vaccine clinical trials have provided important knowledge and insights to support the implementation of large-scale vaccination programs. Mokuolo et al. [6] offered several key learnings from these trials, stressing the significance of robust local regulatory and ethical frameworks, effective community engagement and communication, as well as vigilant monitoring for potential disease enhancement or rebound morbidity following temporary interruptions of clinical infections. A critical factor in the success of vaccine implementation is community acceptance. A recent review of the literature suggests high acceptance of the RTS,S malaria vaccine across low- and middle-income countries (LMICs), with an average acceptance rate of 95.3% [7]. However, acceptance rates vary and appear to be impacted by socio-demographic factors and community apprehensions about safety, efficacy, and vaccine awareness [8, 9].
In light of the success of the RTS,S and R21 vaccines, the need for greater global resources for malaria vaccine research and logistics in vaccine implementation cannot be over-emphasized. This study sought to address a current gap in understanding by using an in-depth scoping review to summarize recent empirical evidence on malaria vaccine efficacy, safety, and community perceptions in Africa.
Methods
A scoping review was conducted using the methodological framework outlined by Arksey and O’Malley [10], incorporated quality recomendations [11], and reported using the PRISMA extension for scoping reviews (PRISMA-ScR), as outlined in Appendix 1 [12]. The review protocol was registered at Open Science Framework (OSF) at https://doi.org/https://doi.org/10.17605/OSF.IO/D54YC.
Eligibility criteria
Studies were included if they evaluated the efficacy, safety, or community perception of a malaria vaccine; were published after 2011; were primary/empirical research; conducted in malaria-endemic African countries; and included the general public as participants (e.g., caregivers, parents, children, or adults). Studies published from 2012 were included as a previous review that have explored malaria vaccine research prior to 2012 [13]. Studies were excluded if the participants were outside Africa, were not primary research (reviews, opinions, editorial, commentaries), and if they evaluated immunogenicity without safety or efficacy as a construct.
Information sources
Five primary databases were searched to identify relevant studies in any language: African Journals Online (AJOL), Academic Search Complete, Medline, CINAHL and PsychInfo. The initial search was conducted in January 2023 for articles published from 2012 to 2022. An update search was conducted in June 2023 for articles published from 2022 to June 2023. The search was supplemented with two gray literature sources; AfricArxiv (Achieve for African Research) and OPUS (Open Publication of UTS Scholars) to identify relevant preprints and thesis/dissertations respectively. Additionally, the reference list of articles that met the inclusion criteria was searched manually and forward literature search on Google Scholar was conducted to identify potentially missing articles. Peer review identified three additional studies published after June 2023 and those studies have also been included.
Search
A combination of MeSh and index terms were formulated based on the PICO framework to aid the search process: Population (P)—African communities, Intervention (I)—malaria vaccine, Comparator (C)—none, and Outcome (O)—efficacy, safety, community perception. The EBSCOhost interface (including Academic Search Complete, CINAHL, Medline with full-text and PsychInfo) and the AJOL database were searched. The full search terms are reported in supplemental Table S1. The EBSCOhost interface was expanded to; ‘Apply related words’ and ‘Apply equivalent subjects’.
For gray literature sources, the term 'malaria vaccine' was used to search for preprints papers on AfricArxiv, and any relevant thesis/publication on OPUS.
Selection of studies
Two reviewers (MC and KA) screened potentially eligible studies using the eligibility criteria. First, exact duplicates were removed in EBSCOhost and the search was narrowed to studies published from January 2012. Search results were then exported to Endnote. The duplicate screening was conducted in Endnote. The remaining articles were independently screened by 2 reviewers based on the title and abstract. The full text of all potentially relevant articles was then retrieved and screened independently by MC and UMB in-line with the eligibility criteria.
Data charting process
A data extraction form was developed by three authors (MC, UMB, DS) and included study characteristics such as the citation, year of publication, study design, and study setting. Data related to the study findings varied based on the focus of the study and included the study methods, the type of malaria vaccine assessed, the outcome assessments used, and the major findings. Two reviewers (KA and MAK) independently conducted the data extraction. Differences were resolved through discussion between the two reviewers and a third reviewer (MC).
Critical appraisal of included studies
The quality of the included studies was assessed using Joanna Briggs Institute (JBI) appraisal tools [14] and the Mixed Methods Appraisal Tool (MMAT) [15]. The appraisal was conducted independently by 2 reviewers (KKD and PB) and differences were resolved by a third reviewer (UMB). No study was excluded based on quality appraisal, but the quality of the study was considered when reaching key conclusions. JBI and MMAT do not provide a scoring guideline, therefore, studies were considered ‘above-average quality’ when they met at least half (average) of the quality criteria assessed in the specific study design. Therefore, the terms ‘below-average quality’ or ‘above-average quality’ were used to refer to study quality in the results.
Data items
Efficacy was operationally defined as the vaccine’s estimated effect on all malaria episodes (clinical, severe, or hospitalization). Efficacy was based on Intention-To-Treat (ITT) or According-To-Protocol/Per Protocol (ATP) analyses. Where ITT and ATP analyses were unavailable, efficacy was based on Hazard Ratio (HR), or any other percentage/proportion estimates reported in the studies. Safety was defined based on the presence or absence of Adverse Event (AE) and/or Serious Adverse Event (SAE). Community perception was defined as the different views of communities (general population) about malaria vaccines.
Synthesis of results
Results were synthesized narratively by summarizing the descriptive numerical data followed by a summary of the textual data. The synthesis considered the nature of the research (e.g., design), the type of malaria vaccine (for efficacy and safety), and the quality of the research studies.
Overall efficacy was classified as positive, none/negative or mixed. A result was considered as having positive efficacy if the Confidence Intervals (CI) were within the positive range; mixed efficacy if the CI ranged from negative to positive; and negative efficacy if the CI was within the negative range to zero. Similarly, safety issues were classified based on the number of subjects presenting with at least one SAE, AE, or none. Where the number of affected subjects were not available, a total number of events/incidents was reported. AEs can be solicited, unsolicited or unexpected, and the cumulative number/range was reported based on available information. For community perception, results were synthesized thematically by reporting the overall quantitative results followed by a summary of qualitative results as applicable. Overall percentages/proportions were reported with a range when available. Community perception was further classified based on 3 components: nature of the vaccine (e.g., risks, effect), systems (e.g., mistrust, logistics), or personal reasons (encompassing anything else). N refers to the number of studies reporting the same finding, while n refers to the number of participants reporting a finding in a study in this review.
Results
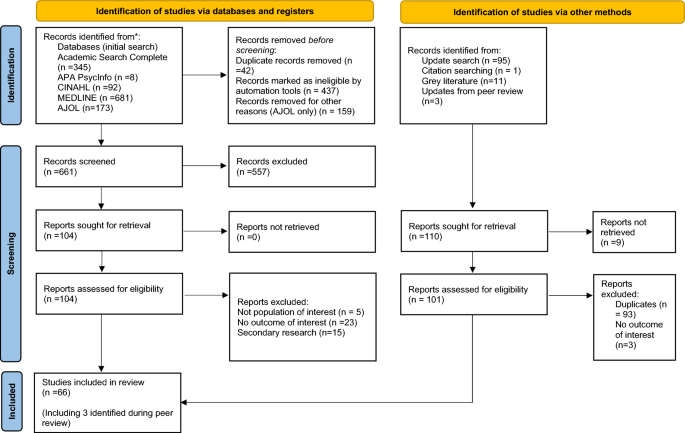
We initially found 1299 articles (Fig. 1) from the five databases, and 661 underwent title/abstract screening. Two non-English articles, in Danish and French, were evaluated and excluded as they were secondary research. In total, 66 studies (N) were included (61 from the main search, 2 from the updated search, and 3 were identified during peer review) [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78].
Characteristics of included studies
The 66 included studies incorporated 47 Randomized Controlled Trials/clinical trials (71.4%), a case–control study (1.6%), and 17 surveys (27.0%). Sixteen African countries were included, with 64 of the 66 studies (97.0%) being above-average quality (Table S2). Further details are presented in Table S3.
Efficacy of malaria vaccines
Half of the included studies (50%, N = 33) reported vaccine efficacy. At 12 months post-vaccination, the R21 vaccine showed the highest overall efficacy at 77% (N = 1, n = 146), compared to the RTS,S vaccine at 55% (N = 1, n = 273). Both of these studies were of above-average quality (Table S2). R21 further demonstrated an efficacy of 79% among younger children (5–17 months compared to 18–36 month-olds) at 12 months [86] and 80% (N = 1, n = 137) at 12 months after a booster dose [78]. Similarly, RTS,S vaccine showed an efficacy of 56% among children aged 5–17 months at 12 months following vaccination [62]. PfSPZ, though tested on only five individuals, demonstrated an efficacy of 100% at three- or eleven-weeks post-vaccination. This efficacy rose from 20 to 100% at 3 weeks when PfSPZ's dosage regimen was adjusted [39]. The combined use of RTS,S/AS01 with chemoprevention yielded efficacy between 59.6 to 60.1% against clinical malaria and outperformed the vaccine in isolation against severe malaria and related deaths [25]. Other vaccines' efficacies varied significantly (Table 1).
Two studies [55, 73] evaluated the long-term (up to 7 years) efficacy of RTS,S on severe and clinical malaria. While the study by Tinto et al. [73] demonstrated a decrease in severe malaria cases over time, there was a rebound against clinical malaria among older children (5–7 years). Oluto et al. [55] identified that vaccine efficacy (clinical malaria) waned over time, including negative efficacy among children with higher exposure to the malaria parasite. Similarly, a negative efficacy of ChAd63/MVA ME-TRAP for an adjusted severe malaria cohort was found [74]. Vaccine effectiveness was maintained when co-administered with malaria chemoprevention [24, 25, 27] or other childhood vaccinations [20].
Safety of malaria vaccines
Thirty-six studies (54.5%, N = 36) investigated the safety of the malaria vaccines, all employing Randomized Controlled Trial design with above-average quality (Table S2). Each study reported one or more AEs (N = 28) or SAEs (N = 23). The reported AEs and SAEs ranged broadly across various vaccines; RTS,S (AEs: 1.6–87.5%, N = 6; SAEs: 2.8–92.2%, N = 12, vaccine-related SAEs: 0.1–1%, N = 7), BK-SE36 (AEs: 5.6–94.4%, N = 1; SAEs: 4.4–5.6%, N = 2), ChAd63/MVA (AEs: 0–100%, N = 6; SAE: 0.4–8.9%, N = 2), FMP2.1/AS02A (SAE: 4%, N = 1), GMZ2 (AEs: 23–100%, N = 2; SAEs: 49–54.5%, N = 2), PfPZ (AEs: 1.6–83.9%, N = 7; SAEs: 1.6%, N = 1), PfAMA1 (AEs: 5–60%, N = 1), PfSPZ-CVac (AEs: 19.4%, N = 1), Pfs25H-EPA (AEs: 100%, N = 1, SAEs: 1.7%, N = 1) and R21 (AEs 0.7–24.6%, N = 1, SAEs: 2.1%, N = 1).
The local and systemic AEs that were typically reported included injection site pain and fever among other symptoms including redness, warmth, discoloration, bruising, erythema, blistering, pruritis, swelling and induration; headache; allergic rash,; drowsiness; irritability; loss of appetite; fatigue; dizziness; abdominal pain; chills; myalgia; diarrhea; nausea and vomiting [18, 20, 30, 31, 37,38,39, 45, 46, 52, 56, 57, 59, 61,62,63,64, 66,67,68,69,70, 72, 74, 75, 77, 86,87,88]. Most AEs subsided within 1–7 days [18, 46, 52, 74, 86].
Commonly reported SAEs were acute gastritis, anemia, bronchitis, cerebral malaria, severe malaria, dehydration, convulsion, febrile convulsion, gastroenteritis, seizures, meningitis, paralytic ileus, pyrexia, pneumonia, respiratory distress, and death. However, most SAEs were.
deemed unrelated to the vaccination (Table 2) and were associated with malaria infection [29, 87]. Only 0.1–1% and 4.3% of SAEs were possibly linked to vaccines, mainly febrile convulsion/seizures, associated with RTS,S vaccine [25, 35, 58, 61,62,63, 66] and R21 vaccine [86] respectively. Malaria vaccine safety when co-administered with other routine childhood immunization was identified [20, 46].
Community perception of malaria vaccine
Seventeen studies (27.0%, N = 17) assessed community perception of malaria vaccines, with a mix of below and above-average quality studies (Table S2). The overall perception of participants has been summarized in addition to five key issues that emerged from the studies: acceptance, availability, knowledge/awareness, logistics, and misconceptions about the vaccines (Table 3).
Overall perception
Ten of the seventeen studies that assessed community perception (58.8%) reported their overall perception of malaria vaccines (Table 3), and were of below and above-average quality (Table S2). Community members agreed that it was essential to have a malaria vaccine [44] and that the vaccine is necessary for malaria control [33]. More than three-quarters of participants from each study reported overall positive perceptions [26, 36, 47, 48], identified malaria as a risk for their children [36], and identified that the vaccine will keep children healthy [23, 44] even though the efficacy of the vaccine may not be 100% [47]. A significant positive association between positive perception and intent to comply with vaccination was reported [26]. More than half of respondents recommend the vaccine to others [48] and were part of the National Program on Immunisation [33, 48]. The majority of participants preferred vaccines to malaria drugs/vector control [28, 34]. There was a mixed reaction between oral and injectable vaccines in Ghana [44], while in Tanzania, participants were open to all modes of administration [60]. The limited side effects experienced by participants in the RTS,S/AS01 vaccine trial reinforced participants’ beliefs about its safety in Nigeria [28].
Acceptance
Of the studies examined, 88.2%, (N = 15) reported acceptance of malaria vaccines (Table 3), and most studies were above-average quality (Table S2). Acceptance rates varied from 32.3% in Ethiopia [21] to 96% in Sierra Leone [43]. Acceptance increased to 98.9% in malaria-endemic areas in Kenya [53]. Key drivers for acceptance were the high risk of malaria in children [17, 41], the desire for self-protection and prevention [41, 43], and incentives such as free consultations and medication [17].
The impact of religion on vaccine acceptance was inconsistent [36, 47, 71]. Some findings showed that Christian mothers were more likely to accept the vaccine than Muslim mothers in Tanzania [47], while in Ghana [36] and Nigeria [71], Christian mothers showed lower odds of accepting the vaccine. Free provision significantly increased vaccine acceptance [41, 43], while increased costs decreased acceptance [41, 76].
Fear of adverse events and unsuccessful intravenous vaccination attempts were linked to vaccine refusal [23, 43, 44, 71]. Factors such as marital status, region, knowledge of vaccine, tribe, education level, prior vaccination experience, satisfaction with healthcare services, and parent age influenced willingness to accept vaccination [21, 33, 41, 47, 53, 76].
Availability
Two of the studies (11.8%) reported concerns associated with the availability of malaria vaccines (Table 3). The need to provide malaria vaccine to adults in addition to children was reported in Mozambique [23]. The importance of an adequate supply chain to promote availability was documented from a key informant interview in Sierra Leone [43].
Knowledge/awareness
Nine of the studies (52.9%) reported knowledge of participants about malaria vaccines (Table 3). The percentage of participants having awareness of malaria vaccines ranged from 11% in Tanzania [60] to 60% in Nigeria [33]. Additionally, there was a low willingness to learn more about the vaccine in Mozambique [23]. Confusion and delays related to trial designs were seen to discourage participation in a malaria vaccine trial in Kenya [17]. The use of mass media, particularly Television, radio, and phones were identified as good sources of information by participants [23, 26, 44]. Information vans, health talks, and information from trusted community members [44] or health professionals were important but were rated equally with internet sources [71]. Awareness of vaccines was higher in older people when compared to younger people [36] and in mothers of Christian children compared to the Islamic faith [36]. There was evidence of confusion about malaria vaccines and other childhood vaccines in Ghana [44].
Logistics
Four of the studies (23.5%) reported findings related to the logistics associated with malaria vaccine enrolments (Table 3). The need for community outreach by community health workers, including malaria vaccine campaigns alongside existing vector control programs to encourage participation was reported [43]. Negative attitudes of health staff were reported and shown to discourage participation in malaria vaccine trials [17]. Similarly, the system’s capacity to train staff for intravenous administration was noted as important [17].
Parents’ willingness to pay for the malaria vaccine was reported as a barrier [26, 28, 43]. Although, affordability was noted as a concern in a number of studies [26, 28, 41, 76], some participants suggested that the provision of malaria vaccines was the sole responsibility of the government [28].
Misconceptions
Four of the studies (23.5%) reported misconceptions about potential malaria vaccines. Rumors of blood ‘theft and selling’ were linked to early withdrawal from malaria vaccine trials in Kenya [17]. Similarly, a widespread belief that newborns should have minimum exposure to adults and that the presence of a vaccine scar signifies a nurse had sexual intercourse with the child hindered vaccination programs in Mozambique [23]. The ideology that vaccines are harmful and can cause sickness was reported as a fear preventing vaccinations [23, 43]. Furthermore, rumors of vaccines causing infertility and system mistrust were cited as critical reasons for hesitancy to receive the malaria vaccine [43, 71].
Discussion
This paper summarizes recent evidence on the efficacy, safety, and perception of malaria vaccines in Africa. All vaccines studied showed some degree of protection in terms of reducing the risk of contracting malaria and/or eliciting an antibody response. Overall efficacy varied; the highest overall efficacy (77%) was observed with R21 [30], which increased to 80% with a booster dose [78]. Increasing the dosage regimen of PfSPZ may also lead to an increase in efficacy from 20 to 100% [39]. Vaccination efficacy decreases over time with the highest efficacy expected up to one year after the last dose [55, 73]. R21 showed increased efficacy between six months (74%) to one year (77%) after vaccination [30]. RTS,S, was the most-studied vaccine. RTS,S showed good efficacy (55%) up to one year after vaccination, but this decreased over time [24, 55], with efficacy around zero after four years and negative in areas with high malaria exposure at five years of follow-up [55]. RTS,S was found to prevent clinical malaria cases in infants and children over three to four years and was further enhanced by administering a booster dose [63]. Emerging evidence suggests that the efficacy of vaccines like RTS,S increases when combined with seasonal malaria chemoprophylaxis [63]. The concomitant use of malaria vaccines with other control measures is therefore seen to be an important mitigation strategy in areas of high transmission.
Adverse events were reported in all studies. The most common adverse events were injection site pain and fever. Most adverse events were reported to subside within one week of appearance. Serious adverse events were rare (0.1–1%). Serious adverse events can occur following vaccinations, with about 1% of participants developing events such as febrile convulsions following malaria vaccines [23, 25, 35, 58, 61,62,63]. This was particularly observed in children within 2–3 days of receiving the RTS,S vaccine [35]. It is therefore possible that adverse events may arise following vaccination; however, further research is required.
Fear of unknown side effects associated with vaccines, especially newly developed ones, are often associated with low levels of acceptance [79]. Willingness to accept the malaria vaccine ranges from 32.3% in Ethiopia to 96% in Sierra Leone [21, 26]. However, a number of factors are likely to affect the use of malaria vaccines in many African communities, including inadequate knowledge, misconceptions, availability of vaccines, and logistics.
This review has identified that knowledge about malaria vaccines is not widespread throughout Africa. Vaccine awareness was slightly lower than vaccine acceptance; however, people may have been reluctant to accept the newly developed malaria vaccines because of generalized vaccine hesitancy in some parts of Africa. Vaccine hesitancy has been reported in the literature as a consequence of misinformation about vaccine origin, efficacy, and safety, and psychological factors such as anxiety [80, 81]. In addition to these factors, political influences, religious beliefs, and low perception of risk combine to contribute to vaccination rates in sub-Saharan Africa [79, 80]. The extent of vaccination hesitancy may vary according to people's commitment to health protection and risk culture and their trust in conventional medicine and public health authorities. Evidence from the literature suggests that the lack of willingness to vaccinate may be due to a lack of knowledge, indifference, and irregular vaccination behavior [82]. Public education campaigns on vaccination programs are therefore important to support behavior change.
The findings of this review could assist public health experts and policymakers in Africa to develop and implement strategies to address the low acceptance and use of malaria vaccines. Wide-spread adoption of malaria vaccines is possible if awareness campaigns provide adequate factual explanations to counter rumors and mis-information [6, 83]. Increasing local vaccine production within the African continent may further promote the use of malaria vaccines. Local production may help reduce mistrust through technology transfer. To raise awareness about vaccination, it is important to take a context-specific approach involving community and religious leaders [84, 85]. The provision of credible information to communities by trusted sources is an important strategy to promote vaccination uptake.
There are some limitations to this review. Due to recent advances in malaria vaccines and the recommendations of Schwartz et al. [9] only studies published since 2012 were included. The scope of this review summarizes the existing evidence and highlights areas for more in-depth analysis in the future.
Conclusion
Different types of malaria vaccines have different efficacy levels, and combining seasonal malaria prophylaxis with a malaria vaccine might increase effectiveness. A variable degree of protection from malaria infection is provided by malaria vaccines with severe adverse events only occurring rarely. Many African communities have a high perception of malaria vaccines, but knowledge of the vaccine is relatively low. Further research and community involvement are needed to respectively improve vaccine efficacy and ensure successful widespread use in African communities.
Data availability
All data used in this review will be made available on request through the corresponding author.
References
World Health Organization. World malaria report: 20 years of global progress and challenges. https://www.who.int/publications/i/item/9789240015791. 2020.
Alonso P, Noor AM. The global fight against malaria is at crossroads. The Lancet. 2017;390:2532–4.
Kanoi BN, Maina M, Likhovole C, Kobia FM, Gitaka J. Malaria vaccine approaches leveraging technologies optimized in the COVID-19 era. Front Trop Dis. 2022. https://doi.org/10.3389/fitd.2022.988665.
Etefia E, Etoh PI. Malaria vaccine development: challenges and prospects. Med Pharm J. 2023;2023:28–42.
World Health Organization malaria vaccine implementation programme.
Mokuolu OA, Bolarinwa OA, Opadiran OR, Ameen HA, Dhorda M, Cheah PY, et al. A framework for stakeholder engagement in the adoption of new anti-malarial treatments in Africa: a case study of Nigeria. Malar J. 2023;22:1–13. https://doi.org/10.1186/s12936-023-04622-2.
Sulaiman SK, Musa MS, Tsiga-Ahmed FI, Dayyab FM, Sulaiman AK, Bako AT. A systematic review and meta-analysis of the prevalence of caregiver acceptance of malaria vaccine for under-five children in low-income and middle-income countries (LMICs). PLoS One. 2022. https://doi.org/10.1371/journal.pone.0278224.
Mumtaz H, Nadeem A, Bilal W, Ansar F, Saleem S, Khan QA, et al. Acceptance, availability, and feasibility of RTS, S/AS01 malaria vaccine: a review. Immun Inflamm Dis. 2023;11: e899. https://doi.org/10.1002/iid3.899.
Dimala CA, Kika BT, Kadia BM, Blencowe H. Current challenges and proposed solutions to the effective implementation of the RTS, S/AS01 Malaria vaccine program in sub-Saharan Africa: a systematic review. PLoS ONE. 2018;13: e0209744.
Arksey H, O’Malley L. 2005. Scoping studies: towards a methodological framework. https://doi.org/10.1080/1364557032000119616
Cooper S, Cant R, Kelly M, Levett-Jones T, McKenna L, Seaton P, et al. An evidence-based checklist for improving scoping review quality. Clin Nurs Res. 2019;30:230–40. https://doi.org/10.1177/1054773819846024.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation ann intern med. Am College Phys. 2018. https://doi.org/10.7326/M18-0850.
Schwartz L, Brown GV, Genton B, Moorthy VS. A review of malaria vaccine clinical projects based on the WHO rainbow table. Malar J. 2012. https://doi.org/10.1186/1475-2875-11-11.
Joanna Briggs Institute. JBI Critical appraisal tools. https://jbi.global/critical-appraisal-tools.
Hong QN, Pluye P, Fàbregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed method appraisal tool (MMAT) Version 2018 - User guide. Montreal. 2018. http://mixedmethodsappraisaltoolpublic.pbworks.com/
Abdulla S, Salim N, Machera F, Kamata R, Juma O, Shomari M, et al. Randomized, controlled trial of the long term safety, immunogenicity and efficacy of RTS, S/AS02D malaria vaccine in infants living in a malaria-endemic region. Malar J. 2013. https://doi.org/10.1186/1475-2875-12-11.
Achieng F, Rosen JG, Cherop RY, Kariuki S, Hoffman SL, Seder R, et al. Caregiver and community perceptions and experiences participating in an infant malaria prevention trial of PfSPZ Vaccine administered by direct venous inoculation: a qualitative study in Siaya County, western Kenya. Malar J. 2020. https://doi.org/10.1186/s12936-020-03293-7.
Afolabi MO, Tiono AB, Adetifa UJ, Yaro JB, Drammeh A, Nébié I, et al. Safety and Immunogenicity of ChAd63 and MVA ME-TRAP in West African Children and Infants. Mol Ther. 2016;24:1470–7.
Ajua A, Lell B, Agnandji ST, Asante KP, Owusu-Agyei S, Mwangoka G, et al. The effect of immunization schedule with the malaria vaccine candidate RTS, S/AS01E on protective efficacy and anti-circumsporozoite protein antibody avidity in African infants. Malar J. 2015. https://doi.org/10.1186/s12936-015-0605-7.
Asante KP, Ansong D, Kaali S, Adjei S, Lievens M, Nana Badu L, et al. Immunogenicity and safety of the RTS, S/AS01 malaria vaccine co-administered with measles, rubella and yellow fever vaccines in Ghanaian children: a phase IIIb, multi-center, non-inferiority, randomized, open, controlled trial. Vaccine. 2020;38:3411–21.
Asmare G. Willingness to accept malaria vaccine among caregivers of under-5 children in Southwest Ethiopia: a community based cross-sectional study. Malar J. 2022. https://doi.org/10.1186/s12936-022-04164-z.
Bejon P, White MT, Olotu A, Bojang K, Lusingu JPA, Salim N, et al. Efficacy of RTS, S malaria vaccines: individual-participant pooled analysis of phase 2 data. Lancet Infect Dis. 2013;13:319–27.
Bingham A, Gaspar F, Lancaster K, Conjera J, Collymore Y, Ba-Nguz A. Community perceptions of malaria and vaccines in two districts of Mozambique. Malar J. 2012. https://doi.org/10.1186/1475-2875-11-394.
Cairns M, Barry A, Zongo I, Sagara I, Yerbanga SR, Diarra M, et al. The duration of protection against clinical malaria provided by the combination of seasonal RTS, S/AS01E vaccination and seasonal malaria chemoprevention versus either intervention given alone. BMC Med. 2022. https://doi.org/10.1186/s12916-022-02536-5.
Chandramohan D, Zongo I, Sagara I, Cairns M, Yerbanga R-S, Diarra M, et al. Seasonal malaria vaccination with or without seasonal malaria chemoprevention. N Engl J Med. 2021;385:1005–17.
Chukwuocha UM, Okorie PC, Iwuoha GN, Ibe SN, Dozie IN, Nwoke BE. Awareness, perceptions and intent to comply with the prospective malaria vaccine in parts of South Eastern Nigeria. Malar J. 2018. https://doi.org/10.1186/s12936-018-2335-0.
Coulibaly D, Kone AK, Traore K, Niangaly A, Kouriba B, Arama C, et al. PfSPZ-CVac malaria vaccine demonstrates safety among malaria-experienced adults: a randomized, controlled phase 1 trial. EClinicalMedicine. 2022. 52.
Darkwa S, de Wildt G, Dalaba M, Vidzro E, Ansah EK. “I would have to sell things in order to get the money”: a qualitative exploration of willingness to pay for the RTS, S/AS01 malaria vaccine in the Volta region Ghana. PLoS One. 2022. https://doi.org/10.1371/journal.pone.0268009.
Dassah S, Adu B, Sirima SB, Mordmüller B, Ngoa UA, Atuguba F, et al. Extended follow-up of children in a phase2b trial of the GMZ2 malaria vaccine. Vaccine. 2021;39:4314–9.
Datoo MS, Natama MH, Somé A, Traoré O, Rouamba T, Bellamy D, et al. Efficacy of a low-dose candidate malaria vaccine, R21 in adjuvant Matrix-M, with seasonal administration to children in Burkina Faso: a randomised controlled trial. The Lancet. 2021;397:1809–18.
Dejon-Agobe JC, Ateba-Ngoa U, Lalremruata A, Homoet A, Engelhorn J, Nouatin OP, et al. Controlled human malaria infection of healthy adults with lifelong malaria exposure to assess safety, immunogenicity, and efficacy of the asexual blood stage malaria vaccine candidate GMZ2. Clin Infect Dis. 2019;69:1377–84.
Dobanõ C, Ubillos I, Jairoce C, Gyan B, Vidal M, Jiménez A, et al. RTS, S/AS01E immunization increases antibody responses to vaccine-unrelated Plasmodium falciparum antigens associated with protection against clinical malaria in African children: a case-control study. BMC Med. 2019. https://doi.org/10.1186/s12916-019-1378-6.
Etokidem AJ, Ndifon WO, Asibong UE. Perception and acceptability of malaria vaccine among maternal and child health clinic attendees at the University of Calabar teaching Hospital, Calabar, Nigeria. J Commun Med Primary Health Care. 2015;27:51.
Febir LG, Asante KP, Dzorgbo D-BS, Senah KA, Letsa TS, Owusu-Agyei S. Community perceptions of a malaria vaccine in the Kintampo districts of Ghana. Malaria J. 2013. https://doi.org/10.1186/1475-2875-12-156.
Guerra Mendoza Y, Garric E, Leach A, Lievens M, Ofori-Anyinam O, Pirçon JY, et al. Safety profile of the RTS, S/AS01 malaria vaccine in infants and children: additional data from a phase III randomized controlled trial in sub-Saharan Africa. Hum Vaccin Immunother. 2019;15:2386–98.
Immurana M, Boachie MK, Klu D, Dalaba MA, Manyeh AK, Alhassan RK. Determinants of willingness to accept child vaccination against malaria in Ghana. Int J Health Planning Manage. 2022;37:1439–53.
Jongo SA, Shekalaghe SA, Preston Church LW, Ruben AJ, Schindler T, Zenklusen I, et al. Safety, immunogenicity, and protective efficacy against controlled human malaria infection of plasmodium falciparum sporozoite vaccine in Tanzanian adults. Am J Trop Med Hyg. 2018;99:338–49.
Jongo SA, Church LWP, Mtoro AT, Chakravarty S, Ruben AJ, Swanson PA, et al. Safety and differential antibody and T-cell responses to the plasmodium falciparum sporozoite malaria vaccine, PfSPZ vaccine, by age in tanzanian adults, adolescents, children, and infants. American Journal of Tropical Medicine and Hygiene. American Society of Tropical Medicine and Hygiene. 2019.
Jongo SA, Preston Church LW, Mtoro AT, Schindler T, Chakravarty S, Ruben AJ, et al. Increase of dose associated with decrease in protection against controlled human malaria infection by PfSPZ vaccine in Tanzanian adults. Clin Infect Dis. 2020;71:2849–57.
Jongo SA, Urbano V, Preston Church LW, Olotu A, Manock SR, Schindler T, et al. Immunogenicity and protective efficacy of radiation-attenuated and chemo-attenuated PfSPZ vaccines in equatoguinean adults. Am J Trop Med Hyg. 2021;104:283–93.
Kpanake L, Sorum PC, Mullet E. The potential acceptability of infant vaccination against malaria: a mapping of parental positions in Togo. Vaccine. 2016;34:408–12.
Laurens MB, Thera MA, Coulibaly D, Ouattara A, Kone AK, Guindo AB, et al. Extended safety, immunogenicity and efficacy of a blood-stage malaria vaccine in Malian children: 24-Month follow-up of a randomized, double-blinded phase 2 trial. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0079323.
McCoy KD, Weldon CT, Ansumana R, Lamin JM, Stenger DA, Ryan SJ, et al. Are malaria transmission-blocking vaccines acceptable to high burden communities? Results from a mixed methods study in Bo Sierra Leone. Malar J. 2021. https://doi.org/10.1186/s12936-021-03723-0.
Meñaca A, Tagbor H, Adjei R, Bart-Plange C, Collymore Y, Ba-Nguz A, et al. Factors likely to affect community acceptance of a malaria vaccine in two districts of ghana: a qualitative study. PLoS One. 2014. https://doi.org/10.1371/journal.pone.0109707.
Mensah VA, Gueye A, Ndiaye M, Edwards NJ, Wright D, Anagnostou NA, et al. Safety, immunogenicity and efficacy of prime-boost vaccination with chad63 and mva encoding me-trap against plasmodium falciparum infection in adults in senegal. PLoS One. 2016. https://doi.org/10.1371/journal.pone.0167951.
Mensah VA, Roetynck S, Kanteh EK, Bowyer G, Ndaw A, Oko F, et al. Safety and immunogenicity of malaria vectored vaccines given with routine expanded program on immunization vaccines in gambian infants and neonates: a randomized controlled trial. Front Immunol. 2017. https://doi.org/10.3389/fimmu.2017.01551.
Mtenga S, Kimweri A, Romore I, Ali A, Exavery A, Sicuri E, et al. Stakeholders’ opinions and questions regarding the anticipated malaria vaccine in Tanzania. Malar J. 2016. https://doi.org/10.1186/s12936-016-1209-6.
Musa S, Olorukooba AA, Muhammad NS, Muhammad B, Makarfi HU. Awareness, perception and acceptance of malaria vaccine among women of the reproductive age group in a rural community in Soba, Kaduna State North-west Nigeria. Kanem J Med Sci. 2022;16:32.
Neafsey DE, Juraska M, Bedford T, Benkeser D, Valim C, Griggs A, et al. Genetic diversity and protective efficacy of the RTS, S/AS01 malaria vaccine. N Engl J Med. 2015;373:2025–37.
Nouatin O, Ateba Ngoa U, Ibáñez J, Dejon-Agobe JC, Mordmüller B, Edoa JR, et al. Effect of immune regulatory pathways after immunization with GMZ2 malaria vaccine candidate in healthy lifelong malaria-exposed adults. Vaccine. 2020;38:4263–72.
Nouatin O, Ibáñez J, Fendel R, Ngoa UA, Lorenz FR, Dejon-Agobé JC, et al. Cellular and antibody response in GMZ2-vaccinated Gabonese volunteers in a controlled human malaria infection trial. Malar J. 2022. https://doi.org/10.1186/s12936-022-04169-8.
Ogwang C, Afolabi M, Kimani D, Jagne YJ, Sheehy SH, Bliss CM, et al. Safety and immunogenicity of heterologous prime-boost Immunisation with Plasmodium falciparum malaria candidate vaccines, ChAd63 ME-TRAP and MVA ME-TRAP, in healthy Gambian and Kenyan Adults. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0057726.
Ojakaa DI, Jarvis JD, Matilu MI, Thiam S. Acceptance of a malaria vaccine by caregivers of sick children in Kenya. Malar J. 2014. https://doi.org/10.1186/1475-2875-13-172.
Olotu A, Fegan G, Wambua J, Nyangweso G, Awuondo KO, Leach A, et al. Four-year efficacy of RTS, S/AS01E and its interaction with malaria exposure. N Engl J Med. 2013;368:1111–20.
Olotu A, Fegan G, Wambua J, Nyangweso G, Leach A, Lievens M, et al. Seven-year efficacy of RTS, S/AS01 Malaria vaccine among young African children. N Engl J Med. 2016;374:2519–29.
Olotu A, Urbano V, Hamad A, Eka M, Chemba M, Nyakarungu E, et al. Advancing global health through development and clinical trials partnerships: a randomized, placebo-controlled, double-blind assessment of safety, tolerability, and immunogenicity of pfspz vaccine for malaria in healthy equatoguinean men. Am J Trop Med Hyg. 2018;98:308–18.
Oneko M, Steinhardt LC, Yego R, Wiegand RE, Swanson PA, Kc N, et al. Safety, immunogenicity and efficacy of PfSPZ Vaccine against malaria in infants in western Kenya: a double-blind, randomized, placebo-controlled phase 2 trial. Nat Med. 2021;27:1636–45.
Otieno L, Guerra Mendoza Y, Adjei S, Agbenyega T, Agnandji ST, Aide P, et al. Safety and immunogenicity of the RTS, S/AS01 malaria vaccine in infants and children identified as HIV-infected during a randomized trial in sub-Saharan Africa. Vaccine. 2020;38:897–906.
Palacpac NMQ, Ntege E, Yeka A, Balikagala B, Suzuki N, Shirai H, et al. Phase 1b randomized trial and follow-up study in Uganda of the blood-stage malaria vaccine candidate BK-SE36. PLoS One. 2013. https://doi.org/10.1371/journal.pone.0064073.
Romore I, Ali AM, Semali I, Mshinda H, Tanner M, Abdulla S. Assessment of parental perception of malaria vaccine in Tanzania. Malar J. 2015. https://doi.org/10.1186/s12936-015-0889-7.
RTSS Clinical Trial Partnership. a phase 3 trial of RTS, S/AS01 malaria vaccine in african infants. New England J Med. 2012;367:2284–95. https://doi.org/10.1056/NEJMoa1208394.
RTSS Clinical Trial Partnership. Efficacy and safety of the RTS, S/AS01 malaria vaccine during 18 months after vaccination: a phase 3 randomized, controlled trial in children and young infants at 11 African Sites. PLoS Med. 2014. https://doi.org/10.1371/journal.pmed.1001685.
RTSS Clinical Trial Partnership. Efficacy and safety of RTS, S/AS01 malaria vaccine with or without a booster dose in infants and children in Africa: Final results of a phase 3, individually randomised, controlled trial. The Lancet. 2015;386:31–45.
Sagara I, Healy SA, Assadou MH, Gabriel EE, Kone M, Sissoko K, et al. Safety and immunogenicity of Pfs25H-EPA/Alhydrogel, a transmission-blocking vaccine against Plasmodium falciparum: a randomised, double-blind, comparator-controlled, dose-escalation study in healthy Malian adults. Lancet Infect Dis. 2018;18:969–82.
Sagara I, Zongo I, Cairns M, Yerbanga RS, Mahamar A, Nikièma F, et al. The anti-circumsporozoite antibody response of children to seasonal vaccination with the RTS, S/AS01Emalaria vaccine. Clin Infect Dis. 2022;75:613–22.
Samuels AM, Ansong D, Kariuki SK, Adjei S, Bollaerts A, Ockenhouse C, et al. Efficacy of RTS, S/AS01E malaria vaccine administered according to different full, fractional, and delayed third or early fourth dose regimens in children aged 5–17 months in Ghana and Kenya: an open-label, phase 2b, randomised controlled trial. Lancet Infect Dis. 2022;22:1329–42.
Sirima SB, Mordmüller B, Milligan P, Ngoa UA, Kironde F, Atuguba F, et al. A phase 2b randomized, controlled trial of the efficacy of the GMZ2 malaria vaccine in African children. Vaccine. 2016;34:4536–42.
Sissoko MS, Healy SA, Katile A, Omaswa F, Zaidi I, Gabriel EE, et al. Safety and efficacy of PfSPZ vaccine against Plasmodium falciparum via direct venous inoculation in healthy malaria-exposed adults in mali: a randomised, double-blind phase 1 trial. Lancet Infect Dis. 2017;17:498–509.
Sissoko MS, Healy SA, Katile A, Zaidi I, Hu Z, Kamate B, et al. Safety and efficacy of a three-dose regimen of Plasmodium falciparum sporozoite vaccine in adults during an intense malaria transmission season in mali: a randomised, controlled phase 1 trial. Lancet Infect Dis. 2022;22:377–89.
Steinhardt LC, Richie TL, Yego R, Akach D, Hamel MJ, Gutman JR, et al. Safety, tolerability, and immunogenicity of plasmodium falciparum sporozoite vaccine administered by direct venous inoculation to infants and young children: findings from an age de-escalation, dose-escalation, double-blind, randomized controlled study in Western Kenya. Clin Infect Dis. 2020;71:1063–71.
Sulaiman SK, Tsiga-Ahmed FI, Musa MS, Sulaiman AK, Dayyab FM, Khan MA, et al. Prevalence, determinants, and reasons for malaria vaccine hesitancy among caregivers of under-five children in Nigeria: results from a nationwide cross-sectional survey. Vaccine. 2023;41:1503–12.
Thera MA, Coulibaly D, Kone AK, Guindo AB, Traore K, Sall AH, et al. Phase 1 randomized controlled trial to evaluate the safety and immunogenicity of recombinant Pichia pastoris-expressed Plasmodium falciparum apical membrane antigen 1 (PfAMA1-FVO [25–545]) in healthy Malian adults in Bandiagara. Malar J. 2016;15:1–11.
Tinto H, Otieno W, Gesase S, Sorgho H, Otieno L, Liheluka E, et al. Long-term incidence of severe malaria following RTS, S/AS01 vaccination in children and infants in Africa: an open-label 3-year extension study of a phase 3 randomised controlled trial. Lancet Infect Dis. 2019;19:821–32.
Tiono AB, Nébié I, Anagnostou N, Coulibaly AS, Bowyer G, Lam E, et al. First field efficacy trial of the ChAd63 MVA ME-TRAP vectored malaria vaccine candidate in 5–17 months old infants and children. PLoS One. 2018;13:208328.
Umeh R, Oguche S, Oguonu T, Pitmang S, Shu E, Onyia JT, et al. Immunogenicity and safety of the candidate RTS, S/AS01 vaccine in young Nigerian children: a randomized, double-blind, lot-to-lot consistency trial. Vaccine. 2014;32:6556–62.
Vera Cruz G, Humeau A, Kpanake L, Sorum PC, Mullet E. Infant vaccination against malaria in Mozambique and in Togo: mapping parents’ willingness to get their children vaccinated. Hum Vaccin Immunother. 2020;16:539–47.
Witte D, Cunliffe NA, Turner AM, Ngulube E, Ofori-Anyinam O, Vekemans J, et al. Safety and immunogenicity of seven dosing regimens of the candidate RTS, S/AS01E Malaria vaccine integrated within an expanded program on immunization Regimen: a phase II, single-center, open, controlled trial in infants in Malawi. Pediatric Infect Disease J. 2018;37:483–91.
Datoo MS, Natama HM, Somé A, Bellamy D, Traoré O, Rouamba T, et al. Efficacy and immunogenicity of R21/Matrix-M vaccine against clinical malaria after 2 years’ follow-up in children in Burkina Faso: a phase 1/2b randomised controlled trial. Lancet Infect Dis. 2022;22:1728–36.
Chutiyami M, Bello UM, Salihu D, Kolo MA, Alsharari AF, Sabo H, et al. Subjective reasons for COVID-19 vaccine hesitancy and sociodemographic predictors of vaccination in Nigeria: an online survey. COVID. 2022;2:1329–40.
Kabakama S, Konje ET, Dinga JN, Kishamawe C, Morhason-Bello I, Hayombe P, et al. Commentary on COVID-19 Vaccine Hesitancy in sub-Saharan Africa. Trop Med Infect Dis MDPI. 2022;77:130.
Chutiyami M, Salihu D, Bello UM, Winser SJ, Gambo AA, Sabo H, et al. Are fear of COVID-19 and vaccine hesitancy associated with COVID-19 vaccine uptake? A population-based online survey in Nigeria. Vaccines. 2022;10:1271.
Peretti-Watel P, Larson HJ, Ward JK, Schulz WS, Verger P. Vaccine hesitancy: clarifying a theoretical framework for an ambiguous notion. PLoS Curr. 2015;25:7.
Grant J, Gyan T, Agbokey F, Webster J, Greenwood B, Asante KP. Challenges and lessons learned during the planning and early implementation of the RTS, S/AS01E malaria vaccine in three regions of Ghana: a qualitative study. Malar J. 2022. https://doi.org/10.1186/s12936-022-04168-9.
Greenwood BM. Control to elimination: implications for malaria research. Trends Parasitol. 2008;24:449–54.
Moorthy VS, Newman RD, Okwo-Bele JM. Malaria vaccine technology roadmap. Lancet. 2013;382:1700–1.
Datoo MM, Dicko A, Tinto H, Ouédraogo JB, Hamaluba M, Olotu A, Beaumont E, Ramos-Lopez F, Magloire Natama H, Weston S, Chemba M. A Phase III randomised controlled trial evaluating the malaria vaccine candidate R21/Matrix-M™ in African children. 2023. https://doi.org/10.2139/ssrn.4584076
Ouédraogo A, Bougouma EC, Palacpac NM, Houard S, Nebie I, Sawadogo J, Berges GD, Soulama I, Diarra A, Hien D, Ouedraogo AZ. Safety and immunogenicity of BK-SE36/CpG malaria vaccine in healthy Burkinabe adults and children: a phase 1b randomised, controlled, double-blinded, age de-escalation trial. Front Immunol. 2023;16:1267372. https://doi.org/10.3389/fimmu.2023.1267372.
Silk SE, Kalinga WF, Mtaka IM, Lilolime NS, Mpina M, Milando F, Ahmed S, Diouf A, Mkwepu F, Simon B, Athumani T. Superior antibody immunogenicity of a viral-vectored RH5 blood-stage malaria vaccine in Tanzanian infants as compared to adults. Med. 2023;4:668–86. https://doi.org/10.1016/j.medj.2023.07.003.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The University of Technology Sydney fully supported the open-access publication of this article as part of its open-access agreement with Springer Nature.
Author information
Authors and Affiliations
Contributions
MC: Conceptualization, protocol and registration, search strategies, article screening, analysis and synthesis, and manuscript drafting. PS: Accessed and verified data, analysis, and manuscript drafting. UMB: Conceptualization, review of quality rating, data analysis, manuscript drafting. DS: Accessed and verified data, conceptualization, data analysis, and manuscript drafting. KA: primary databases search, article screening and data extraction. MAK: data extraction and manuscript drafting. KKD: Quality rating and manuscript drafting. DH: data extraction and manuscript drafting. PB: Quality rating. SKS: Other electronic searches and manuscript drafting. JS: Data verification, qualitative data synthesis, technical and language editing of the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
All authors declare that there are no conflict of interests.
Additional information
Registration at OSF: https://doi.org/10.17605/OSF.IO/D54YC
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chutiyami, M., Saravanakumar, P., Bello, U.M. et al. Malaria vaccine efficacy, safety, and community perception in Africa: a scoping review of recent empirical studies. Infection (2024). https://doi.org/10.1007/s15010-024-02196-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02196-y