Abstract
Purpose
This aimed to identify the factors associated with severe/critical coronavirus disease 2019 (COVID-19) infection in rheumatoid arthritis (RA) patients.
Methods
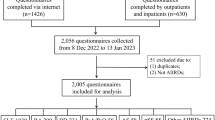
Two-hundred RA patients diagnosed according to the American College of Rheumatology/ European League Against Rheumatism (ACR/EULAR) classification criteria with proven COVID-19 infection were recruited and categorized according to the world health organization (WHO) COVID-19 severity grading into 2 groups: patients with mild/moderate COVID-19 (n = 164) and patients with severe/critical COVID-19 (n = 36). Comparison between both groups was done to identify the risk factors associated with severe/critical infection. Incidence of RA disease activity flare defined as increase in clinical disease activity index (CDAI) more than 10 points following infection was calculated.
Results
Multivariate analysis identified history of previous serious infection, age > 60 years, and diabetes as factors positively associated, whereas COVID-19 vaccination was negatively associated with severe/critical infection. Following COVID-19 infection, the number of patients with severe/critical COVID-19 who had high RA disease activity and the incidence of flares was significantly higher in comparison to patients with mild/moderate COVID-19 (P < 0.001 and 0.003; respectively).
Conclusion
Age > 60 years, diabetes, and history of previous serious infections are risk factors for severe/critical COVID-19, while vaccination has a protective role in RA patients. Infection particularly when severe is associated with risk of disease flare.
Similar content being viewed by others
Introduction
Serious infections (SIs) in patients with rheumatoid arthritis (RA) are a major concern with risk of increased overall mortality. The immunological dysfunction of the disease itself, concomitant illnesses, and/or immunosuppressive medicines may all contribute to the higher risk of SIs in RA [1, 2].
The coronavirus disease 2019 (COVID-19) pandemic, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was one of the greatest threats to public health in the century [3]. The amount of research invested in COVID-19 was huge, and effective vaccines and potential therapeutic agents were discovered [4, 5]. Despite that, until January 2023 COVID-19 was still declared a “Public Health Emergency of International Concern (PHEIC)” [6]. The end of the global emergency was declared in May 2023, but the health community was instructed to remain vigilant [7]. Typically, the virus causes a mild to moderate respiratory illness. However, it occasionally leads to severe alveolar disease that can substantially lead to respiratory failure [8].
The similarities in the cytokine profile, patterns of immune activation, and some common therapeutic strategies suggest an intricate relationship between COVID-19 and RA [9, 10]. Evidence revealed an increased risk of COVID-19 generally and serious outcomes specifically in RA patients [11]. On the other hand, infections are among the environmental factors that can trigger RA [12]. There are numerous cases reported concerning the development of RA following COVID-19 infection [13]. In patients with pre-existing RA, infection can induce flares [14].
The pandemic should not pass without lessons. The data available regarding the co-existence of both diseases can be further invested to elucidate the bidirectional relationship between infections and RA. The current study aimed to identify the factors associated with severe COVID-19 infection in RA patients. The risk of flares in patients following infection was considered a secondary objective.
Patients and methods
This study is a case control study in which RA patients, diagnosed according to 2010 American College of Rheumatology/ European League Against Rheumatism (ACR/EULAR) classification criteria [15], infected with COVID-19 were recruited. Infection was proven by either positive COVID-19 polymerase chain reaction (PCR), SARS-CoV-2 immunoglobulins IgM/IgG or typical computed tomography (CT) chest findings with classic symptoms and signs [16]. Patients were recruited from Rheumatology and Rehabilitation Department, Faculty of medicine, Cairo University hospitals and private rheumatology centers. After analysis of records and personally contacting 1864 patients; 200 patients had a proven COVID-19 infection. They were infected from the start of pandemic in 2019 till 30 June 2022. Patients were informed about the objective of the study and oral consent was obtained for the use of medical data.
Grading of severity of COVID-19 infection was done according to the WHO disease severity grading [16]. Patients who had severe/critical COVID-19 were compared to those with mild/moderate COVID-19 to determine factors associated with severe infection. Comparison was done in terms of general characteristics including age, gender, comorbidities, history of previous serious infections defined as infections that required hospitalization and/or intravenous antibiotics, COVID-19 vaccination prior to infection, as well as RA-related disease factors including disease duration, seropositivity, presence of extra-articular manifestation, disease activity grading prior to infection measured using the Clinical Disease Activity index (CDAI) [17, 18], and medications used to treat RA. Factors that turned out to be significantly different between both groups were subjected to multivariate analysis.
Disease activity grading using CDAI within 6 months prior to COVID-19 infection and within 6 months following infection was obtained from patients’ records and a comparison between both readings was used to calculate the incidence of RA flare. Asai and colleagues defined flare as a CDAI score > 10 [19]. It is also the cut-off for moderate disease activity in the originator score [18]. More than 50% of our cohort had moderate/ high disease activity at baseline and hence increase of CDAI score > 10 points rather than the absolute value was considered flare.
Statistical analysis
Data were coded and entered using the statistical package for the Social Sciences (SPSS) version 26 (IBM Corp., Armonk, NY, USA). Data were summarized using mean, standard deviation, median, minimum, maximum and interquartile range in quantitative data and using frequency (count), and relative frequency (percentage) for categorical data. Comparisons between quantitative variables were done using the non-parametric Kruskal–Wallis and Mann–Whitney tests. For comparing categorical data, Chi square (χ2) test was performed. Exact test was used instead when the expected frequency is less than 5. Multivariate logistic regressions were done to determine the risk factors associated with the occurrence of severe, critical COVID-19 infection. P values less than 0.05 were considered statistically significant.
Results
The demographic data, baseline clinical characteristics, and treatment received by the studied patients are shown in Table 1. The majority of patients were females (93.5%) and their mean age was 48.92 ± 12.1 years. The most common symptoms of COVID-19 infection were myalgia and bone aches, followed by fatigue and sore throat in 74%, 57.5%, and 55.5% of patients, respectively. Most patients had mild COVID-19, while 36 (18%) patients had severe/critical COVID-19 (Table 2).
A comparison between patients with mild/moderate COVID-19 (n = 164) and those with severe/critical COVID-19 (n = 36) was done and is demonstrated in Table 3. Factors that were significantly different between both groups in the univariate analysis were subjected to multivariate analysis as demonstrated in Table 4. History of previous serious infection, age > 60 years, and diabetes had a positive association, whereas COVID-19 vaccination was negatively associated with severe/critical COVID-19 infection. Patients with severe/critical COVID-19 had a significantly higher CDAI prior to infection when compared with those with mild/moderate COVID-19. However, after adjustment of confounding factors CDAI prior to COVID-19 was no longer significant.
Following COVID-19 infection, the number of patients with high disease activity and the incidence of flares in the severe/critical COVID-19 group was significantly higher in comparison to patients with mild/moderate COVID (P < 0.001 and 0.003; respectively) (Table 5).
Discussion
COVID-19 was one of the largest pandemics faced by humans in the modern age [20]. There was a great concern about vulnerable groups including those with autoimmune disease [21]. The risk of COVID-19 in RA being one of the most common autoimmune rheumatic diseases was extensively studied [11]. In a study including 33,886 people with RA in the US Veterans Affairs system, the risk of COVID-19 diagnosis was 25% higher than in 33,886 people without RA [22].
Whether RA is associated with an increased risk of COVID-19 infection is beyond the scale of the current study. The study, however, was conducted to determine the factors associated with severe infection. Several studies conducted on RA patients showed increased risk of hospitalization, poor outcome, and death when compared to the general population [22,23,24]. However, after adjustment for demographic data and comorbidities the risk declined [25] or was even lost [26] in some studies.
In the current study older age, particularly age > 60 years was among the strongest predictors of severe infection (OR 6.13, 95% CI 2.12–17.72). Among the studied comorbidities, diabetes was also identified as a strong predictor (OR 4.54, 95% CI 1.07–19.32). Both factors were associated with poor outcome in a substantial number of studies conducted on the general population. In a meta-analysis that included 109 articles and 20,296 participants, both increasing age (RR 1.45, 95% CI 1.23–1.71) and diabetes (RR 1.59, 95% CI 1.41–1.78) were associated with higher risk of mortality. Every ten-year increase in the mean age of patients was associated with a 7.6% increase in the mortality and 11.2% increase in disease severity [27]. In a retrospective study conducted on 2724 Egyptian COVID-19 patients, of whom 423 (15.52%) were critically ill, age > 60 years (OR 1.30, 95% CI 1.05–1.61, P = 0.014), diabetes (OR 1.62, 95% CI 1.26–2.08, P < 0.001) were among the predictors of critical illness [28]. In the COVID-19 Global Rheumatology Alliance (C19-GRA) registry which included 3,729 patients with rheumatic disease, the risk of death was associated with age (66–75 years: OR 3.00, 95% CI 2.13–4.22; > 75 years: 6.18, 4.47–8.53; both vs ≤ 65 years) [29].
In COVID-19, age seems to be the most important determinant of infection risk possibly reflecting age-related reduction in expression of angiotensin-converting enzyme 2 (ACE-2) receptor, a cellular receptor for SARS- CoV-2 binding [30] age-dependent difficulty in removing particles from small airways [31], excessive release of inflammatory mediators in elderly “inflammaging” [32], incompetent immune response, and high frequency of comorbidities in the elderly population [33]. Several mechanisms render diabetics more prone to infections, particularly COVID-19 infection including defective chemotaxis, macrophage, and phagocytic activity and reduced secretion of cytokines. Poor glycemic control facilitates viral replication and hypoglycemic drugs were implicated in facilitating the entry of SARS-CoV-2 into cells and increased expression of ACE-2 receptor [34].
COVID-19 vaccination offered protection against severe/critical infection in the current study (OR 0.06, 95% CI 0.005–0.73). Most patients with rheumatic disease generate antibody responses after vaccination, although lower antibody titers might be produced than in the wider population [35, 36]. It should be noted, however, that the current study included patients infected with different strains of COVID-19 that could have contributed to variable degrees of severity. SARS-CoV-2 strains that circulated when COVID-19 vaccines became available were associated with decreased mortality in comparison to preceding waves [37].
The effect of RA-related disease activity on the severity of infection was of particular concern in the current study. The potential effect of disease activity found in univariate analysis was lost after adjustment for confounders. The limited insurance coverage in our country results in frequent use of steroids as demonstrated in the current study. Mean prednisolone dose was significantly higher and the use of prednisolone > 5 mg was more frequent in patients with severe/critical COVID-19; the difference was also lost after adjustment for confounders. Patients with a more aggressive disease receive more aggressive immunosuppressants including steroids, and hence, confounding by indication has always been a challenge faced when this particular issue was addressed. Several studies found an association between higher disease activity levels and risk of infection including COVID-19 infection in RA patients [2, 29, 38,39,40]. Strangfeld and colleagues could not find a direct association between higher disease activity and infection risk; the effect, however, was indirect due to steroid use and decline in function [41].
History of previous infection was identified as another predictor of severe COVID-19 (OR 5.88, 95% CI, 2.13–16.22). In a previous study analyzing the risk of serious infections in patients with musculoskeletal disorders, history of prior serious infections was associated with increased risk of subsequent infection [2]. Concomitant bacterial infections were frequently observed in patients with COVID-19 [42] particularly in older patients and those with chronic medical diseases [43], suggesting common pathophysiological mechanisms.
The relationship between COVID-19 and RA is bidirectional, and hence, the effect of COVID-19 on RA disease activity was also investigated in the current study. The hyperstimulation and dysregulation of the immune system in severe COVID-19 was implicated in substantially higher risk of development of autoimmune diseases including RA according to a recent study [44, 45] and might hence result in disease flare in patients who already have these conditions. The current study showed evidence of higher disease activity levels, particularly in patients with severe/critical infection. The fear of utilization of RA treatment during the pandemic and interruption of treatment in patients who developed COVID-19 infection are additional contributing factors.
The current study has the strength of being one of the few studies of its type conducted in the region. However, it has some limitations. The retrospective nature of the study can lead to recall bias. All patients or their relatives were personally contacted, and hence, mortality was underestimated. Additionally, some factors such as different strains of COVID-19 and different types of vaccination received by patients contributed to disease severity.
Data avilability
The data that support the findings of this study are available on request from the corresponding author.
References
Listing J, Gerhold K, Zink A. The risk of infections associated with rheumatoid arthritis, with its comorbidity and treatment. Rheumatology (Oxford). 2013;52:53–61. https://doi.org/10.1093/rheumatology/kes305.
Mehta B, Pedro S, Ozen G, Kalil A, Wolfe F, Mikuls T, Michaud K. Serious infection risk in rheumatoid arthritis compared with non-inflammatory rheumatic and musculoskeletal diseases: a US national cohort study. RMD Open. 2019;5: e000935. https://doi.org/10.1136/rmdopen-2019-000935.
Chakraborty I, Maity P. COVID-19 outbreak: migration, effects on society, global environment and prevention. Sci Total Environ. 2020;728: 138882. https://doi.org/10.1016/j.scitotenv.2020.138882.
Sharma A, Ahmad Farouk I, Lal SK. COVID-19: a review on the novel coronavirus disease evolution, transmission, detection, control and prevention. Viruses. 2021;13:202. https://doi.org/10.3390/v13020202.
Ssentongo P, Ssentongo AE, Voleti N, Groff D, Sun A, Ba DM, Nunez J, Parent LJ, Chinchilli VM, Paules CI. SARS-CoV-2 vaccine effectiveness against infection, symptomatic and severe COVID-19: a systematic review and meta-analysis. BMC Infect Dis. 2022;22:439. https://doi.org/10.1186/s12879-022-07418-y.
Statement on the fourteenth meeting of the International Health Regulations. Emergency Committee on the coronavirus disease (COVID-19) pandemic. In: World health Organization, 2005. https://www.who.int/news/item/30-01-2023-statement-on-the-fourteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic. Accessed 15 Jul 2023.
Statement on the fifteenth meeting of the IHR. Emergency Committee on the COVID-19 pandemic. In: World health Organization, 2005. https://www.who.int/news/item/05-05-2023-statement-on-the-fifteenth-meeting-of-the-international-health-regulations-(2005)-emergency-committee-regarding-the-coronavirus-disease-(covid-19)-pandemic. Accessed 15 Aug 2023.
Zeng H, Ma Y, Zhou Z, Liu W, Huang P, Jiang M, Liu Q, Chen P, Luo H, Chen Y. Spectrum and clinical characteristics of symptomatic and asymptomatic coronavirus disease 2019 (COVID-19) with and without pneumonia. Front Med (Lausanne). 2021;8: 645651. https://doi.org/10.3389/fmed.2021.645651.
Dewanjee S, Kandimalla R, Kalra RS, Valupadas C, Vallamkondu J, Kolli V, Dey Ray S, Reddy AP, Reddy PH. COVID-19 and rheumatoid arthritis crosstalk: emerging association, therapeutic options and challenges. Cells. 2021;10:3291. https://doi.org/10.3390/cells10123291.
Tripathy A, Swain N, Gupta B. The COVID-19 pandemic: an increased risk of rheumatoid arthritis. Future Virol. 2021. https://doi.org/10.2217/fvl-2020-0393.
Zaccardelli A, Wallace ZS, Sparks JA. Acute and postacute COVID-19 outcomes for patients with rheumatoid arthritis: lessons learned and emerging directions 3 years into the pandemic. Curr Opin Rheumatol. 2023;35:175–84. https://doi.org/10.1097/BOR.0000000000000930.
Joo YB, Lim YH, Kim KJ, Park KS, Park YJ. Respiratory viral infections and the risk of rheumatoid arthritis. Arthritis Res Ther. 2019;21:199. https://doi.org/10.1186/s13075-019-1977-9.
Slouma M, Mhemli T, Abbes M, Triki W, Dhahri R, Metoui L, Gharsallah I, Louzir B. Rheumatoid arthritis occurring after coronavirus disease 2019 (COVID-19) infection: case based review. Egypt Rheumatol. 2022;44:275–8. https://doi.org/10.1016/j.ejr.2022.03.001.
Perrot L, Hemon M, Busnel JM, Muis-Pistor O, Picard C, Zandotti C, Pham T, Roudier J, Desplat-Jego S, Balandraud N. First flare of ACPA-positive rheumatoid arthritis after SARS-CoV-2 infection. Lancet Rheumatol. 2021;3:e6–8. https://doi.org/10.1016/S2665-9913(20)30396-9.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO 3rd, Birnbaum NS, Burmester GR, Bykerk VP, Cohen MD, Combe B, Costenbader KH, Dougados M, Emery P, Ferraccioli G, Hazes JM, Hobbs K, Huizinga TW, Kavanaugh A, Kay J, Kvien TK, Laing T, Mease P, Ménard HA, Moreland LW, Naden RL, Pincus T, Smolen JS, Stanislawska-Biernat E, Symmons D, Tak PP, Upchurch KS, Vencovský J, Wolfe F, Hawker G. 2010 Rheumatoid arthritis classification criteria: an American college of rheumatology/European league against rheumatism collaborative initiative. Arthritis Rheum. 2010;62:2569–81. https://doi.org/10.1002/art.27584.
Clinical management of COVID-19, Interim Guidance. In: World Health Organization. https://www.who.int/publications/i/item/clinical-management-of-covid-19. Accessed 8 Jun 2020.
Aletaha D, Nell VP, Stamm T, Uffmann M, Pflugbeil S, Machold K, Smolen JS. Acute phase reactants add little to composite disease activity indices for rheumatoid arthritis: validation of a clinical activity score. Arthritis Res Ther. 2005;7:R796-806. https://doi.org/10.1186/ar1740.
Aletaha D, Smolen J. The simplified disease activity index (SDAI) and the clinical disease activity index (CDAI): a review of their usefulness and validity in rheumatoid arthritis. Clin Exp Rheumatol. 2005;23(Suppl 39):S100–8.
Asai S, Takahashi N, Hayashi M, Hanabayashi M, Kanayama Y, Takemoto T, Yabe Y, Shioura T, Ishikawa H, Yoshioka Y, Kato T, Hirano Y, Fujibayashi T, Hattori Y, Kobayakawa T, Ando M, Kuwatsuka Y, Matsumoto T, Asai N, Sobue Y, Nishiume T, Suzuki M, Ishiguro N, Kojima T. Predictors of disease flare after discontinuation of concomitant methotrexate in Japanese patients with rheumatoid arthritis treated with tocilizumab. Jt Bone Spine. 2020;87:596–602. https://doi.org/10.1016/j.jbspin.2020.06.001.
Feehan J, Apostolopoulos V. Is COVID-19 the worst pandemic? Maturitas. 2021;149:56–8. https://doi.org/10.1016/j.maturitas.2021.02.001.
Grainger R, Kim AHJ, Conway R, Yazdany J, Robinson PC. COVID-19 in people with rheumatic diseases: risks, outcomes, treatment considerations. Nat Rev Rheumatol. 2022;18:191–204. https://doi.org/10.1038/s41584-022-00755-x.
England BR, Roul P, Yang Y, Kalil AC, Michaud K, Thiele GM, Sauer BC, Baker JF, Mikuls TR. Risk of COVID-19 in rheumatoid arthritis: a national veterans affairs matched cohort study in at-risk individuals. Arthritis Rheumatol. 2021;73:2179–88. https://doi.org/10.1002/art.41800.
Topless RK, Phipps-Green A, Leask M, Dalbeth N, Stamp LK, Robinson PC, Merriman TR. Gout, Rheumatoid arthritis, and the risk of death related to coronavirus disease 2019: an analysis of the UK Biobank. ACR Open Rheumatol. 2021;3:333–40. https://doi.org/10.1002/acr2.11252.
Cordtz R, Lindhardsen J, Soussi BG, Vela J, Uhrenholt L, Westermann R, Kristensen S, Nielsen H, Torp-Pedersen C, Dreyer L. Incidence and severeness of COVID-19 hospitalization in patients with inflammatory rheumatic disease: a nationwide cohort study from Denmark. Rheumatology (Oxford). 2021;60:SI59–67. https://doi.org/10.1093/rheumatology/keaa897.
Shin YH, Shin JI, Moon SY, Jin HY, Kim SY, Yang JM, Cho SH, Kim S, Lee M, Park Y, Kim MS, Won HH, Hong SH, Kronbichler A, Koyanagi A, Jacob L, Smith L, Lee KH, Suh DI, Lee SW, Yon DK. Autoimmune inflammatory rheumatic diseases and COVID-19 outcomes in South Korea: a nationwide cohort study. Lancet Rheumatol. 2021;3:e698–706. https://doi.org/10.1016/S2665-9913(21)00151-X.
Reilev M, Kristensen KB, Pottegård A, Lund LC, Hallas J, Ernst MT, Christiansen CF, Sørensen HT, Johansen NB, Brun NC, Voldstedlund M, Støvring H, Thomsen MK, Christensen S, Gubbels S, Krause TG, Mølbak K, Thomsen RW. Characteristics and predictors of hospitalization and death in the first 11,122 cases with a positive RT-PCR test for SARS-CoV-2 in Denmark: a nationwide cohort. Int J Epidemiol. 2020;49:1468–81. https://doi.org/10.1093/ije/dyaa140.
Chidambaram V, Tun NL, Haque WZ, Majella MG, Sivakumar RK, Kumar A, Hsu AT, Ishak IA, Nur AA, Ayeh SK, Salia EL, Zil-E-Ali A, Saeed MA, Sarena APB, Seth B, Ahmadzada M, Haque EF, Neupane P, Wang KH, Pu TM, Ali SMH, Arshad MA, Wang L, Baksh S, Karakousis PC, Galiatsatos P. Factors associated with disease severity and mortality among patients with COVID-19: a systematic review and meta-analysis. PLoS ONE. 2020;15: e0241541. https://doi.org/10.1371/journal.pone.0241541.
Omran D, Al Soda M, Bahbah E, Esmat G, Shousha H, Elgebaly A, Abdel Ghaffar M, Alsheikh M, El Sayed E, Afify S, Abdel Hafez S, Elkelany K, Eltayar A, Ali O, Kamal L, Heiba A. Predictors of severity and development of critical illness of Egyptian COVID-19 patients: a multicenter study. PLoS ONE. 2021;16: e0256203. https://doi.org/10.1371/journal.pone.0256203.
Strangfeld A, Schäfer M, Gianfrancesco MA, Lawson-Tovey S, Liew JW, Ljung L, Mateus EF, Richez C, Santos MJ, Schmajuk G, Scirè CA, Sirotich E, Sparks JA, Sufka P, Thomas T, Trupin L, Wallace ZS, Al-Adely S, Bachiller-Corral J, Bhana S, Cacoub P, Carmona L, Costello R, Costello W, Gossec L, Grainger R, Hachulla E, Hasseli R, Hausmann JS, Hyrich KL, Izadi Z, Jacobsohn L, Katz P, Kearsley-Fleet L, Robinson PC, Yazdany J, Machado PM, COVID-19 Global Rheumatology Alliance. Factors associated with COVID-19-related death in people with rheumatic diseases: results from the COVID-19 global rheumatology alliance physician-reported registry. Ann Rheum Dis. 2021;80:930–42. https://doi.org/10.1136/annrheumdis-2020-219498.
Bunyavanich S, Do A, Vicencio A. Nasal gene expression of angiotensin-converting enzyme 2 in children and adults. JAMA. 2020;323:2427–9. https://doi.org/10.1001/jama.2020.8707.
Svartengren M, Falk R, Philipson K. Long-term clearance from small airways decreases with age. Eur Respir J. 2005;26:609–15. https://doi.org/10.1183/09031936.05.00002105.
Zazzara MB, Bellieni A, Calvani R, Coelho-Junior HJ, Picca A, Marzetti E. Inflammaging at the time of COVID-19. Clin Geriatr Med. 2022;38:473–81. https://doi.org/10.1016/j.cger.2022.03.003.
Perrotta F, Corbi G, Mazzeo G, Boccia M, Aronne L, D’Agnano V, Komici K, Mazzarella G, Parrella R, Bianco A. COVID-19 and the elderly: insights into pathogenesis and clinical decision-making. Aging Clin Exp Res. 2020;32:1599–608. https://doi.org/10.1007/s40520-020-01631-y. (Erratum in: Aging Clin Exp Res 2020; 32(9):1909).
Gęca T, Wojtowicz K, Guzik P, Góra T. Increased risk of COVID-19 in patients with diabetes mellitus-current challenges in pathophysiology, treatment and prevention. Int J Environ Res Public Health. 2022;19:6555. https://doi.org/10.3390/ijerph19116555.
Simon D, Tascilar K, Fagni F, Krönke G, Kleyer A, Meder C, Atreya R, Leppkes M, Kremer AE, Ramming A, Pachowsky ML, Schuch F, Ronneberger M, Kleinert S, Hueber AJ, Manger K, Manger B, Berking C, Sticherling M, Neurath MF, Schett G. SARS-CoV-2 vaccination responses in untreated, conventionally treated and anticytokine-treated patients with immune-mediated inflammatory diseases. Ann Rheum Dis. 2021;80:1312–6. https://doi.org/10.1136/annrheumdis-2021-220461.
Boekel L, Steenhuis M, Hooijberg F, Besten YR, van Kempen ZLE, Kummer LY, van Dam KPJ, Stalman EW, Vogelzang EH, Cristianawati O, Keijzer S, Vidarsson G, Voskuyl AE, Wieske L, Eftimov F, van Vollenhoven R, Kuijpers TW, van Ham SM, Tas SW, Killestein J, Boers M, Nurmohamed MT, Rispens T, Wolbink G. Antibody development after COVID-19 vaccination in patients with autoimmune diseases in the Netherlands: a substudy of data from two prospective cohort studies. Lancet Rheumatol. 2021;3:e778–88. https://doi.org/10.1016/S2665-9913(21)00222-8.
Amin R, Sohrabi MR, Zali AR, Hannani K. Five consecutive epidemiological waves of COVID-19: a population-based cross-sectional study on characteristics, policies, and health outcome. BMC Infect Dis. 2022;22:906. https://doi.org/10.1186/s12879-022-07909-y.
Yun H, Chen L, Roy JA, Greenberg J, Harrold LR, George MD, Curtis JR. Rheumatoid arthritis disease activity and hospitalized infection in a large US registry. Arthritis Care Res (Hoboken). 2023;75:1639–47. https://doi.org/10.1002/acr.24984.
Au K, Reed G, Curtis JR, Kremer JM, Greenberg JD, Strand V, Furst DE, CORRONA Investigators. High disease activity is associated with an increased risk of infection in patients with rheumatoid arthritis. Ann Rheum Dis. 2011;70:785–91. https://doi.org/10.1136/ard.2010.128637.
Emery P, Gallo G, Boyd H, Morgan CL, Currie CJ, Poole CD, Nab HW. Association between disease activity and risk of serious infections in subjects with rheumatoid arthritis treated with etanercept or disease-modifying anti-rheumatic drugs. Clin Exp Rheumatol. 2014;32:653–60.
Strangfeld A, Eveslage M, Schneider M, Bergerhausen HJ, Klopsch T, Zink A, Listing J. Treatment benefit or survival of the fittest: what drives the time-dependent decrease in serious infection rates under TNF inhibition and what does this imply for the individual patient? Ann Rheum Dis. 2011;70:1914–20. https://doi.org/10.1136/ard.2011.151043.
Musuuza JS, Watson L, Parmasad V, Putman-Buehler N, Christensen L, Safdar N. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and meta-analysis. PLoS ONE. 2021;16: e0251170. https://doi.org/10.1371/journal.pone.0251170.
Garcia-Vidal C, Sanjuan G, Moreno-García E, Puerta-Alcalde P, Garcia-Pouton N, Chumbita M, Fernandez-Pittol M, Pitart C, Inciarte A, Bodro M, Morata L, Ambrosioni J, Grafia I, Meira F, Macaya I, Cardozo C, Casals C, Tellez A, Castro P, Marco F, García F, Mensa J, Martínez JA, Soriano A, COVID-19 Researchers Group. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin Microbiol Infect. 2021;27:83–8. https://doi.org/10.1016/j.cmi.2020.07.041.
Chang R, Yen-Ting Chen T, Wang SI, Hung YM, Chen HY, Wei CJ. Risk of autoimmune diseases in patients with COVID-19: a retrospective cohort study. EClinicalMedicine. 2023;56: 101783. https://doi.org/10.1016/j.eclinm.2022.101783.
Sharma C, Bayry J. High risk of autoimmune diseases after COVID-19. Nat Rev Rheumatol. 2023;19:399–400. https://doi.org/10.1038/s41584-023-00964-y.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
AE, LAM, HMA and KTEH structured the study plan and the research design. AE performed the field work of the study. AE, LAM provided data analysis and interpretation of the results. AE and LAM conducted the statistical analysis. LAM wrote the main manuscript draft and prepared the tables and figures. HMA and KTEH critically reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The Research Ethics Committee, Faculty of Medicine, Cairo University has approved this study with approval number (MD-386- 2021). This study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Consent to participate
Informed consent was obtained from all the study participants.
Patient consent
Patient’s consent was obtained from all participants.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Embaby, A., Maged, L.A., Abdel-Hamid, H.M. et al. Factors associated with severe infection in rheumatoid arthritis patients: lessons learned from the COVID-19 pandemic. Infection (2024). https://doi.org/10.1007/s15010-024-02187-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02187-z