Abstract
Purpose
To determine characteristics associated with inappropriate antibiotic use amongst children hospitalised for influenza.
Methods
We performed active surveillance for laboratory-confirmed influenza hospitalizations amongst children ≤ 16 years old at the 12 Canadian Immunization Monitoring Program Active hospitals, from September 2010 to August 2021. Antibiotic use was presumed appropriate if any of the following indications were met: age < 1 month, immunocompromised, hemoglobinopathy, laboratory-confirmed bacterial infection, radiographically confirmed pneumonia, admission to an intensive care unit and mechanical ventilation. Regression analyses were used to identify baseline and clinical characteristics associated with antibiotic use amongst patients without an appropriate indication.
Results
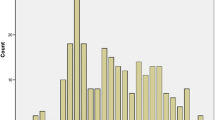
Amongst 8971 children, 6424 (71.6%) received any antibiotics during their hospitalisation. Amongst the 4429 children without an appropriate indication, 2366 (53.2%) received antibiotics. Antibiotic use amongst children without appropriate indication differed between study centres, ranging from 33.2% to 66.1% (interquartile range [IQR] 50.6–56.3%); it did not change significantly over time (p-value for trend = 0.28). In multivariable analyses, older age (adjusted odds ratio [aOR] 0.97, 95% confidence interval [CI] 0.96–0.99), presence of any high-risk condition (aOR 0.80, 95% CI 0.70–0.92), influenza virus type B (aOR 0.8, 95% CI 0.70–0.91) and croup (aOR 0.64, 95% CI 0.49–0.83) were associated with less, whilst fever ≥ 38.5 °C (aOR 1.82, 95% CI 1.42–2.35) and hospitalisation duration (aOR 1.12, 95% CI 1.09–1.15) were associated with more inappropriate antibiotic use.
Conclusions
Over two-third of children hospitalised for influenza received antibiotics, including over half of those without an appropriate indication for antibiotic treatment. Differences amongst study centres suggest the importance of contextual determinants of antibiotic use.



Similar content being viewed by others
Data availability
Data not available. Te data are owned by the Public Health Agency of Canada.
References
Barlam TF, Cosgrove SE, Abbo LM, et al. Implementing an antibiotic stewardship program: guidelines by the Infectious Diseases Society of America and the Society for Healthcare Epidemiology of America. Clin Infect Dis. 2016;62:e51-77.
Uyeki TM, Bernstein HH, Bradley JS, et al. Clinical practice guidelines by the Infectious Diseases Society of America: 2018 update on diagnosis, treatment, chemoprophylaxis, and institutional outbreak management of seasonal influenzaa. Clin Infect Dis. 2019;68:e1–47.
World Health Organization. Guidelines for the clinical management of severe illness from influenza virus infections. World Health Organization; 2022.
Morris DE, Cleary DW, Clarke SC. Secondary bacterial infections associated with influenza pandemics. Front Microbiol. 2017;8:1041.
Teutsch SM, Zurynski YA, Nunez C, et al. Ten years of national seasonal surveillance for severe complications of influenza in Australian children. Pediatr Infect Dis J. 2021;40:191–8.
Papan C, Willersinn M, Weiss C, Karremann M, Schroten H, Tenenbaum T. Antibiotic utilization in hospitalized children under 2 years of age with influenza or respiratory syncytial virus infection—a comparative, retrospective analysis. BMC Infect Dis. 2020;20:606.
Peltola V, Ziegler T, Ruuskanen O. Influenza A and B virus infections in children. Clin Infect Dis. 2003;36:299–305.
Goriacko P, Saiman L, Zachariah P. Antibiotic use in hospitalized children with respiratory viruses detected by multiplex polymerase chain reaction. Pediatr Infect Dis J. 2018;37:443–6.
Avila-Morales S, Ospina-Henao S, Ulloa-Gutierrez R, Avila-Aguero ML. Epidemiological and clinical profile between influenza A and B virus in Costa Rican children. Int J Infect Dis. 2021;105:763–8.
Ghazaryan H, Babloyan A, Sarkissian A, Davtyan K, Berger C. Respiratory syncytial and influenza virus detecting rapid tests in children younger than 5 years of age in Armenia. J Infect Dev Ctries. 2019;13:75S-80S.
Walsh PS, Schnadower D, Zhang Y, Ramgopal S, Shah SS, Wilson PM. Assessment of temporal patterns and patient factors associated with oseltamivir administration in children hospitalized with influenza, 2007–2020. JAMA Netw Open. 2022;5: e2233027.
Wilkes JJ, Leckerman KH, Coffin SE, et al. Use of antibiotics in children hospitalized with community-acquired, laboratory-confirmed influenza. J Pediatr. 2009;154:447–9.
Canadian Pediatic Society. https://www.cps.ca/en/impact. Accessed 15 July 2022.
Mehta K, Morris SK, Bettinger JA, et al. Antiviral use in Canadian children hospitalized for influenza. Pediatrics. 2021;148:e2020049672
Groves HE, Papenburg J, Mehta K, et al. The effect of the COVID-19 pandemic on influenza-related hospitalization, intensive care admission and mortality in children in Canada: a population-based study. Lancet Reg Health Am. 2022;7: 100132.
Bettinger JA, Halperin SA, Vaudry W, Law BJ, Scheifele DW, Canadian Im. The Canadian Immunization Monitoring Program, ACTive (IMPACT): active surveillance for vaccine adverse events and vaccine-preventable diseases. Can Commun Dis Rep. 2014;40:41–4.
Sinilaite A, Papenburg J. Summary of the National Advisory Committee on Immunization (NACI) Seasonal Influenza Vaccine Statement for 2022–2023. Can Commun Dis Rep. 2022;48:373–82.
Public Health Agency of Canada. FluWatch. https://publications.gc.ca/site/eng/9.507424/publication.html. Accessed 13 Oct 2023.
Pantell RH, Roberts KB, Adams WG, et al. Evaluation and management of well-appearing febrile infants 8 to 60 days old. Pediatrics. 2021;148:e2021052228
Fatimah SRS. Chapter 229 Influenza viruses. In: Long SPC, Fischer M, Kimberlin D, editors. Principles and practice of pediatric infectious diseases. 6th ed. Elsevier; 2023. p. 1205–13.
Shah SC, Rumoro DP, Hallock MM, et al. Clinical predictors for laboratory-confirmed influenza infections: exploring case definitions for influenza-like illness. Infect Control Hosp Epidemiol. 2015;36:241–8.
Blumental S, Huisman E, Cornet MC, et al. Pandemic A/H1N1v influenza 2009 in hospitalized children: a multicenter Belgian survey. BMC Infect Dis. 2011;11:313.
Hernandez-Bou S, Novell CB, Alins JG, Garcia-Garcia JJ, Infectious Diseases Working Group SSoPE. Hospitalized children with influenza A H1N1 (2009) infection: a Spanish multicenter study. Pediatr Emerg Care. 2013;29:49–52.
Klein EY, Monteforte B, Gupta A, et al. The frequency of influenza and bacterial coinfection: a systematic review and meta-analysis. Influenza Other Respir Viruses. 2016;10:394–403.
Centers for Disease Control, Prevention. Office-related antibiotic prescribing for persons aged, 1993-1994 to 2007-2008. MMWR Morb Mortal Wkly Rep. 2011;60:1153–6.
Pichichero ME. Dynamics of antibiotic prescribing for children. JAMA. 2002;287:3133–5.
European Centre for Disease Prevention and Control. Antimicrobial consumption in the EU/EEA (ESAC-Net) - Annual Epidemiological Report 2021. Stockholm: ECDC; 2022.
Gerber JS, Newland JG, Coffin SE, et al. Variability in antibiotic use at children’s hospitals. Pediatrics. 2010;126:1067–73.
Skajaa N, Gehrt L, Nieminen H, et al. Trends in Antibiotic Use in Danish, Finnish, Norwegian and Swedish Children. Clin Epidemiol. 2022;14:937–47.
Public Health Agency of Canada. Canadian Antimicrobial Resistance Surveillance System Report. 2020. https://www.canada.ca/content/dam/hc-sc/documents/services/drugs-health-products/canadian-antimicrobial-resistance-surveillance-system-2020-report/CARSS-2020-report-2020-eng.pdf. Accessed 15 July 2022.
Public Health Agency of Canada. Evidence synthesis summary: social and cultural drivers of antimicrobial use. 2019.
Noel KC, Papenburg J, Lacroix J, et al. International Survey on Determinants of Antibiotic Duration and Discontinuation in Pediatric Critically Ill Patients. Pediatr Crit Care Med. 2020;21:e696–706.
Cherry JD. Clinical practice. Croup N Engl J Med. 2008;358:384–91.
Adams K, Tenforde MW, Chodisetty S, et al. A literature review of severity scores for adults with influenza or community-acquired pneumonia - implications for influenza vaccines and therapeutics. Hum Vaccin Immunother. 2021;17:5460–74.
Burstein B, Plint AC, Papenburg J. Use of Radiography in Patients Diagnosed as Having Acute Bronchiolitis in US Emergency Departments, 2007–2015. JAMA. 2018;320:1598–600.
Papenburg J, Fontela PS, Freitas RR, Burstein B. Inappropriate antibiotic prescribing for acute bronchiolitis in US Emergency Departments, 2007–2015. J Pediatric Infect Dis Soc. 2019;8:567–70.
Acknowledgements
IMPACT Investigators on this project: Cheryl Foo, Natalie Bridger, Janeway Children’s Health & Rehabilitation Centre, St. John’s, NL; Scott A. Halperin, Karina Top, IWK Health Centre, Halifax, NS; Roseline Thibeault, Centre Mere-Enfant de Quebec, CHUL, Quebec City, QC; Jesse Papenburg, The Montreal Children’s Hospital, Montreal, QC; Marc Lebel, Centre hospitalier universitaire Sainte-Justine, Montreal, QC; Nicole Le Saux, Children’s Hospital of Eastern Ontario, Ottawa, ON; Shaun K. Morris, Kescha Kazmi, The Hospital for Sick Children, Toronto, ON; Jared Bullard, Winnipeg Children’s Hospital, Winnipeg, MB; Rupeena Purewal, Jim Pattison Children’s Hospital, Saskatoon, SK; Taj Jadavji, Alberta Children’s Hospital, Calgary, AB; Catherine Burton, Stollery Children’s Hospital, Edmonton, AB; Julie A. Bettinger, Laura Sauvé, Manish Sadarangani, BC Children’s Hospital, Vancouver, BC. We acknowledge all past IMPACT site investigators and influenza working group members involved in IMPACT at the time of data collection.
We acknowledge the IMPACT nurse monitors, Annick Audet (IMPACT Nurse Monitor Liaison), the staff of the IMPACT data centre, (Hennady Shulha, Suzanne Liu, Kim Marty), and Melanie Laffin Thibodeau (Manager, Surveillance, Canadian Paediatric Society).
Funding
This surveillance activity is conducted as part of the Canadian Immunization Monitoring Program Active (IMPACT), a national surveillance initiative managed by the Canadian Pediatric Society (CPS) and conducted by the IMPACT network of paediatric investigators on behalf of the Public Health Agency of Canada’s (PHAC’s) Centre for Immunization and Respiratory Infectious Diseases. Funding for IMPACT influenza surveillance is provided by the PHAC. Dr. Sadarangani is supported via salary awards from the BC Children’s Hospital Foundation and Michael Smith Health Research BC. PHAC provided input into the study design.
Author information
Authors and Affiliations
Consortia
Contributions
TS, SKM and JP conceptualized the study; TS, JB and JM curated the data; TS and JM performed the analysis; TS and JP wrote the original draft of the manuscript; SKM, JB, CB, SAH, TJ, KK, MS contributed to study design and reviewed and revised the manuscript; the Canadian Immunization Monitoring Program Active (IMPACT) investigators performed the investigation providing data and reviewed the manuscript; JB, SAH and MS performed project administration and funding acquisition. JP supervised the study. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Papenburg reports grants from MedImmune, grants and personal fees from Merck, personal fees from AstraZeneca, all outside the submitted work. Dr. Sadarangani has been an investigator on projects funded by GlaxoSmithKline, Merck, Moderna, Pfizer, Sanofi-Pasteur, Seqirus, Symvivo and VBI Vaccines. All funds have been paid to his institute, and he has not received any personal payments. Dr. Halperin has been an investigator on projects funded by Sanofi-Pasteur, GlaxoSmithKline and Seqirus. Dr. Morris is a coinvestigator on an investigator-led grant from Pfizer, has served on an ad-hoc advisory boards for Pfizer, Sanofi Pasteur, and Merck and has received speaker fees from GlaxoSmithKline and JNJ China; all unrelated to this study. The other authors have no conflicts of interest to disclose.
Additional information
The members of the Canadian Immunization Monitoring Program Active (IMPACT) Investigators are mentioned in the Acknowledgments section.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schober, T., Morris, S.K., Bettinger, J.A. et al. Antibiotic use in children hospitalised for influenza, 2010–2021: the Canadian Immunization Monitoring Program Active (IMPACT). Infection (2023). https://doi.org/10.1007/s15010-023-02124-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-023-02124-6