Abstract
Purpose
Use of antibiotics can give rise to the selection of resistant bacteria. It remains unclear whether antibiotic use in primary care can influence bacterial resistance incidence in patients when hospitalised. The aim of this study is to explore the impact of prior community antibiotic usage on hospital-detected multidrug-resistant Gram-negative (MRGN) incidence rate.
Methods
This pharmacoepidemiological study was case–control in design, and was carried out in the Antrim Area Hospital (N. Ireland) in two phases. In phase 1, the controls were matched according to: age, gender, admission ward, date of admission, and age-adjusted Charlson co-morbidity index score. During the second phase, controls were selected randomly from the total population of admissions to the hospital over the 2-year study period.
Results
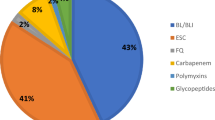
In phase 1, multivariate analysis revealed that prior exposure to the second- and third-generation cephalosporins (p = 0.004) and fluoroquinolones (p = 0.023) in primary care was associated with an increased likelihood of MRGN detection in inpatients. In phase 2, an independent relationship between an increased risk of identification of MRGN, while hospitalised was associated with: prolonged hospitalisation (p < 0.001), being elderly (p < 0.001), being female (p = 0.007), and having genitourinary disease (p < 0.001).
Conclusion
This study provides clear evidence which supports the need to optimise antibiotic use in primary care to help reduce MRGN incidence in hospitalised patients.

Similar content being viewed by others
References
Bush K. Past and present perspectives on β-lactamases. Antimicrob Agents Chemother. 2018. https://doi.org/10.1128/AAC.01076-18.
Russell-Goldman E, Burke L, Humphreys H, Gilleece A, Fitzgerald-Hughes D, O’ Neill E. Clinical features and molecular epidemiology of extended-spectrum B-lactamases-producing Enterobacteriaceae: the hidden messages. J Med Microbiol. 2013;62:1768–74.
Siedelman L, Kline L, Duval S. Risk factors for community- and health facility–acquired extended-spectrum β-lactamase–producing bacterial infections in patients at the University of Minnesota Medical Center, Fairview. Am J Infect Control. 2013;40:849–54.
Rogers BA. (on behalf of the Australasian Society for Infectious Diseases Clinical Research Network) Community-onset Escherichia coli infection resistant to expanded-spectrum cephalosporins in low-prevalence countries. Antimicrob Agents Chemother. 2014;58:2126–34.
Rodríguez-Baño J. Risk-factors for emerging bloodstream infections caused by extended-spectrum beta-lactamase-producing Escherichia coli. Clin Microbiol Infect. 2008;14:180–4.
Branger C, Ledda A, Billard-Pomares T, Doublet B, Fouteau S, Barbe V, Roche D, et al. Extended-spectrum β-lactamase-encoding genes are spreading on a wide range of Escherichia coli plasmids existing prior to the use of third-generation cephalosporins. Microb Genom. 2018;4:85. https://doi.org/10.1099/mgen.0.000203 (Epub Aug 2018).
Rodriguez-Bano J, Picon E, Gijon P, Hernandez JR, Ruiz M, Pena G, et al. Community-onset bacteraemia due to extended spectrum B-lactamase-producing E. coli: risk factors and prognosis. Clin Infect Dis. 2010;50:40–8.
Kritsotakis EI, Tsioutis C, Roumbelaki M, Christidou A, Gikas A. Antibiotic use and the risk of carbapenem-resistant extended-spectrum- lactamase-producing Klebsiella pneumoniae infection in hospitalized patients: results of a double case-control study. J Antimicrob Chemother. 2011;66:1383–8.
Oli AN, Eze DE, Gugu TH, Ezeobi I, Maduagwu UN, Ihekwereme CP. Multi-antibiotic resistant extended-spectrum beta-lactamase producing bacteria pose a challenge to the effective treatment of wound and skin infections. Pan Afr Med J. 2017;27:66.
Artero A, Esparcia A, Alberola J, Madrazo M, Nogueira JM, Eiros JM. Prospective cohort study of risk factors for extended-spectrum ß-lactamase-producing Escherichia coli urinary tract infections in elderly patients admitted to hospital. Int J Clin Pract. 2017;71:e13001 (Epub 5 Sep 2017).
Steiger SN, Comito RR, Nicolau DP. Clinical and economic implications of urinary tract infections. Expert Rev Pharmacoeconomics Outcomes Res. 2017;17:377–83.
Pitout JDD, Laupland KB. Extended-spectrum beta-lactamase-producing Enterobacteriaceae: an emerging public-health concern. Lancet Infect Dis. 2008;8:159–66.
Kang C, Wi YM, Ko KS, Chung DR, Peck KR, Lee NY, Song J. Outcomes and risk factors for mortality in community-onset bacteraemia caused by extended-spectrum beta-lactamase-producing Escherichia coli, with a special emphasis on antimicrobial therapy. Scand J Infect Dis. 2013;45:519–25.
Castillo-Tokumori F, Irey-Salgado C, Málaga G. Worrisome high frequency of extended-spectrum beta-lactamase-producing Escherichia coli in community-acquired urinary tract infections: a case-control study. Int J Infect Dis. 2017;55:16–9.
Cooper BS, Medley GF, Stone SP. Methicillin-resistant Staphylococcus aureus in hospitals and the community: stealth dynamics and control catastrophes. Proc Natl Acad Sci. 2004;101:10223–8.
Gallini A, Degris A, Desplas M, Bourrel R, Archambaud M, Montastruc JL, et al. Inlfluence of fluoroquinolone consumption in inpatients and outpatients on ciprofloxacin-resistant Escherichia coli in a university hospital. J Antimicrob Chemother. 2010;65:2650–8.
Lopez-Lozano JM, Monnet DL, Yague A, Burgos A, Gonzalo N, Campillos P, et al. Modelling and forecasting antimicrobial resistance and its dynamic relationship to antimicrobial use a time-series analysis. Int J Antimicrob Agents. 2000;14:21–31.
Aldeyab MA, Harbarth S, Vernaz N, Kearney MP, Scott MG, Darwish FW, et al. The impact of antibiotic use on the incidence and resistance pattern of extended-spectrum beta-lactamase-producing bacteria in primary and secondary healthcare settings. Br J Clin Pharmacol. 2012;74:171–9.
Exner M, Bhattacharya S, Christiansen B, Gebel J, Goroncy-Bermes P, Hartemann P, Heeg P, et al. Antibiotic resistance: what is so special about multidrug-resistant Gram-negative bacteria. GMS Hyg Infect Control. 2017;12:1–24.
Ramiarina RA, Ramiarina BL, Almeida RM. Pereira WCD Comorbidity adjustment index for the international classification of diseases, 10th revision. Revista de Saúde Pública. 2008;42:590–7.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic co-morbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–82.
Random Integer Generator. https://www.random.org/integers. Accessed Oct 2014.
European Committee on Antimicrobial Susceptibility Testing (EUCAST). Clinical breakpoints-bacteria. 2011. http://www.eucast.org. Accessed Oct 2014.
Doi Y, Park YS, Rivera JI, Adams-Haduch JM, Hingwe J, Sordillo EM, et al. Community-associated extended-spectrum beta-lactamase-producing E. coli infection in the United State. Clin Infect Dis. 2013;56:641–8.
Livermore DM. Declining cephalosporin and fluoroquinolone non-susceptibility among bloodstream Enterobacteriaceae from the UK: links to prescribing change? J Antimicrob Chemother. 2013;68:2667–8.
Karanika S, Karantanos T, Arvanitis M, Grigoras C, Mylonakis E. Fecal colonization with extended-spectrum beta-lactamase-producing enterobacteriaceae and risk factors among healthy individuals: a systematic review and metaanalysis. Clin Infect Dis. 2016;63:310–8.
A report from the PEW charitable trusts. Antibiotic use in outpatient settings. Health experts create national targets to reduce unnecessary antibiotic prescriptions. 2016. Accessed Jan 2019. https://www.pewtrusts.org//media/assets/2016/05/antibioticuseinoutpatientsettings.pdf.
Birgy A, Levy C, Bidet P, Thollot F, Derkx V, Béchet S, et al. ESBL-producing Escherichia coli ST131 versus non-ST131: evolution and risk factors of carriage among French children in the community between 2010 and 2015. J Antimicrob Chemother. 2016;71:2949–57.
D’Agata EM. Methodological issues of case-control studies: a review of established and newly recognised limitations. Infect Control Hosp Epidemiol. 2005;26:338–41.
MacDougall C, Powell J, Johnson C, Edmond M, Polk R. Hospital and community fluoroquinolone use and resistance in Staphylococcus aureus and Escherichia coli in 17 US hospitals. Clin Infect Dis. 2005;41:435–6.
Vernaz N, Huttner B, Muscionico D, Salomon JL, Bonnabry P, Lopez-Lozano JM, et al. Modelling the impact of antibiotic use on antibiotic-resistant Escherichia coli using population-bases data from a large hospital and its surrounding community. J Antimicrob Chemother. 2011;66:928–37.
Augustine MR, Testerman TL, Justo JA, Bookstaver PB, Kohn J, Albrecht H, et al. Clinical risk score for prediction of extended-spectrum β-lactamase-producing enterobacteriaceae in bloodstream isolates. Infect Control Hosp Epidemiol. 2017;38:266–7.
Crogan N, Evans BC. Clostridium difficile: an emerging epidemic in nursing homes. Geriatr Nurs. 2007;28:161–5.
Carroll KC, Bartlett JG. Biology of Clostridium difficile: implications for epidemiology and diagnosis. Ann Rev Microbiol. 2011;65:501–20.
Ishida T, Ito A, Washio Y, Yamazaki A, Noyama M, Tokioka F, et al. Risk factors for drug-resistant pathogens in immunocompetent patients with pneumonia: evaluation of PES pathogens. J Infect Chemother. 2017;23:23–6.
Wells BG, DiPiro JT, Schwinghammer TL, DiPiro CV. Pharmacotherapy handbook. 7th ed. Maidenheach: McGraw-Hill Medical; 2008. p. 544–55.
Pérez Heras I, Sanchez-Gomez JC, Beneyto-Martin P, Ruano-de-Pablo L, Losada-Pinedo B. Community-onset extended-spectrum β-lactamase producing Escherichia coli in urinary tract infections in children from 2015 to 2016: prevalence, risk factors, and resistances. Medicine (Baltimore). 2017;96:e8571.
Acknowledgements
The authors would like to acknowledge the help provided by the staff of the Honest Broker Service (HBS) within the Business Services Organisation Northern Ireland (BSO). The HBS is funded by the BSO and the Department of Health, Social Services and Public Safety for Northern Ireland (DHSSPSNI). The authors alone are responsible for the interpretation of the data and any views or opinions presented are solely those of the authors and do not necessarily represent those of the BSO.
Funding
This research received no specific grant from any funding agency, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest with respect to authorship and/or publication of this article.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For the purposes of conducting this study, governance approvals were obtained from: the Office for Research Ethics Committees Northern Ireland [ORECNI; reference: 14/NI/0065], the Governance Research Office in the Northern Health and Social Care Trust [reference: NRP14-0417-04], and the Honest Broker Governance Board [reference: 002/14]. For this type of study (retrospective in design), formal individual patient consent was not required.
Rights and permissions
About this article
Cite this article
Alnajjar, M.S., Aldeyab, M.A., Scott, M.G. et al. Influence of primary care antibiotic prescribing on incidence rates of multidrug-resistant Gram-negative bacteria in hospitalised patients. Infection 47, 781–791 (2019). https://doi.org/10.1007/s15010-019-01305-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s15010-019-01305-6