Abstract
Purpose
Vascular age (VA) is the direct index to reflect vascular aging, so it plays a particular role in public health. How to obtain VA conveniently and cheaply has always been a research hotspot. This study proposes a new method to evaluate VA with wrist pulse signal.
Methods
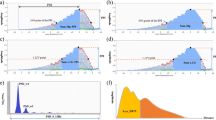
Firstly, we fit the pulse signal by mixed Gaussian model (MGM) to extract the shape features, and adopt principal component analysis (PCA) to optimize the dimension of the shape features. Secondly, the principal components and chronological age (CA) are respectively taken as the independent variables and dependent variable to establish support vector regression (SVR) model. Thirdly, the principal components are fed into the SVR model to predicted the vascular aging of each subject. The predicted value is regarded as the description of VA. Finally, we compare the correlation coefficients of VA with pulse width (PW), inflection point area ratio (IPA), Ratio b/a (RBA), augmentation index (AIx), diastolic augmentation index (DAI) and pulse transit time (PTT) with those of CA with these six indices.
Results
Compared with the CA, the VA is closer to PW (r = 0.539, P < 0.001 to r = 0.589, P < 0.001 in men; r = 0.325, P < 0.001 to r = 0.400, P < 0.001 in women), IPA (r = − 0.446, P < 0.001 to r = − 0.534, P < 0.001 in men; r = − 0.623, P < 0.001 to r = − 0.660, P < 0.001 in women), RBA (r = 0.328, P < 0.001 to r = 0.371, P < 0.001 in women), AIx (r = 0.659, P < 0.001 to r = 0.738, P < 0.001 in men; r = 0.547, P < 0.001 to r = 0.573, P < 0.001 in women), DAI (r = 0.517, P < 0.001 to r = 0.532, P < 0.001 in men; r = 0.507, P < 0.001 to r = 0.570, P < 0.001 in women) and PTT (r = 0.526, P < 0.001 to r = 0.659, P < 0.001 in men; r = 0.577, P < 0.001 to r = 0.814, P < 0.001 in women).
Conclusion
The VA is more representative of vascular aging than CA. The method presented in this study provides a new way to directly and objectively assess vascular aging in public health.






Similar content being viewed by others
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the agreement of the funding but are available from the corresponding author on reasonable request.
References
Lakatta EG, Levy D. Arterial and cardiac aging: major shareholders in cardiovascular disease enterprises. Part I: aging arteries: a ‘Set Up’ for vascular disease. Circulation. 2003;107:139–46. https://doi.org/10.1161/01.CIR.0000048892.83521.58.
Price MA, Alvarado BE, Rosendaal NTA, et al. Early and surgical menopause associated with higher Framingham Risk Scores for cardiovascular disease in the Canadian Longitudinal Study on Aging. Menopause (New York NY). 2021;28(5):484–90. https://doi.org/10.1097/GME.0000000000001729.
Hippisley-Cox J, Coupland C, Vinogradova Y, et al. Predicting cardiovascular risk in England and Wales: prospective derivation and validation of QRISK2. BMJ. 2008;336:1475–82. https://doi.org/10.1136/bmj.39609.449676.25.
Nashef SAM, Roques F, Michel P, et al. European system for cardiac operative risk evaluation (Euro-SCORE). Eur J Cardiothorac Surg. 1999;16:9–13. https://doi.org/10.1016/S1010-7940(99)00134-7.
Mancia G, Laurent S, Agabiti-Rosei E, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27:2121–58. https://doi.org/10.3109/08037050903450468.
Willeit P, Tschiderer L, Allara E, et al. Carotid intima-media thickness progression as surrogate marker for cardiovascular risk. Circulation. 2020;142:621–42. https://doi.org/10.1161/CIRCULATIONAHA.120.046361.
Kelly R, Hayward C, Avolio A, et al. Noninvasive determination of age-related changes in the human arterial pulse. Circulation. 1989;80(6):1652–9. https://doi.org/10.1161/01.CIR.80.6.1652.
Zhang YL, Zheng YY, Ma ZC, et al. Radial pulse transit time is an index of arterial stiffness. Hypertens Res. 2011;34(7):884–7. https://doi.org/10.1038/hr.2011.41.
Zheng YY, Lung CW, Zhang YL, et al. Radial diastolic augmentation index is a useful predictor of arterial stiffness. J Mech Med Biol. 2012;12(1):1–11. https://doi.org/10.1142/S0219519412004405.
Kim HL, Kim SH. Pulse wave velocity in atherosclerosis. Front Cardiovasc Med. 2019;6:41. https://doi.org/10.3389/fcvm.2019.00041.
Awad A, Haddadin A, Tantawy H, et al. The relationship between the photoplethysmographic waveform and systemic vascular resistance. J Clin Monit Comput. 2007;21(6):365–72. https://doi.org/10.1007/s10877-007-9097-5.
Wang L, Pickwell-MacPherson E, Liang YP, et al. Noninvasive cardiac output estimation using a novel photoplethysmogram index. In: Annual international conference of the IEEE Engineering in Medicine and Biology Society, 2009, pp 1746–9. https://doi.org/10.1109/IEMBS.2009.5333091.
Takazawa K, Tanaka N, Fujita M, et al. Assessment of vasoactive agents and vascular aging by the second derivative of photoplethysmogram waveform. Hypertension. 1998;32:365–70. https://doi.org/10.1161/01.HYP.32.2.365.
Tang QF, Huang L, Pan ZG. Multiple linear regression model for vascular aging assessment based on radial artery pulse wave. Eur J Integr Med. 2019;28:92–7. https://doi.org/10.1016/j.eujim.2019.05.006.
Xu LS, Meng MQH, Shi C, et al. Quantitative analyses of pulse images in Traditional Chinese Medicine. Med Acupunct. 2008;20:175–89. https://doi.org/10.1089/acu.2008.0632.
Velik R. An objective review of the technological developments for radial pulse diagnosis in Traditional Chinese Medicine. Eur J Integr Med. 2015;7:321–31. https://doi.org/10.1016/j.eujim.2015.06.006.
Wang H. A quantitative method for pulse strength classification based on decision tree. In: International symposium on information science and engineering, 2008, pp 111–15. https://doi.org/10.1109/ISISE.2008.164.
Imanaga I, Hara H, Koyanagi S, et al. Correlation between wave components of the second derivative of plethysmogram and arterial distensibility. Jpn Heart J. 1998;39:775–84. https://doi.org/10.1536/ihj.39.775.
Aiba Y, Ohshiba S, Horiguchi S, et al. Peripheral hemodynamics evaluated by acceleration plethysmography in workers exposed to lead. Ind Health. 1999;37:3–8. https://doi.org/10.2486/indhealth.37.3.
Nousou N, Urase S, Maniwa Y, et al. Classification of acceleration plethysmogram using self-organizing map. In: International symposium on intelligent signal processing and communications 2006, ISPACS '06, 2006, pp 681–4. https://doi.org/10.1109/ISPACS.2006.364747.
Otsuka T, Kawada T, Katsumata M, et al. Utility of second derivative of the finger photoplethysmogram for the estimation of the risk of coronary heart disease in the general population. Circ J. 2006;70:304–410. https://doi.org/10.1253/circj.70.304.
Vriz O, Palatini P, Mos L, et al. Augmentation index predicts mortality in patients with aortic stenosis: an echo-tracking study. Int J Cardiovasc Imaging. 2021;37:1659–68. https://doi.org/10.1007/s10554-020-02151-6.
An DW, Muhammad IF, Li MX, et al. Carotid-femoral pulse transit time variability predicted mortality and improved risk stratification in the elderly. Hypertension. 2021;78:1287–95. https://doi.org/10.1161/HYPERTENSIONAHA.121.17891.
Groenewegen KA, Ruijter HM, Pasterkamp G, et al. Vascular age to determine cardiovascular disease risk: a systematic review of its concepts, definitions, and clinical applications. Eur J Prev Cardiol. 2016;23(3):264–74. https://doi.org/10.1177/2047487314566999.
Stein JH, Fraizer MC, Aeschlimann SE, et al. Vascular age: integrating carotid intima-media thickness measurements with global coronary risk assessment. Clin Cardiol. 2004;27:388–92. https://doi.org/10.1002/clc.4960270704.
Guaraldi G, Zona S, Alexopoulos N, et al. Coronary aging in HIV-infected patients. Clin Infect Dis. 2009;49:1756–62. https://doi.org/10.1086/648080.
Romanens M, Ackermann F, Sudano I, et al. Arterial age as a substitute for chronological age in the AGLA risk function could improve coronary risk prediction. Swiss Med Wkly. 2014;144:13967. https://doi.org/10.4414/smw.2014.13899.
Reece AS, Hulse GK. Impact of lifetime opioid exposure on arterial stiffness and vascular age: cross-sectional and longitudinal studies in men and women. BMJ Open. 2014;4: e004521. https://doi.org/10.1136/bmjopen-2013-004521.
Cuende JI, Cuende N, Calaveras-Lagartos J. How to calculate vascular age with the SCORE project scales: a new method of cardiovascular risk evaluation. Eur Heart J. 2010;31:2351–8. https://doi.org/10.1093/eurheartj/ehq205.
McClelland RL, Nasir K, Budoff M, et al. Arterial age as a function of coronary artery calcium (from the Multi-Ethnic Study of Atherosclerosis (MESA)). Am J Cardiol. 2009;103:59–63. https://doi.org/10.1016/j.amjcard.2009.02.022.
McClelland RL, Chung H, Detrano R, et al. Distribution of coronary artery calcium by race, gender, and age: results from the Multi-Ethnic Study of Atherosclerosis (MESA). Circulation. 2006;113(1):30–7. https://doi.org/10.1161/CIRCULATIONAHA.105.580696.
Savitzky A, Golay MJE. Smoothing and differentiation of data by simplified least squares procedures. Anal Chem. 1964;36:1627–39. https://doi.org/10.1021/ac60319a045.
Elgendi M. PPG signal analysis—an introduction using MATLAB. Boca Raton: CRC Press; 2021.
Pan ZQ, Tao CL, Tang QF. A fourth derivative-based tool for pulse signal special point identification. In: Thirteenth international conference on graphics and image processing (ICGIP 2021), Kunming, China, 2021. https://doi.org/10.1117/12.2623173.
An XM, Yang R, Alghazzawi DM, et al. Mathematical function data model analysis and synthesis system based on short-term human movement. Appl Math Nonlinear Sci. 2021. https://doi.org/10.2478/amns.2021.2.00088.
Chraibi M, Ensslen T, Gottschalk H, et al. Assessment of models for pedestrian dynamics with functional principal component analysis. Physica A. 2016;451:475–89. https://doi.org/10.1016/j.physa.2016.01.058.
Onel M, Kieslich CA, Pistikopoulos EN. A nonlinear support vector machine-based feature selection approach for fault detection and diagnosis: application to the Tennessee Eastman process. AIChE J. 2019;65(3):992–1005. https://doi.org/10.1002/aic.16497.
Cervantes J, Garcia-Lamont F, Rodríguez-Mazahua L, et al. A comprehensive survey on support vector machine classification: applications, challenges and trends. Neurocomputing. 2020;408:189–215. https://doi.org/10.1016/j.neucom.2019.10.118.
Lin GQ, Li LL, Tseng ML, et al. An improved moth-flame optimization algorithm for support vector machine prediction of photovoltaic power generation. J Clean Prod. 2020;253: 119966. https://doi.org/10.1016/j.jclepro.2020.119966.
Sorelli M, Perrella A, Bocchi L. Detecting vascular age using the analysis of peripheral pulse. IEEE TBME. 2018;65(12):2742–50. https://doi.org/10.1109/tbme.2018.2814630.
Lin CJ. LIBSVM tools, 2018. https://www.csie.ntu.edu.tw/~cjlin/libsvm/index.html#nuandone. Accessed 19 May 2018.
Su BY, Tang QF, Wang GJ, et al. The recognition of human daily actions with wearable motion sensor system. LNCS Trans Edutainment. 2016;9292:68–77. https://doi.org/10.1007/978-3-662-50544-1_6.
Acknowledgements
We are grateful to Hangzhou Health Management Center.
Funding
This work is supported by National Nature Science Foundation of China (No. 61603003), Anhui Provincial Natural Science Foundation (No. 2108085QF269), Zhejiang Provincial Natural Science Foundation (No. LZ21F020008), and the Key Project on Anhui Provincial Natural Science Study by Colleges and Universities (No. KJ2019A055).
Author information
Authors and Affiliations
Contributions
All research done by the authors. Su and Pan designed this research, manuscript writing was mainly accomplished by Tang. Data collection was mainly accomplished by Xu. Wang and Guo contributed in data preprocessing.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All subjects agreed to participate and undertake the tests given by the doctor. This study complied with the principles of the Declaration of 1964 Helsinki and was approved by the Ethics Committee of our institution.
Informed consent
A signed informed consent form was provided before testing.
Consent for publication
The picture materials quoted in this article have no copyright requirements, and the source has been indicated.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tang, Q., Xu, S., Guo, M. et al. Wrist pulse signal based vascular age calculation using mixed Gaussian model and support vector regression. Health Inf Sci Syst 10, 7 (2022). https://doi.org/10.1007/s13755-022-00172-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13755-022-00172-0