Abstract
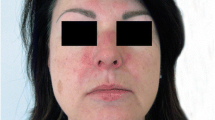
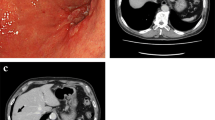
Dermatomyositis (DM) is an autoimmune disease that causes proximal muscle weakness in the extremities leading to severe immobility and dysphagia. Approximately 20% of patients with DM are positive for anti-TIF-1γ antibody and frequently accompanied by malignant tumors. Although DM remission after tumor resection has been reported, the indications for surgery in patients with severe DM are unknown. Herein, we report a case of a 79-year-old Japanese woman who presented with breast cancer and anti-TIF-1γ antibody-positive DM. She became bedridden shortly after DM onset. Although pulsed steroid therapy, intravenous immunoglobulin, tacrolimus, and endocrine therapy with fulvestrant did not improve her symptoms, tumor resection with axillary lymph node dissection resulted in complete remission of the DM after 8 months. Immunohistochemistry revealed high expression of TIF-1γ in cancer cells, both in the primary tumor and axillary lymph nodes. Since the serum levels of anti-TIF-1γ antibody decreased after the surgery, the existence of breast cancer with TIF-1γ expression may have contributed to the worsening of DM. The present case suggests that curative surgery should be considered as a treatment option even if the patient has severe symptoms, such as immobility and dysphagia. Careful discussions with patients and multidisciplinary collaboration are essential to make surgery feasible, particularly for those with severe symptomatic DM.






Similar content being viewed by others
Data availability
All data related to this report are available from the corresponding author upon reasonable request.
References
Sandhu NP, Zakaria S, Degnim AC, Boughey JC (2011) Dermatomyositis presenting as a paraneoplastic syndrome due to underlying breast cancer. BMJ Case Rep 2011
Kubeček O, Soukup T, Paulík A, Kopecký J (2016) Dermatomyositis with anti-TIF-1γ antibodies as a presenting symptom of underlying triple-negative breast cancer: a case report. BMC Cancer 16(1):684
Piras M, Panebianco M, Garibaldi M, Roberto M, Merlonghi G, Pellegrini P et al (2021) A case of pathological complete response and resolution of dermatomyositis following neoadjuvant chemotherapy in HER2-positive early breast cancer. Curr Oncol 28(3):1957–1961
Kassem L, Deygas M, Fattet L, Lopez J, Goulvent T, Lavergne E et al (2015) TIF1γ interferes with TGFβ1/SMAD4 signaling to promote poor outcome in operable breast cancer patients. BMC Cancer 15:453
Blanes M, Bañuls J, Yuste A, Adrover E, Pascual JC, Pastor N et al (2005) Amyopathic dermatomyositis associated with a recurrence of breast cancer. Actas Dermosifiliogr 96(5):299–302
Pectasides D, Koumpou M, Gaglia A, Pectasides M, Lambadiari V, Lianos E et al (2006) Dermatomyositis associated with breast cancer. Anticancer Res 26(3b):2329–2331
Sereda D, Werth VP (2006) Improvement in dermatomyositis rash associated with the use of antiestrogen medication. Arch Dermatol 142(1):70–72
Esposito AC, Munhoz T, Ocanha JP, Miot HA (2016) Syndrome in question. An Bras Dermatol 91(3):387–389
Yamashita H, Kobayashi S, Iwase H, Itoh Y, Masaoka A (1994) Recurrent breast cancer at 21 years after resection detected by serum tumor markers and manifested as dermatomyositis. Breast Cancer 1(1):65–68
Song YJ, Wu YF, Fan T (2010) Dermatosis as the initial manifestation of malignant breast tumors: retrospective analysis of 4 cases. Breast Care (Basel) 5(3):174–176
Kumar N, Deo S (2020) Paraneoplastic dermatomyositis in hereditary breast and ovarian cancer syndrome. Breast J 26(9):1836–1837
Osako T, Ito Y, Morimatsu A, Tada K, Sakurai N, Takahashi S et al (2007) Flare-up of dermatomyositis along with recurrence of breast cancer. Breast J 13(2):200–202
Sakai T, Ogura Y, Narita J, Kimura D, Suto T, Ainai S et al (2005) Metachronous bilateral primary breast cancer associated with dermatomyositis. Breast J 11(3):225–226
Hu T, Vinik O (2019) Dermatomyositis and malignancy. Can Fam Physician 65(6):409–411
Moghimi M, Khodadadi K (2021) Dermatomyositis following biosimilar trastuzumab in a breast cancer patient: a case report. Case Rep Oncol 14(2):1134–1138
Allouch A, Zaatarikahale TB, Moussa MK, Jounblat Y, Bitar N (2020) Dermatomyositis: a presenting clinical vignette in a patient with breast cancer. Cureus 12(9):e10624
Hendren E, Vinik O, Faragalla H, Haq R (2017) Breast cancer and dermatomyositis: a case study and literature review. Curr Oncol 24(5):e429–e433
Pellegrino B, Mazzaschi G, Madeddu D, Mori C, Lagrasta CAM, Missale G et al (2020) Clinico-immunological profile of a 67-year-old woman affected by HER2-positive breast cancer and autoimmune dermatomyositis. Front Oncol 10:192
Goto W, Kashiwagi S, Asano Y, Takada K, Morisaki T, Noda S et al (2017) A case of breast cancer associated with dermatitis that was difficult to differentiate from dermatomyositis. Gan To Kagaku Ryoho 44(12):1930–1932
Voravud N, Dimopoulos M, Hortobagyi G, Ross M, Theriault R (1991) Breast cancer and second primary ovarian cancer in dermatomyositis. Gynecol Oncol 43(3):286–290
Cai Y, Qiao J, Fang H (2012) Metachronous multiple primary malignant neoplasms in a patient with dermatomyositis. Indian J Dermatol Venereol Leprol 78(5):665
Kikuchi N, Ohashi T, Miura T, Nishibu A, Yamamoto T (2017) Triple cancers concurrently detected in a case of antitranscriptional intermediary factor-1γ antibody-positive dermatomyositis. Int J Dermatol 56(12):1516–1517
Otsuka Y, Watanabe H, Kano Y, Tatebe N, Sunahori-Watanabe K, Kawabata T et al (2017) Occurrence of dermatomyositis immediately after mastectomy subsequent to severe chemotherapeutic drug eruption. Intern Med 56(24):3379–3383
Goyal S, Nousari HC (1999) Paraneoplastic amyopathic dermatomyositis associated with breast cancer recurrence. J Am Acad Dermatol 41(5 Pt 2):874–875
Kim Y, Jung W, Park YH (2015) Dermatomyositis and paclitaxel-induced cutaneous drug eruption associated with metastatic breast cancer. J Breast Cancer 18(2):195–199
Daryanani S (1998) Dermatomyositis and breast cancer. J Clin Oncol 16(8):2890–2891
Ahuja S, Makkar P, Gupta S, Vigoda I (2016) Paraneoplastic syndrome and underlying breast cancer: a worsening rash despite initiation of chemotherapy. J Community Support Oncol 14(5):229–231
Matsushita T, Takehara K, Oishi K, Maeda S, Hamaguchi Y, Ishikawa S et al (2017) Case of anti-transcriptional intermediary factor-1-positive dermatomyositis associated with breast cancer developing over 10 years. J Dermatol 44(8):972–973
Ogawa M, Sugiura K, Yokota K, Muro Y, Akiyama M (2016) Anti-transcription intermediary factor 1-γ antibody-positive clinically amyopathic dermatomyositis complicated by interstitial lung disease and breast cancer. J Eur Acad Dermatol Venereol 30(2):373–375
Primiano G, Plantone D, Sauchelli D, Cuccagna C, Renna R, Iorio R et al (2012) Resolution of muscle inflammation after tumor removal in a woman with paraneoplastic dermatomyositis. J Rheumatol 39(12):2359–2360
Luu X, Leonard S, Joseph KA (2015) Dermatomyositis presenting as a paraneoplastic syndrome with resolution of symptoms following surgical management of underlying breast malignancy. J Surg Case Rep 2015(7):rjv075
Khoo HY, Tan WJ, Cheong YT (2018) Breast cancer with dermatomyositis as initial presentation. Med J Malaysia 73(1):44–45
Yesmin S, Sanyal M, Hasan MJ (2019) Breast cancer with paraneoplastic syndrome in a 72 year old male patient. Mymensingh Med J 28(1):254–258
Zhang L, Zhang C, Yang Z, He M, Zhang L, Ezzat S et al (2017) Male occult triple-negative breast cancer with dermatomyositis: a case report and review of the literature. Onco Targets Ther 10:5459–5462
Biyi A, Doudouh A (2016) Muscular visualisation on a bone scan in paraneoplastic dermatomyositis associated with breast cancer. Pan Afr Med J 23:9
Lamquami S, Errarhay S, Mamouni N, Bouchikhi C, Banani A (2015) Dermatomyositis revealing breast cancer: report of a case. Pan Afr Med J 21:89
Vaccaro M, Borgia F, Barbuzza O, Gangemi S, Guarneri B (2010) Dermatomyositis and cutaneous metastases from breast cancer: simultaneous development and parallel course. Rheumatol Int 30(8):1091–1093
Inaguma G, Shimada A, Tsunoda J, Matsuzaki T, Nishi T, Seki H et al (2020) Inflammatory breast cancer associated with amyopathic dermatomyositis: a case report. Surg Case Rep 6(1):284
Dias LP, Faria AL, Scandiuzzi MM, Inhaia CL, Shida JY, Gebrim LH (2015) A rare case of severe myositis as paraneoplastic syndrome on breast cancer. World J Surg Oncol 13:134
Acknowledgements
The authors thank Dr. Ayako Kojima, Department of Dermatology of Uji Takeda Hospital, the Center for Anatomical, Pathological, and Forensic Medical Research, Kyoto University Graduate School of Medicine for preparing the microscope slides. Explorative staining was performed with the approval of the Ethics Committee of Kyoto University Hospital (Protocol Number; G424).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Masahiro Kawashima received lecture fees from Pfizer Japan Inc., Daiichi Sankyo, Guardant Health AMEA, Eisai Co., Ltd., and Chugai Pharmaceutical Co., Ltd.. Masahiro Kawashima received research fundings from Nippon Kayaku Co., Ltd., and Kyowa Kirin Co., Ltd.. Nobuko Kawaguchi-Sakita has an endowed chair at Fujitsu, Meiji Seika Pharma, Yakult, NTT, PRiME-R, CANNON Medical, HUG, NTT-DATA, and IHC. Masahiro Takada received lecture fees from Chugai Pharmaceutical Co., Ltd., Astra Zeneca K.K., and Daiichi Sankyo. Masahiro Takada received research fundings from Astra Zeneca K.K., Daiichi Sankyo, Eisai Co.,Ltd., KBCRN, JBCRG, ABCSG, Yakult Honsha Co., Ltd., MedBis co., Ltd., and IQVIA Japan. Masakazu Toi has a leadership position of JBCRG, KBCRN, OOTR, and JBCS. Masakazu Toi has an advisory role of Daiichi-Sankyo, Eli Lilly and companies, Bristol Myers Squibb, Athenex Oncology, Bertis Inc., Terumo Corporation, and Kansai Medical Net. Masakazu Toi received lecture fees from Chugai Pharmaceutical Co.,Ltd., Takeda Pharmaceuticals, Pfizer Japan Inc., Kyowa Kirin Co., Ltd., Taiho Pharmaceutical Co., Ltd., Eisai Co., Ltd., Daiichi-Sankyo, Astra Zeneca K.K., Eli Lilly and companies, MSD K.K., EXACT Sciences, Novartis Pharmaceuticals, Shimadzu Corporation, Yakult, Nippon Kayaku Co., Ltd., Devicor Medical Japan K.K., and Sysmex Corporation. Masakazu Toi received research funding from Chugai Pharmaceutical Co., Ltd., Takeda Pharmaceuticals, Pfizer Japan Inc., Taiho Pharmaceutical Co., Ltd., JBCRG, KBCRN, Eisai Co., Ltd., Eli Lilly and companies, Daiichi Sankyo, Astra Zeneca K.K., Astellas Pharma Inc., Shimadzu Corporation, Yakult Honsha Co., Ltd., Nippon Kayaku Co., Ltd., AFI Corporation, Luxonus Inc., Shionogi Pharma Co., Ltd., and GL Sciences Inc.. The other authors declare that they have no conflict of interest.
Ethics approval
Research Ethics Committee approval was waved due to the nature of case report.
Informed consent
Informed consent was obtained from the patient included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Fujino, M., Kawashima, M., Yoshifuji, H. et al. Remarkable remission of symptomatic dermatomyositis after curative breast cancer surgery. Int Canc Conf J 13, 111–118 (2024). https://doi.org/10.1007/s13691-023-00646-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-023-00646-2