Abstract
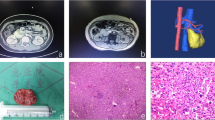
Carotid body tumor involving the succinate dehydrogenase subunit B (SDHB) variant reportedly had a higher frequency of metastasis than other variants of succinate dehydrogenase. However, the correlation between genotype and phenotype among patients with carotid body tumor with SDHB gene variant remains unclear. Thus, we present a case of carotid body tumor with neck lymph metastasis caused by a novel SDHB variant, which resulted in long-term disease-free survival achieved after surgery. A 43-year-old man presented to our hospital with a 2-year history of a painless neck mass. Based on the radiographic findings, the patient was diagnosed with carotid body tumor with a possible Shamblin type III tumor. Another mass was detected and suspected to be a lymph node metastasis. The patient underwent resection of the tumor and lymph nodes. The common carotid artery, internal carotid artery, external carotid artery, internal jugular vein, vagal nerve, and hypoglossal nerve were resected with the tumor. Histopathological examination revealed a paraganglioma. The histological findings of the lymph nodes were similar to those of the carotid body tumor and were confirmed to be metastases of paraganglioma. To analyze the germline SDHx variant, a nonsense variant was detected in the SDHB gene at exon 2, c. 136C > T, p. Arg46*. During the follow-up 80 months after surgery, the patient exhibited no signs of recurrence, metastasis, or development of paragangliomas in other organs. This was the first case of carotid body tumor accompanied by neck metastasis caused by a germline nonsense SDHB variant at exon 2, c. 136C > T, p. Arg46*. Carotid body tumor with neck lymph metastasis caused by this nonsense variant could achieve long-term disease-free survival after surgery. Gene analysis, including SDHB variant, should be performed to predict the prognosis and future risk of metastasis. Genetic testing of SDHB may give a crucial information for the treatment and follow-up strategies of carotid body tumor.



Similar content being viewed by others
Data availability
Not applicable.
References
Kimura N, Lam AKY, Capella C et al (2017) Carotid body paraganglioma. In: El-Naggar AK, Chan JKC, Grandis JR et al (eds) WHO classification of head and neck tumors, 4th edn. IARC, Lyon, pp 277–280
Jochmanova I, Wolf KI, King KS et al (2017) SDHB-related pheochromocytoma and paraganglioma penetrance and genotype-phenotype correlations. J Cancer Res Clin Oncol 143:1421–1435
Tufton N, Sahdev A, Drake WM et al (2019) Can subunit-specific phenotypes guide surveillance imaging decisions in asymptomatic SDH mutation carriers? Clin Endocrinol (Oxf) 90:31–46
Shamblin WR, ReMine WH, Sheps SG et al (1971) Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg 122:732–739
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17:405–424
Williams MD (2017) Paragangliomas of the head and neck: an overview from diagnosis to genetics. Head Neck Pathol 11:278–287
Barbolosi D, Crona J, Serre R et al (2018) Methematical modeling of disease dynamics in SDHB- and SDHD-related paraganglioma: Further step in understanding hereditary tumor differences and future therapeutic strategies. PLoS ONE 13:e0201303
Timmers HJ, Pacak K, Huynh TT et al (2008) Biochemically silent abdominal paragangliomas in patients with mutations in the succinate dehydrogenase subunit B gene. J Clin Endocrinol Metab 93:4826–4832
Lodish MB, Adams KT, Huynh TT et al (2010) Succinate dehydrogenase gene mutations are strongly associated with paraganglioma of the organ of Zuckerkandl. Endocr Relat Cancer 17:581–588
Ghayee HK, Havekes B, Corssmit EP et al (2009) Mediastinal paragangliomas: association with mutations in the succinate dehydrogenase genes and aggressive behavior. Endocr Relat Cancer 16:291–299
Srirangalingam U, Walker L, Khoo B et al (2008) Clinical manifestations of familial paraganglioma and phaeochromocytomas in succinate dehydrogenase B (SDH-B) gene mutation carriers. Clin Endocrinol (Oxf) 69:587–596
Benn DE, Gimenez-Roqueplo AP, Reilly JR et al (2006) Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J Clin Endocrinol Metab 91:827–836
Benn DE, Croxson MS, Tucker K et al (2003) Novel succinate dehydrogenase subunit B (SDHB) mutations in familial phaeochromocytomas and paragangliomas, but an absence of somatic SDHB mutations in sporadic phaeochromocytomas. Oncogene 22:1358–1364
Sriphrapradang C, Choopun K, Tunteeratum A et al (2017) Genotype-phenotype correlation in patients with germline mutations of VHL, RET, SDHB, and SDHD genes: Thai experience. Clin Med Insights Endocrinol Diabetes. https://doi.org/10.1177/1179551417705122
Bayley JP, van Minderhout I, Weiss MM et al (2006) Mutation analysis of SDHB and SDHC: novel germline mutations in sporadic head and neck paraganglioma and familial paraganglioma and/or pheochromocytoma. BMC Med Genet. https://doi.org/10.1186/1471-2350-7-1
Pandit R, Khadilkar K, Sarathi V et al (2016) Germline mutations and genotype-phenotype correlation in Asian Indian patients with pheochromocytoma and paraganglioma. Eur J Endocrinol 175:311–323
Chew WHW, Courtney E, Lim KH et al (2017) Clinical management of pheochromocytoma and paraganglioma in Singapore: missed opportunities for genetic testing. Mol Genet Genomic Med 5:602–607
Burnichon N, Rohmer V, Amar L et al (2009) The succinate dehydrogenase genetic testing in a large prospective series of patients with paragangliomas. J Clin Endcrinol Metab 94:2817–2827
Brouwers FM, Eisenhofer G, Tao JJ et al (2006) High frequency of SDHB germline mutations in patients with malignant catecholamine-producing paragangliomas: implications for genetic testing. J Clin Endocrinol Metab 91:4505–4509
Lioyd RV, Osamura RY, Klöppel G et al (2017) WHO classification of endocrine organs, 4th edn. IARC, Lyon
Ellis RJ, Patel D, Prodanov T et al (2014) The presence of SDHB mutations should modify surgical indications for carotid body paragangliomas. Ann Surg 260:158–162
Acknowledgements
We thank the patient for providing consent and Editage (www.editage.jp) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the patient’s diagnosis and treatment. HO and KY contributed to gene analysis. TM prepared the draft of the paper. TM and HO were responsible for the writing of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The case report was approved by the Institutional Review Board and Research Ethics Committee of Keio University School of Medicine (reference number 20190093).
Informed consent
Written informed consent for publication was obtained from the patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Mikoshiba, T., Yoshihama, K., Ito, F. et al. Carotid body tumor with neck metastasis due to germline SDHB variant: a case report and literature review. Int Canc Conf J 11, 6–11 (2022). https://doi.org/10.1007/s13691-021-00522-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13691-021-00522-x