Abstract
Purpose of Review
This paper aims to describe the heterogenous presentation of agitation in older adults. It will delve into semiology, diagnosis, classification, as well as treatment options available to address agitation.
Recent Findings
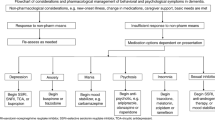
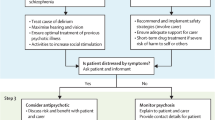
Agitation is a common and distressing symptom that poses risk to patients and caregivers. In older adults, it is often a manifestation of medical and neuropsychiatric conditions such as dementia, stroke, delirium, psychiatric disorders, catatonia, substance intoxication or withdrawal. Agitation in dementia is defined as excessive motor behavior and verbal or physical aggressive behavior, causing significant disability. Several tools are used to describe it; most notably, the Cohen-Mansfield Agitation Inventory (CMAI). Its evaluation is most complete with the DICE (Describe, Investigate, Create, Evaluate) approach which allows for examination of precipitating factors such as delirium, psychiatric disorders, pain, polypharmacy, constipation, environmental elements, and others. Non-pharmacological management should be attempted first, tailoring the treatment to the precipitants. If these fail, pharmacological treatments, although inherently risky, include non-emergent and emergent options. The former are antidepressants and cognitive enhancers, and the latter include antipsychotics, trazodone, and electroconvulsive therapy (ECT). Benzodiazepine use should be limited to excited catatonia or alcohol withdrawal.
Summary
Agitation management is as much about addressing unmet needs as it is about treatment of underlying etiologies. A careful and systematic approach is imperative to successful treatment. It allows the clinician to uncover what the patient is unable to convey and minimizes the risk that polypharmacy may bring. More research is needed into methods to quantify, anticipate, and safely treat agitation in older adults.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Ashman JJ, Schappert SM, Santo L. Emergency Department Visits Among Adults Aged 60 and Over: United States, 2014–2017, NCHS Data Brief No. 367. Hyattsville, MD; 2020.
•Kennedy M, Koehl J, Shenvi CL, Greenberg A, Zurek O, LaMantia M, et al. The agitated older adult in the emergency department: a narrative review of common causes and management strategies. J Am Coll Emerg Physicians Open. 2020;(March):812–23. This recently published article is a helpful review of the approach to evaluating and treating the agitated older adult who presents to the emergency department.
Maust DT, Kales HC, McCammon RJ, Blow FC, Leggett A, Langa KM. Distress associated with dementia-related psychosis and agitation in relation to healthcare utilization and costs. Am J Geriatr Psychiatry Off J Am Assoc Geriatr Psych. 2017;25(10):1074–82.
Bessey LJ, Radue RM, Chapman EN, Boyle LL, Shah MN. Behavioral health needs of older adults in the emergency department. Clin Geriatr Med. 2018 Aug;34(3):469–89.
••Tampi RR, Tampi DJ, Balachandran S. Antipsychotics, antidepressants, anticonvulsants, melatonin, and benzodiazepines for behavioral and psychological symptoms of dementia: a systematic review of meta-analyses. Curr treat options Psychiatry [Internet]. 2017;4(1):55–79. Available from: https://doi.org/10.1007/s40501-017-0104-2. This systematic review is a comprehensive overview of the evidence base for various pharmacologic strategies for the management of agitation in dementia.
Chen A, Copeli F, Metzger E, Cloutier A, Osser DN. The psychopharmacology algorithm project at the Harvard south shore program: an update on management of behavioral and psychological symptoms in dementia. Psychiatry Res. 2021 Jan;295:113641.
Tampi RR, Williamson D, Muralee S, Mittal V, McEnerney N, Thomas J, et al. Behavioral and psychological symptoms of dementia: Part II-treatment. Clin Geriatr. 2011;19(6).
••Yunusa I, Alsumali A, Garba AE, Regestein QR, Eguale T. Assessment of reported comparative effectiveness and safety of atypical antipsychotics in the treatment of behavioral and psychological symptoms of dementia: a network meta-analysis. JAMA Netw Open. 2019;2(3):e190828. In this recently published network meta-analysis, authors assessed the relative benefits and safety of atypical antipsychotics in the treatment of behavioral symptoms of dementia.
Cummings J, Mintzer J, Brodaty H, Sano M, Banerjee S, Devanand DP, et al. Agitation in cognitive disorders: international psychogeriatric association provisional consensus clinical and research definition. Int Psychogeriatrics. 2015;27(1):7–17.
Cohen-Mansfield J. Assessment of disruptive behavior/agitation in the elderly: function, methods, and difficulties. J Geriatr Psychiatry Neurol. 1995;8(1):52–60.
Griffiths AW, Albertyn CP, Burnley NL, Creese B, Walwyn R, Holloway I, et al. Validation of the Cohen-Mansfield agitation inventory observational (CMAI-O) tool. Int Psychogeriatrics. 2020;32(1):75–85.
Kales HC, Gitlin LN, Lyketsos CG. Management of neuropsychiatric symptoms of dementia in clinical settings: recommendations from a multidisciplinary expert panel. J Am Geriatr Soc. 2014;62(4):762–9.
Amjad H, Roth DL, Sheehan OC, Lyketsos CG, Wolff JL, Samus QM. Underdiagnosis of dementia: an observational study of patterns in diagnosis and awareness in US older adults. J Gen Intern Med. 2018;33(7):1131–8.
Cohen-Mansfield J, Billig N. Agitated behaviors in the elderly. I. a conceptual review. J Am Geriatr Soc. 1986 Oct;34(10):711–21.
Cohen-Mansfield J. Agitated behaviors in the elderly. II. Preliminary results in the cognitively deteriorated. J Am Geriatr Soc. 1986 Oct;34(10):722–7.
Finkel SI, Lyons JS, Anderson RL. Cohen-Mansfield agitation inventory in institutionalized elderly. Int J Geriatr Psychiatry. 1992;7(November 1991):4–7.
Kopecky HJ, Kopecky CR, Yudofsky SC. Reliability and validity of the overt agitation severity scale in adult psychiatric inpatients. Psychiatr Q. 1998;69(4):301–23.
Swift RH, Harrigan EP, Cappelleri JC, Kramer D, Chandler LP. Validation of the behavioural activity rating scale (BARS): a novel measure of activity in agitated patients. J Psychiatr Res. 2002;36(2):87–95.
De Medeiros K, Robert P, Gauthier S, Stella F, Politis A, Leoutsakos J, et al. The neuropsychiatric inventory-clinician rating scale (NPI-C): reliability and validity of a revised assessment of neuropsychiatric symptoms in dementia. Int Psychogeriatrics. 2010;22(6):984–94.
Nordstrom K, Zun LS, Wilson MP, Stiebel V, Ng AT, Bregman B, et al. Medical evaluation and triage of the agitated patient: consensus statement of the American association for emergency psychiatry project BETA medical evaluation workgroup. West J Emerg Med. 2012;13(1):3–10.
Geda YE, Schneider LS, Gitlin LN, Co-chair DSMN, Smith GS, Bell J, et al. Progress and anticipation of the future. Alzheimers Dement. 2014;9(5):602–8.
Lyketsos CG. Neuropsychiatric symptoms in dementia: overview and measurement challenges. J Prev Alzheimer’s Dis [Internet]. 2015;2(3):155–6 Available from: http://www.ncbi.nlm.nih.gov/pubmed/26779454%0Ahttp://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=PMC4712963.
Oh ES, Fong TG, Hshieh TT, Inouye SK. Delirium in older persons: advances in diagnosis and treatment. JAMA - J Am Med Assoc. 2017;318(12):1161–74.
Haigh EAP, Bogucki OE, Sigmon ST, Blazer DG. Depression among older adults: a 20-year update on five common myths and misconceptions. Am J Geriatr Psychiatry [Internet]. 2018;26(1):107–22. Available from: https://doi.org/10.1016/j.jagp.2017.06.011.
Sampson EL, White N, Lord K, Leurent B, Vickerstaff V, Scott S, et al. Pain, agitation, and behavioural problems in people with dementia admitted to general hospital wards: a longitudinal cohort study. Pain. 2015;156(4):675–83.
Siddiqi N, House AO, Holmes JD. Occurrence and outcome of delirium in medical in-patients: a systematic literature review. Age Ageing. 2006;35(4):350–64.
Inouye SK. Delirium in hospitalized older patients: recognition and risk factors. J Geriatr Psychiatry Neurol. 1998;11(3):118–25.
Fong TG, Tulebaev SR, Inouye SK. Delirium in older adults: diagnosis, prevention, and treatment. B C Med J. 2017;59(3):165–70.
Golchin N, Frank SH, Vince A, Isham L, Meropol SB. Polypharmacy in the elderly. J Res Pharm Pract [Internet]. 2015;4(2):85–8 Available from: https://pubmed.ncbi.nlm.nih.gov/25984546.
Fong TG, Davis D, Growdon ME, Albuquerque A, Inouye SK. The interface between delirium and dementia in elderly adults. Lancet Neurol [Internet]. 2015/06/29. 2015 Aug;14(8):823–32. Available from: https://pubmed.ncbi.nlm.nih.gov/26139023
Reynish EL, Hapca SM, De Souza N, Cvoro V, Donnan PT, Guthrie B. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: prospective cohort study of 10,014 admissions. BMC Med. 2017;15(1):1–12.
Hegeman AJM, Kok RM, Van Der Mast RC, Giltay EJ. Phenomenology of depression in older compared with younger adults: meta-analysis. Br J Psychiatry. 2012;200(4):275–81.
Chau DL, Walker V, Pai L, Cho LM. Opiates and elderly: use and side effects. Clin Interv Aging. 2008;3(2):273–8.
Adelman RD, Tmanova LL, Delgado D, Dion S, Lachs MS. Caregiver burden: a clinical review. JAMA - J Am Med Assoc. 2014;311(10):1052–9.
Kolanowski A, Boltz M, Galik E, Gitlin LN, Kales HC, Resnick B, et al. Determinants of behavioral and psychological symptoms of dementia: A scoping review of the evidence 2017;65(5):515–29.
Kim T, Jeong H, Won Han J, Kwak KP, Kim BJ, Kim SK, et al. Prevalence and risk factors of abusive behaviors in the caregivers of people with dementia in Korea. Psychiatry Investig. 2018;15(7):677–86.
Cooper C, Livingston G. Mental health/psychiatric issues in elder abuse and neglect. Clin Geriatr med [Internet]. 2014;30(4):839–50. Available from: https://doi.org/10.1016/j.cger.2014.08.011, 2014.
El Chakhtoura NG, Bonomo RA, Jump RLP. Influence of aging and environment on presentation of infection in older adults. Infect Dis Clin N Am. 2017 Dec;31(4):593–608.
Jesse S, Bråthen G, Ferrara M, Keindl M, Ben-Menachem E, Tanasescu R, et al. Alcohol withdrawal syndrome: mechanisms, manifestations, and management. Acta Neurol Scand. 2017 Jan;135(1):4–16.
Campanelli CM, Fick DM, Semla T, Beizer J. Potentially inappropriate medication use in older adults: the American Geriatrics Society 2012 beers criteria. J Am Geriatr Soc. 2012;60(4):616–31.
Christodoulou CG, Fineti K, Douzenis A, Moussas G, Michopoulos I, Lykouras L. Transfers to psychiatry through the consultation-liaison psychiatry service: 11 years of experience. Ann General Psychiatry. 2008;7:1–7.
Ricotta DN, Parris JJ, Parris RS, Sontag DN, Mukamal KJ. The burden of guardianship: a matched cohort study. J Hosp Med. 2018 Sep;13(9):595–601.
Abraha I, Rimland JM, Trotta FM, Dell’Aquila G, Cruz-Jentoft A, Petrovic M, et al. Systematic review of systematic reviews of non-pharmacological interventions to treat behavioural disturbances in older patients with dementia. the SENATOR-OnTop series. BMJ Open. 2017;7(3).
Brooker D. Dementia care mapping: A review of the research literature. Gerontologist. 2005;45(SPEC. ISS. 1):11–8.
Agens JE. Chemical and physical restraint use in the older person. Br J Med Pract. 2010;3(1).
Pan Y, Jiang Z, Yuan C, Wang L, Zhang J, Zhou J, et al. Influence of physical restraint on delirium of adult patients in ICU: a nested case-control study. J Clin Nurs. 2018 May;27(9–10):1950–7.
Wong AH, Taylor RA, Ray JM, Bernstein SL. Physical restraint use in adult patients presenting to a general emergency department. Ann Emerg Med. 2019 Feb;73(2):183–92.
Zun LS. A prospective study of the complication rate of use of patient restraint in the emergency department. J Emerg Med. 2003 Feb;24(2):119–24.
Shenvi C, Kennedy M, Austin CA, Wilson MP, Gerardi M, Schneider S. Managing delirium and agitation in the older emergency department patient: the ADEPT tool. Ann Emerg med [Internet]. 2020;75(2):136–45. Available from: 10.1016/j.annemergmed.2019.07.023.
Frueh BC, Knapp RG, Cusack KJ, Grubaugh AL, Sauvageot JA, Cousins VC, et al. Patients’ reports of traumatic or harmful experiences within the psychiatric setting. Psychiatr Serv. 2005 Sep;56(9):1123–33.
Tarsy D, Baldessarini RJ, Tarazi FI. Effects of newer antipsychotics on extrapyramidal function. CNS Drugs. 2002;16(1):23–45.
Sahlberg M, Holm E, Gislason GH, Køber L, Torp-Pedersen C, Andersson C. Association of selected antipsychotic agents with major adverse cardiovascular events and noncardiovascular mortality in elderly persons. J Am Heart Assoc. 2015;4(9):1–11.
Leung JG, Benedetti AM, Frazee LA, Myers N. Comparison of short-acting intramuscular antipsychotic medication: impact on length of stay and cost. Am J Ther. 2011 Jul;18(4):300–4.
Zirker W, Dorokhine I, Knapp CM, Patel N, Musuku M. Haloperidol overdosing in the treatment of agitated hospitalized older people with delirium: a retrospective chart review from a community teaching hospital. Drugs Aging. 2013;30(8):639–44.
Devanand DP, Strickler JG, Huey ED, Crocco E, Forester BP, Husain MM, et al. Lithium treatment for agitation in Alzheimer’s disease (lit-AD): clinical rationale and study design. Contemp Clin trials [Internet]. 2018;71(march):33–9. Available from: https://doi.org/10.1016/j.cct.2018.05.019.
Tannenbaum C. Inappropriate benzodiazepine use in elderly patients and its reduction. J Psychiatry Neurosci. 2015;40(3):E27–8.
Morrison JR. Catatonia: Retarded and Excited Types. Arch Gen Psychiatry [Internet]. 1973 Jan 1;28(1):39–41. Available from: https://doi.org/10.1001/archpsyc.1973.01750310023005.
Mann SC, Caroff SN, Bleier HR, Welz WK, Kling MA, Hayashida M. Lethal catatonia. Am J Psychiatry. 1986 Nov;143(11):1374–81.
Rasmussen SA, Mazurek MF, Rosebush PI. Catatonia: our current understanding of its diagnosis, treatment and pathophysiology. World J psychiatry [Internet]. 2016 Dec 22;6(4):391–8 Available from: https://pubmed.ncbi.nlm.nih.gov/28078203.
Mayo-Smith MF. Pharmacological management of alcohol withdrawal. A meta-analysis and evidence-based practice guideline. American Society of Addiction Medicine Working Group on pharmacological Management of Alcohol Withdrawal. JAMA. 1997 Jul;278(2):144–51.
Sachdeva A, Choudhary M, Chandra M. Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond. J Clin Diagn Res [Internet]. 2015/09/01. 2015 Sep;9(9):VE01–7. Available from: https://pubmed.ncbi.nlm.nih.gov/26500991
van den Berg JF, Kruithof HC, Kok RM, Verwijk E, Spaans HP. Electroconvulsive therapy for agitation and aggression in dementia: a systematic review. Am J Geriatr Psychiatry [Internet]. 2018;26(4):419–34. Available from: https://doi.org/10.1016/j.jagp.2017.09.023.
Acharya D, Harper DG, Achtyes ED, Seiner SJ, Mahdasian JA, Nykamp LJ, et al. Safety and Utility of Acute Electroconvulsive 2016;30(3):265–73.
Kerner N, Prudic J. Current electroconvulsive therapy practice and research in the geriatric population. Neuropsychiatry (London). 2014;4(1):33–54.
Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, et al. Effect of citalopram on agitation in Alzheimer’s disease – the CitAD randomized controlled trial. Jama. 2014;311(7):682–91.
Ho T, Pollock BG, Mulsant BH, Schantz O, Devanand DP, Mintzer JE, et al. R- and S-citalopram concentrations have differential effects on neuropsychiatric scores in elders with dementia and agitation. Br J Clin Pharmacol. 2016;3:784–92.
Ehrhardt S, Porsteinsson AP, Munro CA, Rosenberg PB, Pollock BG, Devanand DP, et al. Escitalopram for agitation in Alzheimer’s disease (S-CitAD): methods and design of an investigator-initiated, randomized, controlled, multicenter clinical trial. Alzheimers Dement. 2019;15(11):1427–36.
Herrmann N, Ruthirakuhan M, Gallagher D, Verhoeff NPLG, Kiss A, Black SE, et al. Randomized placebo-controlled trial of Nabilone for agitation in Alzheimer’s disease. Am J Geriatr Psychiatry. 2019;27(11):1161–73.
Ballard CG, Waite J, Birks J. Atypical antipsychotics for aggression and psychosis in Alzheimer’s disease. Cochrane Database Syst Rev. 2006
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011
van den Elsen GAH, Ahmed AIA, Verkes R-J, Kramers C, Feuth T, Rosenberg PB, et al. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: a randomized controlled trial. Neurology. 2015 Jun;84(23):2338–46.
Walther S, Mahlberg R, Eichmann U, Kunz D. Delta-9-tetrahydrocannabinol for nighttime agitation in severe dementia. Psychopharmacology. 2006;185(4):524–8.
Tampi RR, Joshi P, Marpuri P, Tampi DJ. Evidence for using dextromethorphan-quinidine for the treatment of agitation in dementia. World J Psychiatry. 2020;10(4):29–33.
Cummings JL, Lyketsos CG, Peskind ER, Porsteinsson AP, Mintzer JE, Scharre DW, et al. Effect of dextromethorphan-quinidine on agitation in patients with Alzheimer disease dementia a randomized clinical trial. JAMA - J Am Med Assoc. 2015;314(12):1242–54.
McDermott CL, Gruenewald DA. Pharmacologic Management of Agitation in patients with dementia. Curr Geriatr Reports. 2019;8(1):1–11.
Cummings J, Lai T-J, Hemrungrojn S, Mohandas E, Yun Kim S, Nair G, et al. Role of donepezil in the Management of Neuropsychiatric Symptoms in Alzheimer’s disease and dementia with Lewy bodies. CNS Neurosci Ther. 2016 Mar;22(3):159–66.
Cumbo E, Ligori LD. Differential effects of current specific treatments on behavioral and psychological symptoms in patients with Alzheimer’s disease: a 12-month, randomized, open-label trial. J Alzheimers Dis. 2014;39(3):477–85.
Gareri P, Putignano D, Castagna A, Cotroneo AM, De Palo G, Fabbo A, et al. Retrospective study on the benefits of combined Memantine and cholinEsterase inhibitor treatMent in AGEd patients affected with Alzheimer’s disease: the MEMAGE study. J Alzheimers Dis. 2014;41(2):633–40.
Davies SJC, Burhan AM, Kim D, Gerretsen P, Graff-Guerrero A, Woo VL, et al. Sequential drug treatment algorithm for agitation and aggression in Alzheimer’s and mixed dementia. J Psychopharmacol. 2018;32(5):509–23.
Maguire GA. Impact of antipsychotics on geriatric patients: efficacy, dosing, and compliance. Prim Care Companion J Clin Psychiatry. 2000 Oct;2(5):165–72.
Walaszek A. Behavioral and psychological symptoms of dementia. Washington: American Psychiatric Association Publishing; 2019.
Jacobson SA. Clinical manual of geriatric psychopharmacology. 2nd ed. Arlington: American Psychiatric Publishing; 2014.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Geriatric Psychiatry
Rights and permissions
About this article
Cite this article
Subramanian, S., Fahed, M., Dix, E. et al. Emergent and Non-Emergent Agitation in the Older Adult: Evaluation and Management. Curr Geri Rep 10, 73–81 (2021). https://doi.org/10.1007/s13670-021-00358-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-021-00358-6