Abstract
Purpose of Review
Agitation is common among older adults with dementia; its origin may be multi-factorial, and it is often difficult to treat. In this paper, we summarize current knowledge and offer considerations on pharmacologic management of behavioral and psychological symptoms of dementia (BPSD).
Recent Findings
We reviewed human studies published from 2013 to 2018 evaluating pharmacologic management of BPSD manifestations including depressive symptoms, mania, psychosis, and other BPSD, as well as severe agitation without determination of underlying cause. After non-pharmacological management is exhausted, the choice of pharmacological options depends on patient comorbidities, specific BPSD presentation, and patient tolerance of medications.
Summary
Depending on manifestations of BPSD, low- to moderate-quality evidence supports the use of anti-depressants, anti-psychotics, or anti-epileptics in conjunction with cholinesterase inhibitors. The current evidence base needs to be augmented with future research that focuses on real-world medication use alongside head-to-head evaluation of medication effectiveness rather than comparison to placebo.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Hebert LE, Weuve J, Scherr PA, Evans DA. Alzheimer disease in the United States (2010-2050) estimated using the 2010 census. Neurology. 2013;80(19):1778–83.
Derby CA, Katz MJ, Lipton RB, Hall CB. Trends in dementia incidence in a birth cohort analysis of the Einstein aging study. JAMA Neurol. 2017;74(11):1345–51.
Rocca WA, Petersen RC, Knopman DS, Hebert LE, Evans DA, Hall KS, et al. Trends in the incidence and prevalence of Alzheimer’s disease, dementia, and cognitive impairment in the United States. Alzheimers Dement. 2011;7(1):80–93.
van der Linde RM, Dening T, Stephan BC, Prina AM, Evans E, Brayne C. Longitudinal course of behavioural and psychological symptoms of dementia: systematic review. Br J Psychiatry. 2016;209(5):366–77.
Livingston G, Kelly L, Lewis-Holmes E, Baio G, Morris S, Patel N, et al. Non-pharmacological interventions for agitation in dementia: systematic review of randomised controlled trials. Br J Psychiatry. 2014;205(6):436–42.
de Oliveira AM, Radanovic M, de Mello PC, Buchain PC, Vizzotto AD, Celestino DL, et al. Nonpharmacological interventions to reduce behavioral and psychological symptoms of dementia: a systematic review. Biomed Res Int. 2015;2015:218980.
Brasure M, Jutkowitz E, Fuchs E, Nelson VA, Kane RA, Shippee T, et al. Nonpharmacologic interventions for agitation and aggression in dementia. Rockville (MD): AHRQ Comparative Effectiveness Reviews; 2016.
Maust DT, Kales HC, McCammon RJ, Blow FC, Leggett A, Langa KM. Distress associated with dementia-related psychosis and agitation in relation to healthcare utilization and costs. Am J Geriatr Psychiatry. 2017;25(10):1074–82.
Suehs BT, Shah SN, Davis CD, Alvir J, Faison WE, Patel NC, et al. Household members of persons with Alzheimer’s disease: health conditions, healthcare resource use, and healthcare costs. J Am Geriatr Soc. 2014;62(3):435–41.
Cummings JL, Geldmacher D, Farlow M, Sabbagh M, Christensen D, Betz P. High-dose donepezil (23 mg/day) for the treatment of moderate and severe Alzheimer’s disease: drug profile and clinical guidelines. CNS Neurosci Ther. 2013;19(5):294–301.
Cummings J, Lai TJ, Hemrungrojn S, Mohandas E, Yun Kim S, Nair G, et al. Role of donepezil in the management of neuropsychiatric symptoms in Alzheimer’s disease and dementia with Lewy bodies. CNS Neurosci Ther. 2016;22(3):159–66.
McKeith I, Del Ser T, Spano P, Emre M, Wesnes K, Anand R, et al. Efficacy of rivastigmine in dementia with Lewy bodies: a randomised, double-blind, placebo-controlled international study. Lancet. 2000;356(9247):2031–6.
Bohnen NI, Kaufer DI, Ivanco LS, Lopresti B, Koeppe RA, Davis JG, et al. Cortical cholinergic function is more severely affected in parkinsonian dementia than in Alzheimer disease: an in vivo positron emission tomographic study. Arch Neurol. 2003;60(12):1745–8.
Wang J, Yu JT, Wang HF, Meng XF, Wang C, Tan CC, et al. Pharmacological treatment of neuropsychiatric symptoms in Alzheimer’s disease: a systematic review and meta-analysis. J Neurol Neurosurg Psychiatry. 2015;86(1):101–9.
Cumbo E, Ligori LD. Differential effects of current specific treatments on behavioral and psychological symptoms in patients with Alzheimer’s disease: a 12-month, randomized, open-label trial. J Alzheimers Dis. 2014;39(3):477–85.
•• Carotenuto A, Rea R, Traini E, Fasanaro AM, Ricci G, Manzo V, et al. The effect of the association between donepezil and choline alphoscerate on behavioral disturbances in Alzheimer’s disease: interim results of the ASCOMALVA trial. J Alzheimers Dis. 2017;56(2):805–15 Interim results suggest addition of choline alphoscerate may result in reduced BPSD and decreased accompanying caregiver distress in patients with mild-moderate AD.
Gareri P, Putignano D, Castagna A, Cotroneo AM, De Palo G, Fabbo A, et al. Retrospective study on the benefits of combined memantine and cholinesterase inhibitor treatMent in AGEd patients affected with Alzheimer’s disease: the MEMAGE study. J Alzheimers Dis. 2014;41(2):633–40.
• Chen R, Chan PT, Chu H, Lin YC, Chang PC, Chen CY, et al. Treatment effects between monotherapy of donepezil versus combination with memantine for Alzheimer disease: a meta-analysis. PLoS One. 2017;12(8):e0183586 Analysis notes greater improvement in BPSD for patients with severe AD receiving combination therapy vs donepezil only.
Yoon SJ, Choi SH, Na HR, Park KW, Kim EJ, Han HJ, et al. Effects on agitation with rivastigmine patch monotherapy and combination therapy with memantine in mild to moderate Alzheimer’s disease: a multicenter 24-week prospective randomized open-label study (the Korean EXelon patch and combination with mEmantine comparative trial study). Geriatr Gerontol Int. 2017;17(3):494–9.
Manabe Y, Ino T, Yamanaka K, Kosaka K. Increased dosage of donepezil for the management of behavioural and psychological symptoms of dementia in dementia with Lewy bodies. Psychogeriatrics. 2016;16(3):202–8.
Seppala LJ, Wermelink A, de Vries M, Ploegmakers KJ, van de Glind EMM, Daams JG, et al. Fall-risk-increasing drugs: a systematic review and meta-analysis: II. Psychotropics. J Am Med Dir Assoc. 2018;19(4):371 e11–7.
Seitz DP, Adunuri N, Gill SS, Gruneir A, Herrmann N, Rochon P. Antidepressants for agitation and psychosis in dementia. Cochrane Database Syst Rev. 2011;2:CD008191.
•• Porsteinsson AP, Drye LT, Pollock BG, Devanand DP, Frangakis C, Ismail Z, et al. Effect of citalopram on agitation in Alzheimer disease: the CitAD randomized clinical trial. JAMA. 2014;311(7):682–91 RCT demonstrated efficacy of citalopram for management of BPSD.
Banerjee S, Hellier J, Romeo R, Dewey M, Knapp M, Ballard C, et al. Study of the use of antidepressants for depression in dementia: the HTA-SADD trial--a multicentre, randomised, double-blind, placebo-controlled trial of the clinical effectiveness and cost-effectiveness of sertraline and mirtazapine. Health Technol Assess. 2013;17(7):1–166.
Farina N, Morrell L, Banerjee S. What is the therapeutic value of antidepressants in dementia? A narrative review. Int J Geriatr Psychiatry. 2017;32(1):32–49.
Santa Cruz MR, Hidalgo PC, Lee MS, Thomas CW, Holroyd S. Buspirone for the treatment of dementia with behavioral disturbance. Int Psychogeriatr. 2017;29(5):859–62.
Mizukami K, Hatanaka K, Tanaka Y, Sato S, Asada T. Therapeutic effects of the selective serotonin noradrenaline reuptake inhibitor milnacipran on depressive symptoms in patients with Alzheimer’s disease. Prog Neuro-Psychopharmacol Biol Psychiatry. 2009;33(2):349–52.
Mokhber N, Abdollahian E, Soltanifar A, Samadi R, Saghebi A, Haghighi MB, et al. Comparison of sertraline, venlafaxine and desipramine effects on depression, cognition and the daily living activities in Alzheimer patients. Pharmacopsychiatry. 2014;47(4–5):131–40.
Lin CP, Chu CP, Liu HC. Bupropion improved apathy in behavioral variant frontotemporal dementia: a case report. Neurocase. 2016;22(5):466–8.
Martinon-Torres G, Fioravanti M, Grimley EJ. Trazodone for agitation in dementia. Cochrane Database Syst Rev. 2004;4:CD004990.
Camargos EF, Louzada LL, Quintas JL, Naves JO, Louzada FM, Nobrega OT. Trazodone improves sleep parameters in Alzheimer disease patients: a randomized, double-blind, and placebo-controlled study. Am J Geriatr Psychiatry. 2014;22(12):1565–74.
Tampi RR, Tampi DJ. Efficacy and tolerability of benzodiazepines for the treatment of behavioral and psychological symptoms of dementia: a systematic review of randomized controlled trials. Am J Alzheimers Dis Other Demen. 2014;29(7):565–74.
Defrancesco M, Marksteiner J, Fleischhacker WW, Blasko I. Use of benzodiazepines in Alzheimer’s disease: a systematic review of literature. Int J Neuropsychopharmacol. 2015;18(10):pyv055.
Tampi RR, Tampi DJ, Balachandran S, Srinivasan S. Antipsychotic use in dementia: a systematic review of benefits and risks from meta-analyses. Ther Adv Chronic Dis. 2016;7(5):229–45.
Kane JM, Correll CU, Nierenberg AA, Caroff SN, Sajatovic M, Tardive Dyskinesia Assessment Working G. Revisiting the Abnormal Involuntary Movement Scale: Proceedings From the Tardive Dyskinesia Assessment Workshop. J Clin Psychiatry. 2018;79(3).
Van Leeuwen E, Petrovic M, van Driel ML, De Sutter AI, Vander Stichele R, Declercq T, et al. Withdrawal versus continuation of long-term antipsychotic drug use for behavioural and psychological symptoms in older people with dementia. Cochrane Database Syst Rev. 2018;3:CD007726.
• Tjia J, Reidenberg MM, Hunnicutt JN, Paice K, Donovan JL, Kanaan A, et al. Approaches to gradual dose reduction of chronic off-label antipsychotics used for behavioral and psychological symptoms of dementia. Consult Pharm. 2015;30(10):599–611 Synthesizes data supporting proposed de-prescribing algorithm for patients receiving anti-psychotics.
Mathys M, Fang S, John J, Carter J. Antipsychotic discontinuation after the initiation of selective serotonin reuptake inhibitors therapy for the treatment of behavioral and psychological symptoms associated with dementia. Ment Health Clin. 2018;8(3):122–6.
•• Brodaty H, Aerts L, Harrison F, Jessop T, Cations M, Chenoweth L, et al. Antipsychotic deprescription for older adults in long-term care: the HALT study. J Am Med Dir Assoc. 2018;19(7):592–600 e7 Demonstrated that anti-psychotics may be safely withdrawn without increase in BPSD or adverse outcomes.
Tariot PN, Schneider LS, Cummings J, Thomas RG, Raman R, Jakimovich LJ, et al. Chronic divalproex sodium to attenuate agitation and clinical progression of Alzheimer disease. Arch Gen Psychiatry. 2011;68(8):853–61.
Lonergan E, Luxenberg J. Valproate preparations for agitation in dementia. Cochrane Database Syst Rev. 2009;3:CD003945.
Gallagher D, Herrmann N. Antiepileptic drugs for the treatment of agitation and aggression in dementia: do they have a place in therapy? Drugs. 2014;74(15):1747–55.
Suzuki H, Gen K. Clinical efficacy of lamotrigine and changes in the dosages of concomitantly used psychotropic drugs in Alzheimer’s disease with behavioural and psychological symptoms of dementia: a preliminary open-label trial. Psychogeriatrics. 2015;15(1):32–7.
Cooney C, Murphy S, Tessema H, Freyne A. Use of low-dose gabapentin for aggressive behavior in vascular and mixed vascular/Alzheimer dementia. J Neuropsychiatry Clin Neurosci. 2013;25(2):120–5.
•• Cummings JL, Lyketsos CG, Peskind ER, Porsteinsson AP, Mintzer JE, Scharre DW, et al. Effect of dextromethorphan-quinidine on agitation in patients with alzheimer disease dementia: a randomized clinical trial. JAMA. 2015;314(12):1242–54 In short-term 10 week trial, authors found reduced agitation among AD patients taking dextromethorphan-quinidine.
Tampi RR, Hassell C, Joshi P, Tampi DJ. Analgesics in the management of behavioral and psychological symptoms of dementia: a perspective review. Drugs Context. 2017;6:212508.
Habiger TF, Flo E, Achterberg WP, Husebo BS. The interactive relationship between pain, psychosis, and agitation in people with dementia: results from a cluster-randomised clinical trial. Behav Neurol. 2016;2016:7036415.
Devanand DP, Strickler JG, Huey ED, Crocco E, Forester BP, Husain MM, et al. Lithium treatment for agitation in Alzheimer’s disease (lit-AD): clinical rationale and study design. Contemp Clin Trials. 2018;71:33–9.
Carr CN, Straley CM, Baugh TB. Allopurinol for the treatment of refractory aggression: a case series. Pharmacotherapy. 2017;37(6):748–54.
Wade AG, Farmer M, Harari G, Fund N, Laudon M, Nir T, et al. Add-on prolonged-release melatonin for cognitive function and sleep in mild to moderate Alzheimer’s disease: a 6-month, randomized, placebo-controlled, multicenter trial. Clin Interv Aging. 2014;9:947–61.
Schroeck JL, Ford J, Conway EL, Kurtzhalts KE, Gee ME, Vollmer KA, et al. Review of safety and efficacy of sleep medicines in older adults. Clin Ther. 2016;38(11):2340–72.
McCleery J, Cohen DA, Sharpley AL. Pharmacotherapies for sleep disturbances in dementia. Cochrane Database Syst Rev. 2016;11:CD009178.
Butchart J, Brook L, Hopkins V, Teeling J, Puntener U, Culliford D, et al. Etanercept in Alzheimer disease: a randomized, placebo-controlled, double-blind, phase 2 trial. Neurology. 2015;84(21):2161–8.
De Giorgi R, Series H. Treatment of inappropriate sexual behavior in dementia. Curr Treat Options Neurol. 2016;18(9):41.
Quill TE, Lo B, Brock DW, Meisel A. Last-resort options for palliative sedation. Ann Intern Med. 2009;151(6):421–4.
Hendriks SA, Smalbrugge M, Hertogh CM, van der Steen JT. Dying with dementia: symptoms, treatment, and quality of life in the last week of life. J Pain Symptom Manag. 2014;47(4):710–20.
Benitez-Rosario MA, Morita T. Palliative sedation in clinical scenarios: results of a modified Delphi study. Support Care Cancer. 2018.
Cherny NI, Group EGW. ESMO Clinical Practice Guidelines for the management of refractory symptoms at the end of life and the use of palliative sedation. Ann Oncol. 2014;25(Suppl 3):iii143–52.
Gurschick L, Mayer DK, Hanson LC. Palliative sedation: an analysis of international guidelines and position statements. Am J Hosp Palliat Care. 2015;32(6):660–71.
Bodnar J. A review of agents for palliative sedation/continuous deep sedation: pharmacology and practical applications. J Pain Palliat Care Pharmacother. 2017;31(1):16–37.
van den Elsen GA, Ahmed AI, Verkes RJ, Kramers C, Feuth T, Rosenberg PB, et al. Tetrahydrocannabinol for neuropsychiatric symptoms in dementia: a randomized controlled trial. Neurology. 2015;84(23):2338–46.
Savaskan E, Mueller H, Hoerr R, von Gunten A, Gauthier S. Treatment effects of Ginkgo biloba extract EGb 761(R) on the spectrum of behavioral and psychological symptoms of dementia: meta-analysis of randomized controlled trials. Int Psychogeriatr. 2018;30(3):285–93.
Fu CY, Moyle W, Cooke M. A randomised controlled trial of the use of aromatherapy and hand massage to reduce disruptive behaviour in people with dementia. BMC Complement Altern Med. 2013;13:165.
Yoshiyama K, Arita H, Suzuki J. The effect of aroma hand massage therapy for people with dementia. J Altern Complement Med. 2015;21(12):759–65.
O’Connor DW, Eppingstall B, Taffe J, van der Ploeg ES. A randomized, controlled cross-over trial of dermally-applied lavender (Lavandula angustifolia) oil as a treatment of agitated behaviour in dementia. BMC Complement Altern Med. 2013;13:315.
Yang MH, Lin LC, Wu SC, Chiu JH, Wang PN, Lin JG. Comparison of the efficacy of aroma-acupressure and aromatherapy for the treatment of dementia-associated agitation. BMC Complement Altern Med. 2015;15:93.
Furukawa K, Tomita N, Uematsu D, Okahara K, Shimada H, Ikeda M, et al. Randomized double-blind placebo-controlled multicenter trial of Yokukansan for neuropsychiatric symptoms in Alzheimer’s disease. Geriatr Gerontol Int. 2017;17(2):211–8.
Teranishi M, Kurita M, Nishino S, Takeyoshi K, Numata Y, Sato T, et al. Efficacy and tolerability of risperidone, yokukansan, and fluvoxamine for the treatment of behavioral and psychological symptoms of dementia: a blinded, randomized trial. J Clin Psychopharmacol. 2013;33(5):600–7.
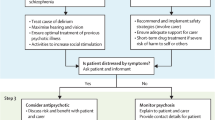
• Davies SJ, Burhan AM, Kim D, Gerretsen P, Graff-Guerrero A, Woo VL, et al. Sequential drug treatment algorithm for agitation and aggression in Alzheimer’s and mixed dementia. J Psychopharmacol. 2018;32(5):509–23 Proposes treatment algorithm for BPSD, considering various manifestations of BPSD.
• Kales HC, Lyketsos CG, Miller EM, Ballard C. Management of behavioral and psychological symptoms in people with Alzheimer’s disease: an international Delphi consensus. Int Psychogeriatr. 2018;1–8. Expert consensus regarding treatment considerations for BPSD.
Soto M, Andrieu S, Nourhashemi F, Ousset PJ, Ballard C, Robert P, et al. Medication development for agitation and aggression in Alzheimer disease: review and discussion of recent randomized clinical trial design. Int Psychogeriatr. 2014:1–17.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Cara McDermott and David Gruenewald declare no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclosure
The contents of this article do not represent the views of the US Department of Veterans Affairs or the US Government.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Palliative Care
Rights and permissions
About this article
Cite this article
McDermott, C.L., Gruenewald, D.A. Pharmacologic Management of Agitation in Patients with Dementia. Curr Geri Rep 8, 1–11 (2019). https://doi.org/10.1007/s13670-019-0269-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13670-019-0269-1