Abstract
Purpose of Review
Anti-Müllerian hormone (AMH) is secreted by ovarian granulosa cells and has become a surrogate marker for ovarian reserve. We review anticipated AMH levels throughout the reproductive lifespan and how AMH levels can be used in assisted reproductive technology.
Recent Findings
While AMH is a surrogate marker for ovarian reserve, values do not predict fertility. Patients with low versus normal AMH have similar fertility. AMH levels are helpful in guiding treatment for infertility, including medication dosing for IVF and anticipated cycle outcomes. AMH levels are positively correlated with ovarian response in IVF cycles. For cancer patients with planned gonadotoxic chemotherapy, AMH levels are useful in counseling patients prior to treatment, recommending fertility preservation options, and monitoring ovarian function following treatment. New studies have shown a possible protective effect of AMH injection on the ovaries for women undergoing gonadotoxic chemotherapy treatment. AMH levels are a useful adjunct to follicle-stimulating hormone (FSH) levels when diagnosing menopause and premature ovarian insufficiency (POI) and can be used to estimate the menopausal transition in women above the age of 40 but have limited clinical utility in predicting menopause for women at risk for POI.
Summary
AMH is a useful tool to assess ovarian reserve and response to ovarian stimulation, but levels are not correlated with rates of conception and should not be used to counsel on spontaneous fertility. While AMH can be used as a quantitative measure of ovarian reserve, AMH level is not a qualitative marker for oocytes. AMH injection may be a therapeutic option for fertility preservation in the future.




Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
•• Of major importance
Munsterberg A, Lovell-Badge R. Expression of the mouse anti-mullerian hormone gene suggests a role in both male and female sexual differentiation. Development. 1991;113.
Rajpert-De Meyts E, Jørgensen N, Græm N, Müller J, Cate RL, Skakkebæk NE. Expression of anti-Müllerian hormone during normal and pathological gonadal development: association with differentiation of sertoli and granulosa cells 1 . J Clin Endocrinol Metab [Internet]. The Endocrine Society; 1999 [cited 2021 Apr 7];84:3836–44. Available from: https://pubmed.ncbi.nlm.nih.gov/10523039/.
Weenen C, Laven JSE, von Bergh ARM, Cranfield M, Groome NP, Visser JA, et al. Anti-Müllerian hormone expression pattern in the human ovary: potential implications for initial and cyclic follicle recruitment. Mol Hum Reprod [Internet]. Mol Hum Reprod; 2004 [cited 2021 Apr 7];10:77–83. Available from: https://pubmed.ncbi.nlm.nih.gov/14742691/.
Salmon NA, Handyside AH, Joyce IM. Oocyte regulation of anti-Müllerian hormone expression in granulosa cells during ovarian follicle development in mice. Dev Biol [Internet]. Academic Press Inc.; 2004 [cited 2021 Apr 7];266:201–8. Available from: https://pubmed.ncbi.nlm.nih.gov/14729489/.
• La Marca A, Stabile G, Carducci Artenisio A, Volpe A. Serum anti-Mullerian hormone throughout the human menstrual cycle. Hum Reprod [Internet]. Oxford University Press; 2006 [cited 2021 May 5];21:3103–7. Available from: https://pubmed.ncbi.nlm.nih.gov/16923748/. This study clarified anticipated AMH values for women with PCOS, hypothalmic hypogonadism and premature ovarian insufficiency compared to controls. These data help define the conditions and aid in patient counseling.
Nelson SM, Marca L. The journey from the old to the new AMH assay: how to avoid getting lost in the values.
Bonifacio M, Bradley CK, Karia S, Livingstone M, Bowman MC, McArthur SJ. The original Beckman Coulter Generation II assay significantly underestimates AMH levels compared with the revised protocol. J Assist Reprod Genet [Internet]. Springer New York LLC; 2015 [cited 2021 May 5];32:1691–6. Available from: https://link.springer.com/. https://doi.org/10.1007/s10815-015-0579-y.
Gassner D, Jung R. First fully automated immunoassay for anti-Müllerian hormone. Clin Chem Lab Med [Internet]. Walter de Gruyter GmbH; 2014 [cited 2021 May 5];52:1143–52. Available from: https://pubmed.ncbi.nlm.nih.gov/24622790/.
Demirdjian G, Bord S, Lejeune C, Masica R, Rivière D, Nicouleau L, et al. Performance characteristics of the Access AMH assay for the quantitative determination of anti-Müllerian hormone (AMH) levels on the Access* family of automated immunoassay systems. Clin Biochem [Internet]. Elsevier Inc.; 2016 [cited 2021 May 5];49:1267–73. Available from: https://pubmed.ncbi.nlm.nih.gov/27542330/.
Van Helden J, Weiskirchen R. Performance of the two new fully automated anti-Müllerian hormone immunoassays compared with the clinical standard assay. Hum Reprod [Internet]. Oxford University Press; 2015 [cited 2021 May 5];30:1918–26. Available from: https://pubmed.ncbi.nlm.nih.gov/26093541/.
Anckaert E, Öktem M, Thies A, Cohen-Bacrie M, Daan NMP, Schiettecatte J, et al. Multicenter analytical performance evaluation of a fully automated anti-Müllerian hormone assay and reference interval determination. Clin Biochem [Internet]. Elsevier Inc.; 2016 [cited 2021 May 5];49:260–7. Available from: https://pubmed.ncbi.nlm.nih.gov/26500002/.
Nelson SM, Pastuszek E, Kloss G, Malinowska I, Liss J, Lukaszuk A, et al. Two new automated, compared with two enzyme-linked immunosorbent, antimüllerian hormone assays. Fertil Steril [Internet]. Elsevier Inc.; 2015 [cited 2021 May 5];104:1016–1021.e6. Available from: https://pubmed.ncbi.nlm.nih.gov/26183313/.
Cui Y, Shi Y, Cui L, Han T, Gao X, Chen ZJ. Age-specific serum antimüllerian hormone levels in women with and without polycystic ovary syndrome. Fertil Steril [Internet]. Elsevier Inc.; 2014 [cited 2021 May 5];102. Available from: https://pubmed.ncbi.nlm.nih.gov/24746743/.
• Nelson SM, Messow MC, Wallace AM, Fleming R, McConnachie A. Nomogram for the decline in serum antimüllerian hormone: a population study of 9,601 infertility patients. Fertil Steril [Internet]. Elsevier Inc.; 2011 [cited 2021 May 5];95. Available from: https://pubmed.ncbi.nlm.nih.gov/20869051/. This study identified a nomogram for AMH values by age, which is used for patient counseling and to guide treatment recommendations. The lab assay used has been validated in multiple studies.
Nelson SM, Messow MC, Mcconnachie A, Wallace H, Kelsey T, Fleming R, et al. External validation of nomogram for the decline in serum anti-Müllerian hormone in women: a population study of 15,834 infertility patients.
• Lie Fong S, Visser JA, Welt CK, De Rijke YB, Eijkemans MJC, Broekmans FJ, et al. Serum anti-müllerian hormone levels in healthy females: a nomogram ranging from infancy to adulthood. J Clin Endocrinol Metab [Internet]. Oxford Academic; 2012 [cited 2021 May 5];97:4650–5. Available from: https://academic.oup.com/jcem/article/97/12/4650/2536586. This study plotted a nomogram for AMH values that included childhood and adolscents, improving our understanding of anticipated levels by age.
La Marca A, Pati M, Orvieto R, Stabile G, Carducci Artenisio A, Volpe A. Serum anti-Müllerian hormone levels in women with secondary amenorrhea. Fertil Steril [Internet]. Fertil Steril; 2006 [cited 2021 May 5];85:1547–9. Available from: https://pubmed.ncbi.nlm.nih.gov/16616745/.
Birch Petersen K, Hvidman HW, Forman JL, Pinborg A, Larsen EC, Macklon KT, et al. Ovarian reserve assessment in users of oral contraception seeking fertility advice on their reproductive lifespan. Hum Reprod [Internet]. Oxford University Press; 2015 [cited 2021 May 16];30:2364–75. Available from: https://pubmed.ncbi.nlm.nih.gov/26311148/.
Van Den Berg MH, Van Dulmen-Den Broeder E, Overbeek A, Twisk JWR, Schats R, Van Leeuwen FE, et al. Comparison of ovarian function markers in users of hormonal contraceptives during the hormone-free interval and subsequent natural early follicular phases. Hum Reprod [Internet]. Oxford University Press; 2010 [cited 2021 May 16];25:1520–7. Available from: https://academic.oup.com/humrep/article/25/6/1520/2915768.
•• Hariton E, Shirazi T, Douglas N, Hershlag A, Briggs S. Anti-Müllerian hormone levels among contraceptive users: evidence from a cross-sectional cohort of 27,125 individuals. Am J Obstet Gynecol [Internet]. Am J Obstet Gynecol; 2021 [cited 2021 Aug 20]; Available from: https://pubmed.ncbi.nlm.nih.gov/34126087/. Mean AMH levels are significantly lower in women using the combined oral contraceptive pill (23.68% lower), vaginal ring (22.07% lower), hormonal intrauterine device (6.73% lower), implant (23.44% lower), and progestin-only pill (14.80% lower) than women not on any contraceptive.
Su HI, Maas K, Sluss PM, Chang RJ, Hall JE, Joffe H. The impact of depot GnRH agonist on AMH levels in healthy reproductive-aged women. J Clin Endocrinol Metab [Internet]. The Endocrine Society; 2013 [cited 2021 Aug 20];98:E1961. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3849679/.
•• Wang Y, Yuan Y, Meng D, Liu X, Gao Y, Wang F, et al. Effects of environmental, social and surgical factors on ovarian reserve: implications for age-relative female fertility. Int J Gynecol Obstet [Internet]. John Wiley and Sons Ltd; 2021 [cited 2021 May 15]; Available from: https://pubmed.ncbi.nlm.nih.gov/33569772/. Alcohol use and smoking lower AMH levels, whereas caffeine does not.
Freour T, Masson D, Mirallie S, Jean M, Bach K, Dejoie T, et al. Active smoking compromises IVF outcome and affects ovarian reserve. Reprod Biomed Online [Internet]. Reproductive Healthcare Ltd; 2008 [cited 2021 May 15];16:96–102. Available from: https://pubmed.ncbi.nlm.nih.gov/18252054/.
•• Simões-Pereira J, Nunes J, Aguiar A, Sousa S, Rodrigues C, Sampaio Matias J, et al. Influence of body mass index in anti-Müllerian hormone levels in 951 non-polycystic ovarian syndrome women followed at a reproductive medicine unit. Endocrine [Internet]. Humana Press Inc.; 2018 [cited 2021 May 5];61:144–8. Available from: https://pubmed.ncbi.nlm.nih.gov/29470775/. AMH values are inversely correlated with BMI in women with PCOS.
Vagios S, James KE, Sacha CR, Hsu JY, Dimitriadis I, Bormann CL, et al. A patient-specific model combining antimüllerian hormone and body mass index as a predictor of polycystic ovary syndrome and other oligo-anovulation disorders. Fertil Steril [Internet]. Elsevier Inc.; 2021 [cited 2021 May 5];115:229–37. Available from: https://pubmed.ncbi.nlm.nih.gov/33077236/.
Pitts S, Dahlberg SE, Gallagher JS, Gordon CM, DiVasta AD. Is ovarian reserve impacted in anorexia nervosa? J Pediatr Adolesc Gynecol [Internet]. Elsevier Inc.; 2021 [cited 2021 May 15]. p. 196–202. Available from: https://pubmed.ncbi.nlm.nih.gov/33278562/.
Pedachenko N, Anagnostis P, Shemelko T, Tukhtarian R, Alabbas L. Serum anti-Mullerian hormone, prolactin and estradiol concentrations in infertile women with endometriosis. Gynecol Endocrinol [Internet]. Taylor and Francis Ltd.; 2021 [cited 2021 May 15];37:162–5. Available from: https://pubmed.ncbi.nlm.nih.gov/33274686/.
Hwu YM, Wu FS, Li SH, Sun FJ, Lin MH, Lee RK. The impact of endometrioma and laparoscopic cystectomy on serum anti-Müllerian hormone levels. Reprod Biol Endocrinol [Internet]. Reprod Biol Endocrinol; 2011 [cited 2021 May 15];9. Available from: https://pubmed.ncbi.nlm.nih.gov/21651823/.
Steiner AZ, Pritchard D, Stanczyk FZ, Kesner JS, Meadows JW, Herring AH, et al. Association between biomarkers of ovarian reserve and infertility among older women of reproductive age. JAMA - J Am Med Assoc [Internet]. American Medical Association; 2017 [cited 2021 May 16];318:1367–76. Available from: https://jamanetwork.com/.
•• Zarek SM, Mitchell EM, Sjaarda LA, Mumford SL, Silver RM, Stanford JB, et al. Is anti-Müllerian hormone associated with fecundability? Findings from the EAGeR trial. J Clin Endocrinol Metab [Internet]. Endocrine Society; 2015 [cited 2021 May 15];100:4215–21. Available from: https://pubmed.ncbi.nlm.nih.gov/26406293/. AMH is a poor predictor fecundidy.
Depmann M, Broer SL, Eijkemans MJC, van Rooij IAJ, Scheffer GJ, Heimensem J, et al. Anti-Müllerian hormone does not predict time to pregnancy: results of a prospective cohort study. Gynecol Endocrinol [Internet]. Taylor and Francis Ltd; 2017 [cited 2021 May 15];33:644–8. Available from: https://pubmed.ncbi.nlm.nih.gov/28393651/.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril [Internet]. Elsevier Inc.; 2004 [cited 2021 May 15];81:19–25. Available from: https://pubmed.ncbi.nlm.nih.gov/14711538/.
Eilertsen TB, Vanky E, Carlsen SM. Anti-Mullerian hormone in the diagnosis of polycystic ovary syndrome: can morphologic description be replaced. Hum Reprod [Internet]. Oxford University Press; 2012 [cited 2021 May 16];27:2494–502. Available from: https://pubmed.ncbi.nlm.nih.gov/22693172/.
Lauritsen MP, Bentzen JG, Pinborg A, Loft A, Forman JL, Thuesen LL, et al. The prevalence of polycystic ovary syndrome in a normal population according to the Rotterdam criteria versus revised criteria including anti-Müllerian hormone. Hum Reprod [Internet]. Oxford University Press; 2014 [cited 2021 May 16];29:791–801. Available from: https://pubmed.ncbi.nlm.nih.gov/24435776/.
Mumford SL, Legro RS, Diamond MP, Coutifaris C, Steiner AZ, Schlaff WD, et al. Baseline AMH level associated with ovulation following ovulation induction in women with polycystic ovary syndrome. J Clin Endocrinol Metab [Internet]. Endocrine Society; 2016 [cited 2021 May 15]. p. 3288–96. Available from: https://pubmed.ncbi.nlm.nih.gov/27228369/.
Coskun B, Dilbaz B, Karadag B, Coskun B, Tohma YA, Dur R, et al. The role of anti-Mullerian hormone in predicting the response to clomiphene citrate in unexplained infertility. Taiwan J Obstet Gynecol Elsevier Ltd. 2018;57:713–7.
Hansen KR, He ALW, Styer AK, Wild RA, Butts S, Engmann L, et al. Predictors of pregnancy and live-birth in couples with unexplained infertility after ovarian stimulation–intrauterine insemination. Fertil Steril [Internet]. Elsevier Inc.; 2016 [cited 2021 May 15]. p. 1575–1583.e2. Available from: https://pubmed.ncbi.nlm.nih.gov/26949110/.
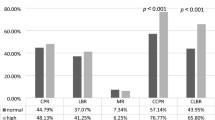
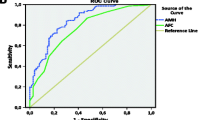
Broer SL, Dólleman M, Opmeer BC, Fauser BC, Mol BW, Broekmans FJM. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta-analysis. Hum Reprod Update [Internet]. Oxford University Press; 2011 [cited 2021 May 15];17:46–54. Available from: https://academic.oup.com/humupd/article/17/1/46/639734.
Elgindy EA, El-Haieg DO, El-Sebaey A. Anti-Müllerian hormone: correlation of early follicular, ovulatory and midluteal levels with ovarian response and cycle outcome in intracytoplasmic sperm injection patients. Fertil Steril [Internet]. Fertil Steril; 2008 [cited 2021 May 15];89:1670–6. Available from: https://pubmed.ncbi.nlm.nih.gov/17658520/.
•• Baker VL, Glassner MJ, Doody K, Schnell VL, Gracia C, Shin SS, et al. Validation study of the Access AMH antimüllerian hormone assay for the prediction of poor ovarian response to controlled ovarian stimulation. Fertil Steril [Internet]. Elsevier Inc.; 2021 [cited 2021 May 15]; Available from: https://pubmed.ncbi.nlm.nih.gov/33812650/. In IVF cycles, the mean AMH level for poor responders as 0.99 ng/ml compared to a mean AMH of 2.83 ng/ml in normal to high responders.
Andersen AN, Witjes H, Gordon K, Mannaerts B. Predictive factors of ovarian response and clinical outcome after IVF/ICSI following a rFSH/GnRH antagonist protocol with or without oral contraceptive pre-treatment. Hum Reprod [Internet]. Oxford University Press; 2011 [cited 2021 May 16];26:3413–23. Available from: https://academic.oup.com/humrep/article/26/12/3413/2914030.
Nelson SM, Klein BM, Arce JC. Comparison of antimüllerian hormone levels and antral follicle count as predictor of ovarian response to controlled ovarian stimulation in good-prognosis patients at individual fertility clinics in two multicenter trials. Fertil Steril [Internet]. Elsevier Inc.; 2015 [cited 2021 May 16];103:923–930.e1. Available from: https://pubmed.ncbi.nlm.nih.gov/25624196/.
Broer SL, Dólleman M, Van Disseldorp J, Broeze KA, Opmeer BC, Bossuyt PMM, et al. Prediction of an excessive response in in vitro fertilization from patient characteristics and ovarian reserve tests and comparison in subgroups: an individual patient data meta-analysis. Fertil Steril [Internet]. Elsevier Inc.; 2013 [cited 2021 May 16];100:420–429.e7. Available from: https://pubmed.ncbi.nlm.nih.gov/23721718/.
Broer SL, van Disseldorp J, Broeze KA, Dolleman M, Opmeer BC, Bossuyt P, et al. Added value of ovarian reserve testing on patient characteristics in the prediction of ovarian response and ongoing pregnancy: an individual patient data approach. Hum Reprod Update [Internet]. Oxford Academic; 2013 [cited 2021 May 16];19:26–36. Available from: https://academic.oup.com/humupd/article/19/1/26/629243.
Asada Y, Tsuiki M, Sonohara M, Fukunaga N, Hattori Y, Inoue D, et al. Performance of anti-Müllerian hormone (AMH) levels measured by Beckman Coulter Access AMH assay to predict oocyte yield following controlled ovarian stimulation for in vitro fertilization. Reprod Med Biol [Internet]. John Wiley and Sons Ltd; 2019 [cited 2021 May 15];18:273–7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6613014/.
Penzias A, Azziz R, Bendikson K, Falcone T, Hansen K, Hill M, et al. Testing and interpreting measures of ovarian reserve: a committee opinion. Fertil Steril [Internet]. Elsevier Inc.; 2020 [cited 2021 May 16];114:1151–7. Available from: https://pubmed.ncbi.nlm.nih.gov/33280722/.
Bedoschi G, Navarro PA, Oktay K. Chemotherapy-induced damage to ovary: mechanisms and clinical impact [Internet]. Futur. Oncol. Future Medicine Ltd.; 2016 [cited 2021 May 16]. p. 2333–44. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5066134/.
•• Berjeb KK, Debbabi L, Braham M, Zemni Z, Chtourou S, Hannachi H, et al. Evaluation of ovarian reserve before and after chemotherapy. J Gynecol Obstet Hum Reprod [Internet]. Elsevier Masson s.r.l.; 2021 [cited 2021 May 16];50. Available from: https://pubmed.ncbi.nlm.nih.gov/33307239/. The degree of ovarian damage caused by chemotherpay depends on patient age, AMH, and dose and type of chemotherapy agent.
•• Goldfarb SB, Turan V, Bedoschi G, Taylan E, Abdo N, Cigler T, et al. Impact of adjuvant chemotherapy or tamoxifen-alone on the ovarian reserve of young women with breast cancer. Breast Cancer Res Treat [Internet]. Springer; 2021 [cited 2021 May 16];185:165–73. Available from: https://pubmed.ncbi.nlm.nih.gov/32930927/. Tamoxifen treatment alone for breast cancer does not impact ovarian reserve.
Lekovich J, Lobel ALS, Stewart JD, Pereira N, Kligman I, Rosenwaks Z. Female patients with lymphoma demonstrate diminished ovarian reserve even before initiation of chemotherapy when compared with healthy controls and patients with other malignancies. J Assist Reprod Genet [Internet]. Springer New York LLC; 2016 [cited 2021 May 16];33:657–62. Available from: https://pubmed.ncbi.nlm.nih.gov/26943918/.
Yu B, Douglas N, Ferin MJ, Nakhuda GS, Crew K, Lobo RA, et al. Changes in markers of ovarian reserve and endocrine function in young women with breast cancer undergoing adjuvant chemotherapy. Cancer [Internet]. Cancer; 2010 [cited 2021 May 16];116:2099–105. Available from: https://pubmed.ncbi.nlm.nih.gov/20187091/.
Anderson RA, Rosendahl M, Kelsey TW, Cameron DA. Pretreatment anti-Müllerian hormone predicts for loss of ovarian function after chemotherapy for early breast cancer. Eur J Cancer [Internet]. Elsevier; 2013 [cited 2021 May 16];49:3404–11. Available from: /pmc/articles/PMC3807650/.
Dillon KE, Sammel MD, Prewitt M, Ginsberg JP, Walker D, Mersereau JE, et al. Pretreatment antimüllerian hormone levels determine rate of posttherapy ovarian reserve recovery: acute changes in ovarian reserve during and after chemotherapy. Fertil Steril [Internet]. Elsevier Inc.; 2013 [cited 2021 May 16];99. Available from: https://pubmed.ncbi.nlm.nih.gov/23084267/.
•• Loubersac S, Dezellus A, Lefebvre T, Reignier A, Barriere P, Masson D, et al. Evolution of serum anti-Müllerian Hormone (AMH) level in young women treated with chemotherapy for breast cancer according to basal AMH level. Eur J Obstet Gynecol Reprod Biol [Internet]. Elsevier Ireland Ltd; 2020 [cited 2021 May 16];254:132–7. Available from: https://pubmed.ncbi.nlm.nih.gov/32971432/. Higher pre-treatment AMH levels are also associated with more rapid recovery of ovarian function.
Irene Su H, Kwan B, Whitcomb BW, Shliakhsitsava K, Dietz AC, Stark SS, et al. Modeling variation in the reproductive lifespan of female adolescent and young adult cancer survivors using AMH. J Clin Endocrinol Metab [Internet]. Endocrine Society; 2020 [cited 2021 May 16];105:2740–51. Available from: https://pubmed.ncbi.nlm.nih.gov/32270202/.
Cameron K, Sammel MD, Prewitt M, Gracia C. Differential rates of change in measures of ovarian reserve in young cancer survivors across the reproductive lifespan. J Clin Endocrinol Metab [Internet]. Oxford University Press; 2019 [cited 2021 May 16];104:1813–22. Available from: https://pubmed.ncbi.nlm.nih.gov/30566616/.
•• Morin SJ, Patounakis G, Juneau CR, Neal SA, Scott RT, Seli E. Diminished ovarian reserve and poor response to stimulation in patients <38 years old: a quantitative but not qualitative reduction in performance. Hum Reprod [Internet]. Oxford University Press; 2018 [cited 2021 Jan 13];33:1489–98. Available from: https://pubmed.ncbi.nlm.nih.gov/30010882/. AMH levels do not independently correlate with oocyte quality; age is the most predictive factor for euploidy.
Lee S, Ozkavukcu S, Heytens E, Moy F, Alappat RM, Oktay K. Anti-Mullerian hormone and antral follicle count as predictors for embryo/oocyte cryopreservation cycle outcomes in breast cancer patients stimulated with letrozole and follicle stimulating hormone. J Assist Reprod Genet [Internet]. J Assist Reprod Genet; 2011 [cited 2021 May 16];28:651–6. Available from: https://pubmed.ncbi.nlm.nih.gov/21573682/.
•• Turan V, Quinn MM, Dayioglu N, Rosen MP, Oktay K. The impact of malignancy on response to ovarian stimulation for fertility preservation: a meta-analysis. Fertil Steril [Internet]. Elsevier Inc.; 2018 [cited 2021 May 16];110:1347–55. Available from: https://pubmed.ncbi.nlm.nih.gov/30503134/. Patients with cancer have a similar response to ovarian stimulation in IVF cycles as patients without cancer.
•• Brun T, Dion L, Jaillard S, Bales D, Domin M, Lavoué V, et al. Ovarian response to stimulation for fertility preservation in women with hematologic cancer. J Gynecol Obstet Hum Reprod [Internet]. Elsevier Masson s.r.l.; 2021 [cited 2021 May 16];50. Available from: https://pubmed.ncbi.nlm.nih.gov/33010467/. Patients with cancer have a similar response to ovarian stimulation in IVF cycles as patients without cancer.
Phillips KA, Collins IM, Milne RL, McLachlan SA, Friedlander M, Hickey M, et al. Anti-Müllerian hormone serum concentrations of women with germline BRCA1 or BRCA2 mutations. Hum Reprod [Internet]. Oxford University Press; 2016 [cited 2021 May 16];31:1126–32. Available from: https://pubmed.ncbi.nlm.nih.gov/27094481/.
Derks-Smeets IAP, van Tilborg TC, van Montfoort A, Smits L, Torrance HL, Meijer-Hoogeveen M, et al. BRCA1 mutation carriers have a lower number of mature oocytes after ovarian stimulation for IVF/PGD. J Assist Reprod Genet [Internet]. Springer New York LLC; 2017 [cited 2021 May 16];34:1475–82. Available from: https://pubmed.ncbi.nlm.nih.gov/28831696/.
Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol [Internet]. J Clin Oncol; 2010 [cited 2021 May 16];28:240–4. Available from: https://pubmed.ncbi.nlm.nih.gov/19996028/.
Phillips KA, Collins IM, Milne RL, McLachlan SA, Friedlander M, Hickey M, et al. Anti-Müllerian hormone serum concentrations of women with germline BRCA1 or BRCA2 mutations. Hum Reprod Oxford University Press. 2016;31:1126–32.
Lambertini M, Moore HCF, Leonard RCF, Loibl S, Munster P, Bruzzone M, et al. Gonadotropin-releasing hormone agonists during chemotherapy for preservation of ovarian function and fertility in premenopausal patients with early breast cancer: a systematic review and meta-analysis of individual patient–level data [Internet]. J. Clin. Oncol. American Society of Clinical Oncology; 2018 [cited 2021 May 16]. p. 1981–90. Available from: https://pubmed.ncbi.nlm.nih.gov/29718793/.
Demeestere I, Brice P, Peccatori FA, Kentos A, Gaillard I, Zachee P, et al. Gonadotropin-releasing hormone agonist for the prevention of chemotherapy-induced ovarian failure in patients with lymphoma: 1-year follow-up of a prospective randomized trial. J Clin Oncol [Internet]. J Clin Oncol; 2013 [cited 2021 May 16];31:903–9. Available from: https://pubmed.ncbi.nlm.nih.gov/23129737/.
Blumenfeld Z. Fertility preservation using GnRH agonists: rationale, possible mechanisms, and explanation of controversy. Clin Med Insights Reprod Heal [Internet]. SAGE Publications; 2019 [cited 2021 May 16];13:117955811987016. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6710670/.
Durlinger ALL, Kramer P, Karels B, De Jong FH, Uilenbroek JTJ, Anton Grootegoed J, et al. Control of primordial follicle recruitment by anti-mullerian hormone in the mouse ovary. Endocrinology [Internet]. Endocrine Society; 1999 [cited 2021 May 16];140:5789–96. Available from: https://pubmed.ncbi.nlm.nih.gov/10579345/.
•• Kano M, Sosulski AE, Zhang LH, Saatcioglu HD, Wang D, Nagykery N, et al. AMH/MIS as a contraceptive that protects the ovarian reserve during chemotherapy. Proc Natl Acad Sci U S A. National Academy of Sciences; 2017;114:E1688–97. In a mouse model, AMH injection prior to chemotherapy blocks primordial follicle activation and preserves ovarian reserve.
Chronopoulou E, Raperport C, Sfakianakis A, Srivastava G, Homburg R. Elective oocyte cryopreservation for age-related fertility decline. J Assist Reprod Genet [Internet]. Springer; 2021 [cited 2021 Aug 20];38:1177. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7894970/.
Doyle J, Richter K, Lim J, Stillman R, Graham J, Tucker M. Successful elective and medically indicated oocyte vitrification and warming for autologous in vitro fertilization, with predicted birth probabilities for fertility preservation according to number of cryopreserved oocytes and age at retrieval. Fertil Steril [Internet]. Fertil Steril; 2016 [cited 2021 Aug 20];105:459–466.e2. Available from: https://pubmed.ncbi.nlm.nih.gov/26604065/.
Franasiak JM, Forman EJ, Hong KH, Werner MD, Upham KM, Treff NR, et al. The nature of aneuploidy with increasing age of the female partner: a review of 15,169 consecutive trophectoderm biopsies evaluated with comprehensive chromosomal screening. Fertil Steril [Internet]. Elsevier Inc.; 2014 [cited 2021 Feb 26];101:656–663.e1. Available from: https://pubmed.ncbi.nlm.nih.gov/24355045/.
•• Blakemore J, Grifo J, DeVore S, Hodes-Wertz B, Berkeley A. Planned oocyte cryopreservation-10–15-year follow-up: return rates and cycle outcomes. Fertil Steril [Internet]. Fertil Steril; 2021 [cited 2021 Aug 20];115:1511–20. Available from: https://pubmed.ncbi.nlm.nih.gov/33712289/. Oocyte survival after vitrification is ~74% and about 40% of women return to use their vitrified oocytes.
Dewailly D, Andersen CY, Balen A, Broekmans F, Dilaver N, Fanchin R, et al. The physiology and clinical utility of anti-Müllerian hormone in women. Hum Reprod Update [Internet]. Oxford University Press; 2014 [cited 2021 May 15];20:370–85. Available from: https://pubmed.ncbi.nlm.nih.gov/24430863/.
M. Dólleman, M. J. Faddy, J. van Disseldorp, C. M. Messow, B. Leader, F. J. M. Broekmans. The relationship between anti-Müllerian hormone in women receiving fertility assessments and age at menopause in subfertile women: evidence from large population studies). J Clin Endocrinol Metab [Internet]. 2013 [cited 2021 May 16];98:1946–53. Available from: https://academic.oup.com/jcem/article/98/5/1946/2536930.
Freeman EW, Sammel MD, Lin H, Gracia CR. Anti-Mullerian hormone as a predictor of time to menopause in late reproductive age women. J Clin Endocrinol Metab [Internet]. J Clin Endocrinol Metab; 2012 [cited 2021 May 16];97:1673–80. Available from: https://pubmed.ncbi.nlm.nih.gov/22378815/.
Bentzen JG, Forman JL, Larsen EC, Pinborg A, Johannsen TH, Schmidt L, et al. Maternal menopause as a predictor of anti-Müllerian hormone level and antral follicle count in daughters during reproductive age. Hum Reprod [Internet]. Oxford University Press; 2013 [cited 2021 May 16];28:247–55. Available from: https://pubmed.ncbi.nlm.nih.gov/23136135/.
•• Finkelstein JS, Lee H, Karlamangla A, Nee RM, Slus PM, Burnett-Bowie SAM, et al. Antimullerian hormone and impending menopause in late reproductive age: the study of women’s health across the nation. J Clin Endocrinol Metab [Internet]. Endocrine Society; 2020 [cited 2021 May 16];105:E1862–71. Available from: https://pubmed.ncbi.nlm.nih.gov/31965189/. The probability of entering menopause within one year for women with an AMH <0.01 is 51% for women <48 years-old and 79% for women ≥51 years-old.
Depmann M, Eijkemans MJC, Broer SL, Scheffer GJ, Van Rooij IAJ, Laven JSE, et al. Does anti-Müllerian hormone predict menopause in the general population? Results of a prospective ongoing cohort study. Hum Reprod [Internet]. Oxford University Press; 2016 [cited 2021 May 16];31:1580–7. Available from: https://pubmed.ncbi.nlm.nih.gov/27179263/.
Nelson LM. Primary ovarian insufficiency. N Engl J Med [Internet]. Massachusetts Medical Society; 2009 [cited 2021 May 16];360:606–14. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19196677.
Lunding SA, Aksglaede L, Anderson RA, Main KM, Juul A, Hagen CP, et al. AMH as predictor of premature ovarian insufficiency: a longitudinal study of 120 turner syndrome patients. J Clin Endocrinol Metab [Internet]. Endocrine Society; 2015 [cited 2021 May 16];100:E1030–8. Available from: https://pubmed.ncbi.nlm.nih.gov/25978111/.
•• Anderson RA, Nelson SM. Anti-Müllerian hormone in the diagnosis and prediction of premature ovarian insufficiency. Semin Reprod Med [Internet]. Thieme Medical Publishers, Inc.; 2020 [cited 2021 May 16];38. Available from: https://pubmed.ncbi.nlm.nih.gov/33429444/. AMH levels can be used to diagnose POI, but are not useful to predict the onset of menopause in post-pubertal patients at risk of POI.
Bidet M, Bachelot A, Bissauge E, Golmard JL, Gricourt S, Dulon J, et al. Resumption of ovarian function and pregnancies in 358 patients with premature ovarian failure. J Clin Endocrinol Metab [Internet]. Oxford Academic; 2011 [cited 2021 May 16];96:3864–72. Available from: https://academic.oup.com/jcem/article/96/12/3864/2834954.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Reproductive Endocrinology and Infertility (REI)
Rights and permissions
About this article
Cite this article
Gordon, C.E., Yanushpolsky, E. Anti-Müllerian Hormone: Current Understanding and Clinical Use. Curr Obstet Gynecol Rep 10, 61–70 (2021). https://doi.org/10.1007/s13669-021-00310-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-021-00310-7