Abstract
Purpose of Review
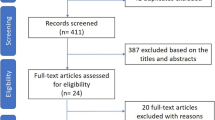
We conducted a review of the current evidence relating to antibiotic duration in the short- and long-term management of non-cystic fibrosis bronchiectasis.
Recent Findings
In non-cystic fibrosis pulmonary exacerbations, evidence is primarily based on expert consensus and recent guidelines recommend antibiotic durations of approximately 14 days. Chronic antibiotics (oral or inhaled) are recommended in patients with frequent exacerbations or with chronic Pseudomonas aeruginosa airways infection. Macrolides are the best studied therapies for long-term use with evidence for effect limited to a 12-month duration. Encouragingly, there are increased efforts to develop registries and conduct larger population-level studies to improve patient care.
Summary
There is a paucity of evidence for optimal antibiotic strategies in exacerbations and chronic maintenance in persons with non-cystic fibrosis bronchiectasis. Rationally designed studies which utilize a registry and population-based approach will be critical to build evidence-based strategies to optimize management of non-cystic fibrosis bronchiectasis.
Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Chalmers J, Smith MP, McHugh BJ, Doherty C, Govan JR, Hill AT. Short- and long-term antibiotic treatment reduces airways and systemic inflammation in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2012;186(7):657–65.
Chalmers J, Goeminne P, Aliberti S, et al. The bronchiectasis severity index. An international derivation and validation study. Am J Respir Crit Care Med. 2014;189:576–85.
Kapur N, Masters IB, Chang AB. Longitudinal growth and lung function in pediatric non-cystic fibrosis bronchiectasis: what influences lung function stability? Chest. 2010;138:158–64.
Sheehan R, Wells AU, Copley SJ, Desai SR, Howling SJ, Cole PJ, et al. A comparison of serial computed tomography and functional change in bronchiectasis. Eur Respir J. 2002;20:581–7.
Aliberti S, Lonni S, Dore S, et al. Clinical phenotype in adult patients with bronchiectasis. Eur Respir J. 2016;47:1113–22.
•• Polverino E, Goeminne PC, McDonnell MJ, et al. European Respiratory Society guidelines for the management of adult bronchiectasis. Eur Respir J. 2017;50:1700629 This is the most recent guideline for nCFB and summarizes current evidence for management.
Cole P. Inflammation: a two-edge sword – the model of bronchiectasis. Eur J Respir Dis. 1986;69:6–15.
Hoegger M, Fischer AJ, McMenimen JD, et al. Impaired mucus detachment disrupts mucociliary transport in a piglet model of cystic fibrosis. Science. 2014;345:818–22.
Pezzulo A, Tang XX, Hoegger MJ, et al. Reduced airway surface pH impairs bacterial killing in the porcine cystic fibrosis lung. Nature. 2012;487(7405):109–13.
O’Donnell A. Bronchiectasis. Chest. 2008;134:815–23.
Tunney M, Einarsson GG, Wei L, et al. Lung microbiota and bacterial abundance in patients with bronchiectasis when clinically stable and during exacerbation. Am J Respir Crit Care Med. 2013;187(10):1118–26.
Rogers G, Zain NM, Bruce KD, et al. A novel microbiota stratification system predicts future exacerbations in bronchiectasis. Ann Am Thorac Soc. 2014;11:496–503.
Ho P, Chan KN, Ip MS, et al. The effect of Pseudomonas aeruginosa infection on clinical parameters in steady-state bronchiectasis. Chest. 1998;114(6):1594–8.
Angrill J, Agustí C, de Celis R, et al. Bacterial colonisation in patients with bronchiectasis: microbiological pattern and risk factors. Thorax. 2002;57:15–9.
Loebinger M, Wells AU, Hansell DM, et al. Mortality in bronchiectasis: a long-term study assessing the factors influencing survival. Eur Respir J. 2009;34(4):843–9.
Woo T, Lim R, Surette MG, et al. Epidemiology and natural history of Pseudomonas aeruginosa airway infections in non-cystic fibrosis bronchiectasis. ERJ Open Res. 2018;4:00162–2017.
De Soyza A, Perry A, Hall AJ, et al. Molecular epidemiological analysis suggests cross-infection with Pseudomonas aeruginosa is rare in non-cystic fibrosis bronchiectasis. Eur Respir J. 2014;43(3):900–3.
•• Hill A, Haworth CS, Aliberti S, Barker A, Blasi F, Boersma W, et al. Pulmonary exacerbation in adults with bronchiectasis: a consensus definition for clinical research. Eur Respir J. 2017;49(6). This study is important as it aims to develop a standardized definition for pulmonary exacerbations specific to non-cystic fibrosis bronchiectasis.):1700051.
Weycker D, Oster G, Tino G. Prevalence and economic burden of bronchiectasis. Clin Pulm Med. 2005;12(4):205–9.
O’Donnell A, Barker AF, Ilowite JS, et al. Treatment of idiopathic bronchiectasis with aerosolized recombinant human DNase I. Chest. 1998;113:1329–34.
Barker A, O’Donnell AE, Flume P, et al. Aztreonam for inhalation solution in patients with non-cystic fibrosis bronchiectasis (AIR-BX1 and AIR-BX2): two randomized double-blind placebo-controlled phase 3 trials. Lancet Respir Med. 2014;2:738–49.
Orriols R, Hernando R, Ferrer A, et al. Eradication therapy against Pseudomonas aeruginosa in non-cystic fibrosis bronchiectasis. Respiration. 2015;90:290–305.
Orriols R, Roe J. Inhaled antibiotic therapy in non-cystic fibrosis patients with bronchiectasis and chronic bronchial infection by Pseudomonas aeruginosa. Respir Med. 1999;93:476–80.
White L, Mirrani G, Grover M, et al. Outcomes of Pseudomonas eradication therapy in patients with non-cystic fibrosis bronchiectasis. Respir Med. 2012;106:356–60.
•• Chalmers J, Aliberti S, Polverino E, et al. The EMBARC European Bronchiectasis registy: protocol for an international observational study. ERJ Open Res. 2016;2. This study is important as it is an effort to develop population-based studies to better understand and manage non-cystic fibrosis bronchiectasis.:00081–2015.
Vendrell M, de Gracia J, Olveira C, Martinez-Garcia MA, Girón R, Máiz L, et al. Normativa SEPAR: diagnostico y tratamiento de las bronquiectasias. Arch Bronconeumol. 2008;44:629–40.
Pasteur M, Bilton D, Hill AT, et al. British Thoracic Society guideline for non-CF bronchiectasis. Thorax. 2010;65:i1–i58.
Hill A, Sullivan AL, Chalmers JD, et al. British Thoracic Society guideline for bronchiectasis in adults. Thorax. 2019;74:1–69.
• Judson M, Chaudhry H, Compa DR, O’Donnell AE. A Delphi study of pharmacotherpapy for noncystic fibrosis bronchiectasis. Am J Med Sci. 2014;348(5):387–93 This study attempts to assess the evidence of the therapies utilized for non-cystic fibrosis bronchiectasis.
Bilton D, Henig N, Morrissey B, Gotfried M. Addition of inhaled tobramycin to ciprofloxacin for acute exacerbations of Pseudomonas aeruginosa infection in adult bronchiectasis. Chest. 2006;130:1503–10.
Murray M, Turnbull K, MacQuarrie S, et al. Assessing response to treatment of exacerbations of bronchiectasis in adults. Eur Respir J. 2009;33:312–7.
Friedman N, Temkin E, Carmeli Y. The negative impact of antibiotic resistance. Clin Microbiol Infect. 2016;22(5):416–22.
Eliopoulous G, Cosgrove SE, Carmeli Y. The impact of antimicrobial resistance on health and economic outcomes. Clin Infect Dis. 2003;36(11):1433–7.
Thabit AK, Crandon JL, Nicolau DP. Antimicrobial resistance: impact on clinical and economic outcomes and the need for new antimicrobials. Expert Opin Pharmacother. 2015;16(2):159–77.
Doern G, Brecher SM. The clinical predictive value (or lack thereof) of the results of In vitro antimicrobial susceptibility tests. J Clin Microbiol. 2011;49:S11–4.
Somayaji R, Parkins MD, Shah A, et al. Antimicrobial resistance in cystic fibrosis international working group. Antimicrobial susceptibility testing (AST) and associated clinical outcomes in individuals with cystic fibrosis: a systematic review. J Cyst Fibros. 2019;18(2):236–43.
Cogen J, Whitlock KB, Gibson RL, Hoffman LR, VanDevanter DR. The use of antimicrobial susceptibility testing in pediatric cystic fibrosis pulmonary exacerbations. J Cyst Fibros. 2019;(19):30764–7. https://doi.org/10.1016/j.jcf.2019.05.012.
Murray M, Govan JRW, Doherty CJ, et al. A randomized controlled trial of nebulized gentamicin in non-cystic fibrosis bronchiectasis. Am J Respir Crit Care Med. 2011;183:491–9.
Serisier D, Bilton D, De Soyza A, et al. Inhaled, dual release liposomal ciprofloxacin in non-cystic fibrosis bronchiectasis (ORBIT-2): a randomised, double-blind, placebo-controlled trial. Thorax. 2013;68:812–7.
Haworth C, Foweraker JE, Wilkinson P, et al. Inhaled colistin in patients with bronchiectasis and chronic Pseudomonas aeruginosa infection. Am J Respir Crit Care Med. 2014;189:975–82.
Currie D, Garbett ND, Chan KI, et al. Double-blind randomized study of prolonged higher-dose oral amoxycillin in purulent bronchiectasis. Q J Med. 1990;76:799–816.
PROLONGED antibiotic treatement of severe bronchiectasis: a report by a subcommittee of the Antibiotics Clinical Trials (non-tuberculous) Committee of the Medical Research Council. Br Med J. 1957;2:255–259.
• Hnin K, Nguyen C, Carson KV, et al. Prolonged antibiotics for non-cystic fibrosis bronchiectasis in children and adults. Cochrane Database Syst Rev. 2015;8:CD001392 This study assessess the current evidence for use of long-term antibiotics in non-cystic fibrosis bronchiectasis.
Gao Y, Guan W, Xu G, et al. Macrolide therapy in adults and children with non-cystic fibrosis bronchiectasis: a systematic review and meta-analysis. PLoS One. 2014;9:e90047.
Brodt A, Stovold E, Zhang L. Inhaled antibiotics for stable non-cystic fibrosis bronchiectasis: a systematic review. Eur Respir J. 2014;44:382–93.
Shi Z, Peng H, Hu XW, Hu JG. Effectiveness and safety of macrolides in bronchiectasis patients: a meta-analysis and systematic review. Pulm Pharmacol Ther. 2014;28:171–8.
Wong C, Jayaram I, Karalus N, et al. Azithromycin for prevention of exacerbations in non-cystic fibrosis bronchiectasis (EMBRACE): a randomized, double-blind, placebo-controlled trial. Lancet. 2012;380:660–7.
Serisier D, Martin ML, McGuckin MA, et al. Effect of long-term, low-dose erythromycin on pulmonary exacerbations among patients with non-cystic fibrosis bronchiectasis: the BLESS randomized controlled trial. JAMA. 2013;309:1260–7.
Altenburg J. Effect of azithromycin maintenance treatment on infectious exacerbations among patients with non-cystic fibrosis bronchiectasis. JAMA. 2013;309:1251–9.
Nichols DP, Odem-Davis K, Cogen JD, et al. Pulmonary outcomes associated with long-term azithromycin therapy in cystic fibrosis. Am J Respir Crit Care Med 2019. https://doi.org/10.1164/rccm.201906-1206OC.
West N, Beckett VV, Jain R, on behalf of the STOP investigators, et al. Standardized Treatment of Pulmonary Exacerbations (STOP) study: physician treatment practices and outcomes for individuals with cystic fibrosis with pulmonary exacerbations. J Cyst Fibros. 2017;16:600–6.
Sanders D, Solomon GM, Beckett VV, on behalf of the STOP Study Group, et al. Standardized Treatment of Pulmonary Exacerbations (STOP) Study: observations at the initiation of intravenous antibiotics for cystic fibrosis pulmonary exacerbations. J Cyst Fibros. 2017;16:592–9.
Ford I, Norrie J. Pragmatic trials. N Engl J Med. 2016;375:454–63.
Funding
Dr. Goss’ research time is supported by the Cystic Fibrosis Foundation Therapeutics (GOSS13A0) and NIH (P30 DK089507, UL1TR000423). There was no role of funding sources in writing of this manuscript, or the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
All authors participated in drafting and/or revising the manuscript for intellectual content, and edited the manuscript for final approval.
Corresponding author
Ethics declarations
Conflict of Interest
Ranjani Somayaji declares no conflict of interest. Christopher Goss reports grants from Cystic Fibrosis Foundation, grants from European Commission, grants from NIH (NHLBI), grants from NIH (NIDDK and NCRR), personal fees from Gilead Sciences for serving as a Chair of a Grant Review Committee; personal fees from Novartis serving as a DSMB Chair for a trial supported by Novartis and the European Commission, grants from NIH, and grants from FDA for funding to study a novel antimicrobial in cystic fibrosis, and served a US lead in a phase 2 trial of novel therapy for cystic fibrosis support from Boehringer Ingelheim.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Disclaimer
None of the work presented in this opinion piece was influenced by the funding sources noted above. The funding sources that support other ongoing researches played no role in writing this manuscript, or in the decision to submit for publication.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Bronchiectasis
Rights and permissions
About this article
Cite this article
Somayaji, R., Goss, C.H. Duration of Antibiotic Therapy in Non-cystic Fibrosis Bronchiectasis. Curr Pulmonol Rep 8, 160–165 (2019). https://doi.org/10.1007/s13665-019-00235-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13665-019-00235-w