Abstract
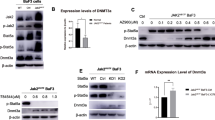
Escalated PD-L1 expression has been identified during malignant transformation in a number of cancer types and helps cancer cells escape an effective anti-tumor immune response. The mechanisms underlying escalated production of PD-L1 in many cancers, however, are still far from clear. We studied PD-L1, STAT3 and STAT5 mRNA expression using qRT-PCR in 72 BCR/ABL1 negative myeloproliferative neoplasm (MPN) patients (39 polycythemia vera and 33 essential thrombocythemia). Furthermore, phosphorylation status of STAT3 and STAT5 was studied using immunoblotting in the same patients. All MPN patients were first screened for JAK2 (V617F) mutation by tetra-primer ARMS-PCR, followed by quantification of JAK2 (V617F) mutation burden in all V617F positive MPN patients by ASO-PCR. Patients were screened for BCR/ABL1 fusion gene transcripts to rule out Ph positive status. Our findings showed that mRNA levels of PD-L1 and STAT3 were significantly higher in JAK2 (V617F) MPN patients, while as STAT5 was insignificantly upregulated. STAT3 and STAT5 phosphorylation was seen to be higher in JAK2 (V617F) MPN patients compared to the JAK2 (WT) patients. Upregulation of PD-L1, STAT3 and STAT5 was significantly associated with JAK2 (V617F) percentage in MPN patients. PD-L1, STAT3 and STAT5 expression significantly and positively correlated with JAK2 (V617F) allele burden. In addition, significant coexpression of PD-L1 with STAT3 and STAT5 was observed in MPN patients. In summary, JAK2 (V617F) mutation is accompanied by increased PD-L1 expression and this PD-L1 over expression is mediated by JAK2 (V617F) mainly through STAT3, while as STAT5 may play a minor role.
Graphic abstract





Similar content being viewed by others
Change history
14 July 2020
In the original publication, third author name was incorrectly published as “Ab Rashid Mir”. The correct name should read as “Rashid Mir”.
References
Chemnitz JM, et al. SHP-1 and SHP-2 associate with immunoreceptor tyrosine-based switch motif of programmed death 1 upon primary human T cell stimulation, but only receptor ligation prevents T cell activation. J Immunol. 2004;173(2):945–54.
Dong H, et al. B7–H1, a third member of the B7 family, co-stimulates T-cell proliferation and interleukin-10 secretion. Nat Med. 1999;5(12):1365–9.
Velcheti V, Rimm DL, Schalper KA. Sarcomatoid lung carcinomas show high levels of programmed death ligand-1 (PD-L1). J Thorac Oncol. 2013;8(6):803–5.
Velcheti V, et al. Programmed death ligand-1 expression in non-small cell lung cancer. Lab Investig. 2014;94(1):107–16.
Hamanishi J, et al. Programmed cell death 1 ligand 1 and tumor-infiltrating CD8+ T lymphocytes are prognostic factors of human ovarian cancer. Proc Natl Acad Sci USA. 2007;104(9):3360–5.
Hamanishi J, et al. PD-1/PD-L1 blockade in cancer treatment: perspectives and issues. Int J Clin Oncol. 2016;21(3):462–73.
Thompson RH, et al. Costimulatory B7–H1 in renal cell carcinoma patients: Indicator of tumor aggressiveness and potential therapeutic target. Proc Natl Acad Sci USA. 2004;101(49):17174–9.
Shen JK, et al. Programmed cell death ligand 1 expression in osteosarcoma. Cancer Immunol Res. 2014;2(7):690–8.
Norde WJ, et al. PD-1/PD-L1 interactions contribute to functional T-cell impairment in patients who relapse with cancer after allogeneic stem cell transplantation. Can Res. 2011;71(15):5111–222.
Michot JM, et al. Immune-related adverse events with immune checkpoint blockade: a comprehensive review. Eur J Cancer. 2016;54:139–48.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Wolchok J. How recent advances in immunotherapy are changing the standard of care for patients with metastatic melanoma. Ann Oncol. 2012;23(Supp1 8):viii5–21.
Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363(8):711–23.
Topalian SL, et al. Safety, activity, and immune correlates of anti-PD-1 antibody in cancer. N Engl J Med. 2012;366(26):2443–544.
Dunn GP, et al. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3(11):991–8.
Mapara MY, Sykes M. Tolerance and cancer: mechanisms of tumor evasion and strategies for breaking tolerance. J Clin Oncol. 2004;22(6):1136–51.
Marincola FM, et al. Tumors as elusive targets of T cell-based active immunotherapy. Trends Immunol. 2003;24(6):335–42.
Hersey P, Zhang XD. How melanoma cells evade trail-induced apoptosis. Nat Rev Cancer. 2001;1(2):142–50.
Lonchay C, et al. Correlation between tumor regression and T cell responses in melanoma patients vaccinated with a MAGE antigen. Proc Natl Acad Sci USA. 2004;101(Suppl 2):14631–8.
Ansell SM, et al. PD-1 blockade with nivolumab in relapsed or refractory Hodgkin's lymphoma. N Engl J Med. 2015;372(4):311–9.
Chen R, et al. Phase II study of the efficacy and safety of pembrolizumab for relapsed/refractory classic hodgkin lymphoma. J Clin Oncol. 2017;35(19):2125–32.
Prestipino A, et al. Oncogenic JAK2(V617F) causes PD-L1 expression, mediating immune escape in myeloproliferative neoplasms. Sci Transl Med. 2018;10(429):eaam7729.
Arber DA, et al. The 2016 revision to the World Health Organization classification of myeloid neoplasms and acute leukemia. Blood. 2016;127(20):2391–405.
Barbui T, et al. The 2016 revision of WHO classification of myeloproliferative neoplasms: clinical and molecular advances. Blood Rev. 2016;30(6):453–9.
Tefferi A. Novel mutations and their functional and clinical relevance in myeloproliferative neoplasms: JAK2, MPL, TET2, ASXL1, CBL, IDH and IKZF1. Leukemia. 2010;24(6):1128–38.
Baxter EJ, et al. Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054–61.
James C, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144–8.
Vannucchi AM, et al. Clinical correlates of JAK2V617F presence or allele burden in myeloproliferative neoplasms: a critical reappraisal. Leukemia. 2008;22(7):1299–307.
Passamonti F, et al. A prospective study of 338 patients with polycythemia vera: the impact of JAK2 (V617F) allele burden and leukocytosis on fibrotic or leukemic disease transformation and vascular complications. Leukemia. 2010;24(9):1574–9.
Tefferi A. Mutant molecules of interest in myeloproliferative neoplasms: introduction. Acta Haematol. 2008;119(4):192–3.
Passamonti F, et al. Relation between JAK2 (V617F) mutation status, granulocyte activation, and constitutive mobilization of CD34+ cells into peripheral blood in myeloproliferative disorders. Blood. 2006;107(9):3676–82.
Scott LM, et al. Progenitors homozygous for the V617F mutation occur in most patients with polycythemia vera, but not essential thrombocythemia. Blood. 2006;108(7):2435–7.
Tefferi A, et al. The clinical phenotype of wild-type, heterozygous, and homozygous JAK2V617F in polycythemia vera. Cancer. 2006;106(3):631–5.
Vannucchi AM, et al. Prospective identification of high-risk polycythemia vera patients based on JAK2(V617F) allele burden. Leukemia. 2007;21(9):1952–9.
Vannucchi AM, et al. Clinical profile of homozygous JAK2 617V%3eF mutation in patients with polycythemia vera or essential thrombocythemia. Blood. 2007;110(3):840–6.
Alvarez-Larran A, et al. Postpolycythaemic myelofibrosis: frequency and risk factors for this complication in 116 patients. Br J Haematol. 2009;146(5):504–9.
Passamonti F, et al. A dynamic prognostic model to predict survival in post-polycythemia vera myelofibrosis. Blood. 2008;111(7):3383–7.
Kralovics R, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779–900.
Marzec M, et al. Oncogenic kinase NPM/ALK induces through STAT3 expression of immunosuppressive protein CD274 (PD-L1, B7–H1). Proc Natl Acad Sci USA. 2008;105(52):20852–7.
Wolfle SJ, et al. PD-L1 expression on tolerogenic APCs is controlled by STAT-3. Eur J Immunol. 2011;41(2):413–24.
Rosenberg JE, et al. Atezolizumab in patients with locally advanced and metastatic urothelial carcinoma who have progressed following treatment with platinum-based chemotherapy: a single-arm, multicentre, phase 2 trial. Lancet. 2016;387(10031):1909–20.
Butte MJ, et al. Programmed death-1 ligand 1 interacts specifically with the B7–1 costimulatory molecule to inhibit T cell responses. Immunity. 2007;27(1):111–22.
Francisco LM, Sage PT, Sharpe AH. The PD-1 pathway in tolerance and autoimmunity. Immunol Rev. 2010;236:219–42.
Ohaegbulam KC, et al. Human cancer immunotherapy with antibodies to the PD-1 and PD-L1 pathway. Trends Mol Med. 2015;21(1):24–33.
Topalian SL, et al. Mechanism-driven biomarkers to guide immune checkpoint blockade in cancer therapy. Nat Rev Cancer. 2016;16(5):275–87.
Postow MA, Callahan MK, Wolchok JD. Immune checkpoint blockade in cancer therapy. J Clin Oncol. 2015;33(17):1974–82.
Jones AV, et al. Widespread occurrence of the JAK2 V617F mutation in chronic myeloproliferative disorders. Blood. 2005;106(6):2162–8.
Guru SA, et al. PDGFRalpha promoter polymorphisms and expression patterns influence risk of development of imatinib-induced thrombocytopenia in chronic myeloid leukemia: a study from India. Tumour Biol. 2017;39(10):1010428317713857.
Hochberg EP, et al. A novel rapid single nucleotide polymorphism (SNP)-based method for assessment of hematopoietic chimerism after allogeneic stem cell transplantation. Blood. 2003;101(1):363–9.
Paterson AM, et al. The programmed death-1 ligand 1:B7–1 pathway restrains diabetogenic effector T cells in vivo. J Immunol. 2011;187(3):1097–105.
Inman BA, et al. Atezolizumab: A PD-L1-blocking antibody for bladder cancer. Clin Cancer Res. 2017;23(8):1886–900.
Deng R, et al. Preclinical pharmacokinetics, pharmacodynamics, tissue distribution, and tumor penetration of anti-PD-L1 monoclonal antibody, an immune checkpoint inhibitor. mAbs. 2016;8(3):593–603.
Stewart R, et al. Identification and characterization of MEDI4736, an antagonistic Anti-PD-L1 monoclonal antibody. Cancer Immunol Res. 2015;3(9):1052–62.
Mok T, et al. 192TiP: NEPTUNE: a global, phase 3 study of durvalumab (MEDI4736) plus tremelimumab combination therapy versus standard of care (SoC) platinum-based chemotherapy in the first-line treatment of patients (pts) with advanced or metastatic NSCLC. J Thorac Oncol. 2016;11:S140–S141141.
Kolbusz RV, et al. Exaggerated response to insect bites. An unusual cutaneous manifestation of chronic lymphocytic leukemia. Int J Dermatol. 1989;28(3):186–7.
Grenga I, et al. A fully human IgG1 anti-PD-L1 MAb in an in vitro assay enhances antigen-specific T cell responses. Clin Transl Immunol. 2016;5(5):e83.
Boyerinas B, et al. Antibody-dependent cellular cytotoxicity activity of a novel anti-PD-L1 antibody avelumab (MSB0010718C) on human tumor cells. Cancer Immunol Res. 2015;3(10):1148–57.
Fujii R, et al. Enhanced killing of chordoma cells by antibody-dependent cell-mediated cytotoxicity employing the novel anti-PD-L1 antibody avelumab. Oncotarget. 2016;7(23):33498–511.
Kataoka K, et al. Aberrant PD-L1 expression through 3'-UTR disruption in multiple cancers. Nature. 2016;534(7607):402–6.
Xie QK, et al. Programmed death ligand 1 as an indicator of pre-existing adaptive immune responses in human hepatocellular carcinoma. Oncoimmunology. 2016;5(7):e1181252.
Ikeda S, et al. PD-L1 Is upregulated by simultaneous amplification of the PD-L1 and JAK2 genes in non-small cell lung cancer. J Thorac Oncol. 2016;11(1):62–71.
Lee SJ, et al. Interferon regulatory factor-1 is prerequisite to the constitutive expression and IFN-gamma-induced upregulation of B7–H1 (CD274). FEBS Lett. 2006;580(3):755–62.
Shin DS, et al. Primary resistance to PD-1 blockade mediated by JAK1/2 mutations. Cancer Discov. 2017;7(2):188–201.
Garcia-Diaz A, et al. Interferon receptor signaling pathways regulating PD-L1 and PD-L2 expression. Cell Rep. 2017;19(6):1189–201.
Acknowledgements
Sameer Ahmad Guru acknowledges Indian Council of Medical Research (ICMR), Government of India (GOI) for providing financial support to carry out the research. He further extends his gratitude towards Multidisciplinary Research Unit (MRU), MAMC, New Delhi for providing lab space to carry out part of experimental work. We also extend our thanks to technical staff especially Mrs. Shobha for maintaining the aseptic conditions in laboratory.
Funding
Authors do not have any financial relationship with the organization that sponsored the research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Ethical approval
The study was approved by the Institutional Ethics Committee (IEC) of Maulana Azad Medical College (MAMC) and associated Hospitals; Lok Nayak Jay Prakash (LNJP), Govind Balab Pant Institute of Postgraduate Medical Education and Research (GIPMER), Guru Nanak Eye Centre, New Delhi, India (registered with Drug Controller General of India, Directorate of General Health Services, New Delhi) with study approval number issued F.1/IEC/MAMC/ (38)/4/2017/No: 211.
Informed consent
Our sincere and deep gratitude goes to all the patients included in this study for giving consent and making this study possible.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised due to correct the third author name.
Rights and permissions
About this article
Cite this article
Guru, S.A., Sumi, M.P., Mir, R. et al. Ectopic PD-L1 expression in JAK2 (V617F) myeloproliferative neoplasm patients is mediated via increased activation of STAT3 and STAT5. Human Cell 33, 1099–1111 (2020). https://doi.org/10.1007/s13577-020-00370-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13577-020-00370-6