Abstract
Objective
Clinical questions arise frequently at the point of care, and approximately half of these questions go unanswered, representing an opportunity to improve quality of care. Radiation oncologists perform the unique task of contour delineation, which has been linked to decreased survival and increased toxicity when performed inaccurately. Little is known about how radiation oncologists approach contouring-related questions in clinical practice.
Methods
A survey was distributed to all attendees of an educational contouring symposium at the 2017 Annual Meeting of the American College of Radiation Oncology. Providers indicated their years of clinical experience and level of specialization and answered questions regarding resources used to answer contouring-related questions, awareness of consensus contouring guidelines, and barriers to guideline usage.
Results
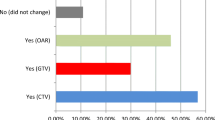
Eighty-three out of 85 radiation oncologists attending the symposium returned the survey (97.6%). The majority of respondents were generalists (85%) and had over 10 years of clinical experience (73%). The most frequently used contouring resource was Radiation Therapy Oncology Group atlases (mean Likert score 4.1). Participants correctly identified the existence of consensus contouring guideline publications 42% of the time. The main barriers to guideline usage were a lack of awareness regarding publication (60%), poor ease of use (30%), lack of time (23%), and lack of comprehensiveness of available resources (21%).
Conclusion
This study provides information to guide further development and implementation of contouring resources, with radiation oncologists preferring resources that are atlas-based and can be accessed quickly and easily. Both self-reported and objectively tested awareness of consensus contouring guidelines was low, reflecting a need for better guideline dissemination.




Similar content being viewed by others
References
Segedin B, Petric P (2016) Uncertainties in target volume delineation in radiotherapy—are they relevant and what can we do about them? Radiol Oncol 50(3):254–262. https://doi.org/10.1515/raon-2016-0023
Berry SL, Boczkowski A, Ma R, Mechalakos J, Hunt M (2016) Interobserver variability in radiation therapy plan output: results of a single-institution study. Pract Radiat Oncol 6(6):442–449. https://doi.org/10.1016/j.prro.2016.04.005
Peters LJ, O'Sullivan B, Giralt J, Fitzgerald TJ, Trotti A, Bernier J, Bourhis J, Yuen K, Fisher R, Rischin D (2010) Critical impact of radiotherapy protocol compliance and quality in the treatment of advanced head and neck cancer: results from TROG 02.02. J Clin Oncol 28(18):2996–3001. https://doi.org/10.1200/JCO.2009.27.4498
Ohri N, Shen X, Dicker AP, Doyle LA, Harrison AS, Showalter TN (2013) Radiotherapy protocol deviations and clinical outcomes: a meta-analysis of cooperative group clinical trials. J Natl Cancer Inst 105(6):387–393. https://doi.org/10.1093/jnci/djt001
Boero IJ, Paravati AJ, Xu B, Cohen EEW, Mell LK, Le QT, Murphy JD (2016) Importance of radiation oncologist experience among patients with head-and-neck cancer treated with intensity-modulated radiation therapy. J Clin Oncol 34(7):684–690. https://doi.org/10.1200/JCO.2015.63.9898
Del Fiol G, Workman TE, Gorman PN (2014) Clinical questions raised by clinicians at the point of care: a systematic review. JAMA Intern Med 174(5):710–718. https://doi.org/10.1001/jamainternmed.2014.368
Ellsworth MA, Homan JM, Cimino JJ, Peters SG, Pickering BW, Herasevich V (2015) Point-of-care knowledge-based resource needs of clinicians: a survey from a large academic medical center. Appl Clin Inform 6(2):305–317. https://doi.org/10.4338/ACI-2014-11-RA-0104
Osheroff JA, Forsythe DE, Buchanan BG, Bankowitz RA, Blumenfeld BH, Miller RA (1991) Physicians’ information needs: analysis of questions posed during clinical teaching. Ann Intern Med 114(7):576–581. https://doi.org/10.7326/0003-4819-114-7-576
González-González AI, Dawes M, Sánchez-Mateos J et al (2007) Information needs and information-seeking behavior of primary care physicians. Ann Fam Med 5(4):345–352. https://doi.org/10.1370/afm.681
Green ML, Ciampi MA, Ellis PJ (2000) Residents’ medical information needs in clinic: are they being met? Am J Med 109(3):218–223. https://doi.org/10.1016/S0002-9343(00)00458-7
Ely JW, Osheroff JA, Chambliss ML, Ebell MH, Rosenbaum ME (2005) Answering physicians’ clinical questions: obstacles and potential solutions. J Am Med Inform Assoc 12(2):217–224. https://doi.org/10.1197/jamia.M1608
Ely JW, Osheroff JA, Ebell MH, Chambliss ML, Vinson DC, Stevermer JJ, Pifer EA (2002) Obstacles to answering doctors’ questions about patient care with evidence: qualitative study. BMJ 324(7339):710. https://doi.org/10.1136/bmj.324.7339.710
Grimshaw JM, Russell IT (1993) Effect of clinical guidelines on medical practice: a systematic review of rigorous evaluations. Lancet 342(8883):1317–1322. https://doi.org/10.1016/0140-6736(93)92244-N
Jagsi R, Huang G, Griffith K, Zikmund-Fisher BJ, Janz NK, Griggs JJ, Katz SJ, Hawley ST (2014) Attitudes toward and use of cancer management guidelines in a national sample of medical oncologists and surgeons. J Natl Compr Cancer Netw 12(2):204–212. https://doi.org/10.6004/jnccn.2014.0021
Dillmon M, Goldberg JM, Ramalingam SS et al (2012) Clinical practice guidelines for cancer care: utilization and expectations of the practicing oncologist. J Oncol Pract 8(6):350–353 352 p following 353
Somerfield MR, Bohlke K, Browman GP, Denduluri N, Einhaus K, Hayes DF, Khorana AA, Miller RS, Mohile SG, Oliver TK, Ortiz E, Lyman GH (2016) Innovations in American Society of Clinical Oncology Practice Guideline Development. J Clin Oncol 34(26):3213–3220. https://doi.org/10.1200/JCO.2016.68.3524
Han LC, Delpe S, Shah ND, Ziegenfuss JY, Tilburt JC, Karnes RJ, Nguyen PL, Gross CP, Yu JB, Trinh QD, Sun M, Ranasinghe WKB, Kim SP (2014) Perceptions of radiation oncologists and urologists on sources and type of evidence to inform prostate cancer treatment decisions. Int J Radiat Oncol Biol Phys 89(2):277–283. https://doi.org/10.1016/j.ijrobp.2014.02.001
Fuller CD, Nijkamp J, Duppen JC, Rasch CR, Thomas CR Jr, Wang SJ, Okunieff P, Jones WE 3rd, Baseman D, Patel S, Demandante CG, Harris AM, Smith BD, Katz AW, McGann C, Harper JL, Chang DT, Smalley S, Marshall DT, Goodman KA, Papanikolaou N, Kachnic LA, Radiation Oncology Committee of the Southwest Oncology Group (2011) Prospective randomized double-blind pilot study of site-specific consensus atlas implementation for rectal cancer target volume delineation in the cooperative group setting. Int J Radiat Oncol Biol Phys 79(2):481–489. https://doi.org/10.1016/j.ijrobp.2009.11.012
Mavroidis P, Giantsoudis D, Awan MJ, Nijkamp J, Rasch CR, Duppen JC, Thomas CR Jr, Okunieff P, Jones WE 3rd, Kachnic LA, Papanikolaou N, Fuller CD, Southwest Oncology Group Radiation Oncology Committee (2014) Consequences of anorectal cancer atlas implementation in the cooperative group setting: radiobiologic analysis of a prospective randomized in silico target delineation study. Radiother Oncol 112(3):418–424. https://doi.org/10.1016/j.radonc.2014.05.011
Skinner A (2007) Survey research: designing an instrument. Johns Hopkins Bloomberg School of Public Health, Baltimore
AJ W, Bosch WR, Chang DT et al (2015) Expert consensus contouring guidelines for intensity modulated radiation therapy in esophageal and gastroesophageal junction cancer. Int J Radiat Oncol Biol Phys 92(4):911–920
Hong TS, Bosch WR, Krishnan S, Kim TK, Mamon HJ, Shyn P, Ben-Josef E, Seong J, Haddock MG, Cheng JC, Feng MU, Stephans KL, Roberge D, Crane C, Dawson LA (2014) Interobserver variability in target definition for hepatocellular carcinoma with and without portal vein thrombus: radiation therapy oncology group consensus guidelines. Int J Radiat Oncol Biol Phys 89(4):804–813. https://doi.org/10.1016/j.ijrobp.2014.03.041
Brouwer CL, Steenbakkers RJ, Bourhis J et al (2015) CT-based delineation of organs at risk in the head and neck region: DAHANCA, EORTC, GORTEC, HKNPCSG, NCIC CTG, NCRI, NRG Oncology and TROG consensus guidelines. Radiother Oncol 117(1):83–90. https://doi.org/10.1016/j.radonc.2015.07.041
Niyazi M, Brada M, Chalmers AJ, Combs SE, Erridge SC, Fiorentino A, Grosu AL, Lagerwaard FJ, Minniti G, Mirimanoff RO, Ricardi U, Short SC, Weber DC, Belka C (2016) ESTRO-ACROP guideline “target delineation of glioblastomas”. Radiother Oncol 118(1):35–42. https://doi.org/10.1016/j.radonc.2015.12.003
Cox BW, Spratt DE, Lovelock M, Bilsky MH, Lis E, Ryu S, Sheehan J, Gerszten PC, Chang E, Gibbs I, Soltys S, Sahgal A, Deasy J, Flickinger J, Quader M, Mindea S, Yamada Y (2012) International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(5):e597–e605. https://doi.org/10.1016/j.ijrobp.2012.03.009
Illidge T, Specht L, Yahalom J, Aleman B, Berthelsen AK, Constine L, Dabaja B, Dharmarajan K, Ng A, Ricardi U, Wirth A (2014) Modern radiation therapy for nodal non-Hodgkin lymphoma-target definition and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 89(1):49–58. https://doi.org/10.1016/j.ijrobp.2014.01.006
Yahalom J, Illidge T, Specht L, Hoppe RT, Li YX, Tsang R, Wirth A (2015) Modern radiation therapy for extranodal lymphomas: field and dose guidelines from the International Lymphoma Radiation Oncology Group. Int J Radiat Oncol Biol Phys 92(1):11–31. https://doi.org/10.1016/j.ijrobp.2015.01.009
Kastner M, Bhattacharyya O, Hayden L, Makarski J, Estey E, Durocher L, Chatterjee A, Perrier L, Graham ID, Straus SE, Zwarenstein M, Brouwers M (2015) Guideline uptake is influenced by six implementability domains for creating and communicating guidelines: a realist review. J Clin Epidemiol 68(5):498–509. https://doi.org/10.1016/j.jclinepi.2014.12.013
Lefresne S, Olivotto IA, Joe H, Blood PA, Olson RA (2013) Impact of quality assurance rounds in a Canadian radiation therapy department. Int J Radiat Oncol Biol Phys 85(3):e117–e121. https://doi.org/10.1016/j.ijrobp.2012.10.015
Bennett CL, Somerfield MR, Pfister DG, Tomori C, Yakren S, Bach PB, American Society of Clinical Oncology (2003) Perspectives on the value of American Society of Clinical Oncology clinical guidelines as reported by oncologists and health maintenance organizations. J Clin Oncol 21(5):937–941. https://doi.org/10.1200/JCO.2003.07.165
Grimshaw JM, Thomas RE, MacLennan G et al (2004) Effectiveness and efficiency of guideline dissemination and implementation strategies. Health Technol Assess 8(6):iii–iiv 1-72
Stafford RS, Bartholomew LK, Cushman WC, Cutler JA, Davis BR, Dawson G, Einhorn PT, Furberg CD, Piller LB, Pressel SL, Whelton PK, ALLHAT Collaborative Research Group (2010) Impact of the ALLHAT/JNC7 dissemination project on thiazide-type diuretic use. Arch Intern Med 170(10):851–858. https://doi.org/10.1001/archinternmed.2010.130
Flynn S, Hebert P, Korenstein D, Ryan M, Jordan WB, Keyhani S (2017) Leveraging social media to promote evidence-based continuing medical education. PLoS One 12(1):e0168962. https://doi.org/10.1371/journal.pone.0168962
Ibrahim AM, Lillemoe KD, Klingensmith ME, Dimick JB (2017) Visual abstracts to disseminate research on social media: a prospective, case-control crossover study. Ann Surg 266(6):e46–e48. https://doi.org/10.1097/SLA.0000000000002277
Bonis PA, Pickens GT, Rind DM et al (2008) Association of a clinical knowledge support system with improved patient safety, reduced complications and shorter length of stay among Medicare beneficiaries in acute care hospitals in the United States. Int J Med Inform 77(11):745–753. https://doi.org/10.1016/j.ijmedinf.2008.04.002
Isaac T, Zheng J, Jha A (2012) Use of UpToDate and outcomes in US hospitals. J Hosp Med 7(2):85–90. https://doi.org/10.1002/jhm.944
Gillespie EF, Panjwani N, Golden DW, Gunther JR, Chapman TR, Brower JV, Kosztyla R, Bykowski JM, Sanghvi P, Murphy JD (2016) Multi-institutional randomized trial testing the utility of an interactive three-dimensional contouring atlas among radiation oncology residents. Int J Radiat Oncol Biol Phys 96(2):E416–E417. https://doi.org/10.1016/j.ijrobp.2016.06.1677
Funding
The present study was supported by an American College of Radiation Oncology Education Seed Grant (to Erin F. Gillespie) and a small research grant from the Agency for Healthcare Research and Quality (grant R03HS024321 to James D. Murphy).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Erin F. Gillespie and James D. Murphy are co-founders of the non-profit contouring education website eContour (eContour.org). Michael V. Sherer, Alex K. Bryant, Abraham J. Wu, Parul N. Barry, Brian E. Lally, and Catheryn M. Yashar declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Documentation of informed consent was waived by the institutional review board.
Electronic supplementary material
ESM 1
(PDF 608 kb)
Rights and permissions
About this article
Cite this article
Sherer, M.V., Bryant, A.K., Wu, A.J. et al. Assessment of contouring resource use and awareness of contouring guidelines among radiation oncologists. J Radiat Oncol 7, 103–109 (2018). https://doi.org/10.1007/s13566-018-0343-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13566-018-0343-x