Abstract
In the first half of the twentieth century, the rate of death from infectious disease in the United States fell precipitously. Although this decline is well-known and well-documented, there is surprisingly little evidence about whether it took place uniformly across the regions of the United States. We use data on infectious disease deaths from all reporting U.S. cities to describe regional patterns in the decline of urban infectious mortality from 1900 to 1948. We report three main results. First, urban infectious mortality was higher in the South in every year from 1900 to 1948. Second, infectious mortality declined later in southern cities than in cities in the other regions. Third, comparatively high infectious mortality in southern cities was driven primarily by extremely high infectious mortality among African Americans. From 1906 to 1920, African Americans in cities experienced a rate of death from infectious disease that was greater than what urban whites experienced during the 1918 flu pandemic.






Similar content being viewed by others
Notes
Using state-level vital statistics, Moehling and Thomasson (2014) found that home nurse visits, spending on health and sanitation, and the establishment of health centers reduced infant mortality between 1924 and 1929.
The complete-count census data cover the decennial censuses from 1900 to 1940 and come from IPUMS-USA at the University of Minnesota (Ruggles et al. 2018). Without the very recent release of complete-count census data with clean city and age variables, our analysis would not have been possible.
For instance, Boustan and Margo (2016) noted that national black life expectancy estimates derived from vital statistics data in the early twentieth century are likely understated because they are based primarily on northern states, whose black residents predominantly lived in cities (see also Logan and Parman 2014).
We were able to minimize errors in our digitization by checking that cause-specific deaths sum to total deaths in each city and each year.
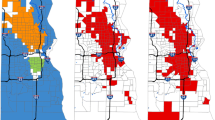
Our own panel ranges from 329 to 982 cities because of data restrictions described later in the article and in the online appendix. In Fig. A4 (online appendix), we map the cities in our sample within their corresponding regions.
The most consequential of these categories is rheumatism and rheumatic fever. In our main results, we exclude these causes, but we reproduce our results with both causes classified as infectious in Fig. A2 in the online appendix. Reassuringly, Fig. A2 is nearly indistinguishable from our main result reported in Fig. 1, panel b. Acute rheumatic fever is the only infectious cause that we exclude even when it is reported separately from noninfectious diseases (chronic rheumatism and gout) because rheumatism and rheumatic fever are reported sometimes separately and sometimes in a combined category and because deaths from these causes combined made up a relatively large share of total deaths. The median death rate from “rheumatism” in 1910, when the category first appears, was 7 per 100,000.
Specifically, we classified the following causes of death as infectious: appendicitis; assorted infectious, epidemic, or parasitic causes; bronchitis, diarrhea, diphtheria, erysipelas, influenza, malaria, measles, meningitis, pneumonia, polio, puerperal fever, scarlet fever, septicemia, small-pox, syphilis, tuberculosis, and whooping cough. Not all of these causes appeared in every year of the vital statistics data we used, and many appeared in multiple variants (e.g., specific forms of tuberculosis).
The ICD provides standardized guidelines for coding causes of death. The first ICD was developed by Jacques Bertillon in 1893 and adopted by many countries. Now called the International Classification of Diseases, it has subsequently been revised many times to incorporate changes in terminology and medical knowledge (Anderson 2011). ICD revisions were implemented uniformly across cities in the vital statistics.
In our series, the southern median urban infectious death rate exceeded the 1900 urban Midwestern median in every year from 1900 to 1920. However, there is a sharp break between 1920 and 1921, in which infectious mortality appeared to fall in all regions, coincident with a change in ICD codes. (For example, meningitis was reported separately before 1921 but collapsed into “all other causes” afterward.) Some of this apparent mortality decline likely reflected the ICD change, although some likely reflected the resurgence of influenza in 1920. We say that the regional difference in 1900 represented “at least” 20 years of the southern mortality decline to come because mortality in all regions might have been higher in years after 1920 absent the ICD change.
We report the sample sizes for all panels in the online appendix. Some cities exited and reentered the full panel over the period.
We centered years relative to the beginning of each period to simplify the interpretation of the coefficients. We saturated the regression model with four region fixed effects rather than include an intercept or the linear trend in year.
The vital statistics report mortality for whites and nonwhites, but in this period, nonwhites overwhelmingly were African American. In all years except 1930–1934, “Mexicans” were classified as white (U. S. Department of Commerce 1941:2). The change in the classification of “Mexicans” had a minimal effect on the nonwhite mortality rates of the North, Midwest, and South. In the West, it causes a spike in nonwhite infectious mortality from 1930 to 1934, visible in panel c of Fig. 4.
According to Troesken (2004), northern and southern cities had similar rates of public water and sewer connections in the early twentieth century.
Although median infectious mortality among African Americans from 1906 to 1920 was higher than that among whites during the flu pandemic, the age pattern in deaths during the flu pandemic was unique. Infectious mortality is usually highest among the very young and the very old, but the flu pandemic killed many people in the prime of their life (Noymer 2009). As discussed earlier, between 1920 and 1921, a change in the coding of causes of death made infectious mortality appear to fall in all groups; median nonwhite comparative mortality ratios were 3.3 in 1920 but 2.4 in 1921, and they remained below 2.8 for the remainder of the series. Some of the infectious mortality decline between 1920 and 1921 likely also reflects the resurgence of influenza in 1920.
Both the racial population shares, \( {\overline{c}}_i^s(t) \) and \( {\overline{c}}_i^n(t) \), and the racial group–specific mortality rates, \( {\overline{m}}_i^s(t) \) and \( {\overline{m}}_i^n(t) \), are calculated as unweighted means across cities.
The racial composition measures were generated from IPUMS population measures, which in some cases generate city population totals that differ from published city population totals. In each city in our racial group–specific sample, these discrepancies never exceed 2.5 % in either direction. When we generated the proportions shown in Fig. 5, we estimated the total regional difference as the sum of the two decomposition terms so that a consistent population size was used in the numerator and denominator of this proportion.
Three cities had infectious mortality among whites in some years from 1906 to 1920 that exceeded median urban white infectious mortality in 1918: Key West, FL (two years), San Antonio, TX (five years), and Asheville, NC (seven years).
Eriksson and Niemesh (2016) found that moving to the North increased the infant mortality rates of African Americans in 1920 but that this effect had disappeared by 1940, mostly because of the disappearance of the urban mortality penalty.
References
Acevedo-Garcia, D. (2000). Residential segregation and the epidemiology of infectious diseases. Social Science & Medicine, 51, 1143–1161.
Alsan, M., & Goldin, C. (2019). Watersheds in child mortality: The role of effective water and sewerage infrastructure, 1880 to 1920. Journal of Political Economy, 127, 586–638.
Anderson, D. M., Charles, K. K., Olivares, C. L. H., & Rees, D. I. (2019). Was the first public health campaign successful? The tuberculosis movement and its effect on mortality. American Economic Journal: Applied Economics, 11(2), 143–175.
Anderson, D. M., Charles, K. K., & Rees, D. (2018). Public health efforts and the decline in urban mortality (NBER Working Paper No. 25027). Cambridge, MA: National Bureau of Economic Research.
Anderson, R. N. (2011). Coding and classifying causes of death: Trends and international differences. In R. G. Rogers & E. M. Crimmins (Eds.), International handbook of adult mortality (pp. 467–489). Dordrecht, the Netherlands: Springer.
Armstrong, G. L., Conn, L. A., & Pinner, R. W. (1999). Trends in infectious disease mortality in the United States during the 20th century. JAMA, 281, 61–66.
Black, D. A., Sanders, S. G., Taylor, E. J., & Taylor, L. J. (2015). The impact of the Great Migration on mortality of African Americans: Evidence from the Deep South. American Economic Review, 105, 477–503.
Boustan, L., & Margo, R. A. (2016). Racial differences in health in the United States: A long-run perspective. In J. Komlos & I. R. Kelly (Eds.), The Oxford handbook of economics and human biology (pp. 730–750). Oxford, UK: Oxford University Press.
Cain, L., & Hong, S. C. (2009). Survival in 19th century cities: The larger the city, the smaller your chances. Explorations in Economic History, 46, 450–463.
Carter, S. B., Gartner, S. S., Haines, M. R., Olmstead, A. L., Sutch, R., & Wright, G. (2006). Historical statistics of the United States: Millennial edition (Vol. 3). Cambridge, UK: Cambridge University Press.
Catillon, M., Cutler, D., & Getzen, T. (2018). Two hundred years of health and medical care: The importance of medical care for life expectancy gains (NBER Working Paper No. 25330). Cambridge, MA: National Bureau of Economic Research.
Collins, W. J., & Thomasson, M. A. (2004). The declining contribution of socioeconomic disparities to the racial gap in infant mortality. Southern Economic Journal, 70, 746–776.
Condran, G. A., & Crimmins, E. (1980). Mortality differentials between rural and urban areas of states in the northeast United States, 1890–1900. Journal of Historical Geography, 6, 179–202.
Condran, G. A., & Crimmins-Gardner, E. (1978). Public health measures and mortality in U.S. cities in the late nineteenth century. Human Ecology, 6, 27–54.
Crimmins, E. M., & Condran, G. A. (1983). Mortality variation in U.S. cities in 1900: A two-level explanation by cause of death and underlying factors. Social Science History, 7, 31–59.
Cutler, D., Deaton, A., & Lleras-Muney, A. (2006). The determinants of mortality. Journal of Economic Perspectives, 20(3), 97–120.
Cutler, D., & Miller, G. (2005). The role of public health improvements in health advances: The twentieth-century United States. Demography, 42, 1–22.
Deaton, A. (2013). The great escape: Health, wealth, and the origins of inequality. Princeton, NJ: Princeton University Press.
Du Bois, W. E. B. (1908). The negro American family. Atlanta, GA: Atlanta University Press.
Eriksson, K., & Niemesh, G. T. (2016). Death in the promised land: The Great Migration and black infant mortality (Working paper). Retrieved from https://ssrn.com/abstract=3071053
Ewbank, D. C. (1987). History of black mortality and health before 1940. Milbank Quarterly, 65, 100–128.
Ferrie, J. P., & Troesken, W. (2008). Water and Chicago’s mortality transition, 1850–1925. Explorations in Economic History, 45, 1–16.
Fogel, R. W. (2004). The escape from hunger and premature death, 1700–2100: Europe, America, and the Third World. Cambridge, UK: Cambridge University Press.
Galishoff, S. (1985). Germs know no color line: Black health and public policy in Atlanta, 1900–1918. Journal of the History of Medicine and Allied Sciences, 40, 22–41.
Grigoryeva, A., & Ruef, M. (2015). The historical demography of racial segregation. American Sociological Review, 80, 814–842.
Haines, M. R. (2001). The urban mortality transition in the United States, 1800–1940. Annales de Démographie Historique, 101(1), 33–64.
Haines, M. R. (2006). Vital statistics. In S. B. Carter, S. S. Gartner, M. R. Haines, A. L. Olmstead, R. Sutch, & G. Wright (Eds.), Historical statistics of the United States: Millennial edition (ch. Ab). New York, NY: Cambridge University Press. https://doi.org/10.1017/ISBN-9780511132971.Ab.ESS.01
Higgs, R. (1973). Mortality in rural America, 1870–1920: Estimates and conjectures. Explorations in Economic History, 10, 177–193.
Humphreys, M. (2009). How four once common diseases were eliminated from the American South. Health Affairs, 28, 1734–1744.
International Institute for Vital Registration and Statistics. (1993). Historical development of cause of death statistics (Technical Assistance Report, No. 55). Atlanta, GA: Centers for Disease Control and Prevention.
Jayachandran, S., Lleras-Muney, A., & Smith, K. V. (2010). Modern medicine and the twentieth century decline in mortality: Evidence on the impact of sulfa drugs. American Economic Journal: Applied Economics, 2(2), 118–146.
Kitchens, C. (2013). A dam problem: TVA’s fight against malaria, 1926–1951. Journal of Economic History, 73, 694–724.
Lee, K.-S. (2007). Infant mortality decline in the late 19th and early 20th centuries: The role of market milk. Perspectives in Biology and Medicine, 50, 585–602.
Logan, T. D., & Parman, J. M. (2014). The dynamics of African-American health: A historical perspective. Review of Black Political Economy, 41, 299–318.
McKeown, T., & Record, R. G. (1962). Reasons for the decline of mortality in England and Wales during the nineteenth century. Population Studies, 16, 94–122.
Meeker, E. (1971). The improving health of the United States, 1850–1915. Explorations in Economic History, 9, 353–373.
Melosi, M. V. (1999). The sanitary city: Urban infrastructure in America from colonial times to the present. Baltimore, MD: Johns Hopkins University Press.
Moehling, C. M., & Thomasson, M. A. (2014). Saving babies: The impact of public education programs on infant mortality. Demography, 51, 367–386.
Moriyama, I. M., Loy, R. M., & Robb-Smith, A. H. T. (2011). History of the statistical classification of diseases and causes of death. Hyattsville, MD: National Center for Health Statistics.
Noymer, A. (2009). Testing the influenza-tuberculosis selective mortality hypothesis with Union Army data. Social Science & Medicine, 68, 1599–1608.
Preston, S. H., & Haines, M. R. (1991). Fatal years: Child mortality in late nineteenth-century America. Princeton, NJ: Princeton University Press.
Preston, S. H., Heuveline, P., & Guillot, M. (2000). Demography: Measuring and modeling population processes. Oxford, UK: Blackwell.
Roberts, S. (2009). Infectious fear: Politics, disease, and the health effects of segregation. Chapel Hill: University of North Carolina Press.
Ruggles, S., Flood, S., Goeken, R., Grover, J., Meyer, E., Pacas, J., & Sobek, M. (2018). IPUMS USA: Version 8.0 [Data set]. Minneapolis: Minnesota Population Center, University of Minnesota. https://doi.org/10.18128/D010.V8.0
Sen, A. (1998). Mortality as an indicator of economic success and failure. Economic Journal, 108, 1–25.
Smith, D. W., & Bradshaw, B. S. (2006). Variation in life expectancy during the twentieth century in the United States. Demography, 43, 647–657.
Smith, D. W., & Bradshaw, B. S. (2008). Reduced variation in death rates after introduction of antimicrobial agents. Population Research and Policy Review, 27, 343–351.
Szreter, S. (1988). The importance of social intervention in Britain’s mortality decline c. 1850–1914: A re-interpretation of the role of public health. Social History of Medicine, 1, 1–38.
Troesken, W. (2004). Water, race, and disease. Cambridge, MA: MIT Press.
U.S. Department of Commerce. (1941). Vital statistics of the United States, 1939—Part I: Natality and mortality data for the United States tabulated by place of occurrence with supplemental tables for Hawaii, Puerto Rico, and the Virgin Islands (Report). Washington, DC: United States Government Printing Office.
Zelner, J. L., Muller, C., & Feigenbaum, J. J. (2017). Racial inequality in the annual risk of tuberculosis infection in the United States, 1910–1933. Epidemiology and Infection, 145, 1797–1804.
Acknowledgments
Authorship is alphabetical to reflect equal contributions. We thank Magali Barbieri, Douglas Ewbank, Evan Roberts, Melissa Thomasson, and Jon Zelner for helpful comments. Hero Ashman, Gianluca Russo, and jim saliba provided excellent research assistance. This research was supported by the Robert Wood Johnson Foundation Health & Society Scholars program; the Regents’ Junior Faculty Fellowship at the University of California, Berkeley; and the Minnesota Population Center at the University of Minnesota, Twin Cities, which is funded by a grant from the Eunice Kennedy Shriver National Institute for Child Health and Human Development (P2C HD041023).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feigenbaum, J.J., Muller, C. & Wrigley-Field, E. Regional and Racial Inequality in Infectious Disease Mortality in U.S. Cities, 1900–1948. Demography 56, 1371–1388 (2019). https://doi.org/10.1007/s13524-019-00789-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-019-00789-z