Abstract
Since the mid-1990s, the United States has witnessed a dramatic rise in drug overdose mortality. Educational gradients in life expectancy widened over the same period, and drug overdose likely plays a role in this widening, particularly for non-Hispanic whites. The contemporary drug epidemic is distinctive in terms of its scope, the nature of the substances involved, and its geographic patterning, which influence how it impacts different education groups. I use vital statistics and National Health Interview Survey data to examine the contribution of drug overdose to educational gradients in life expectancy from 1992–2011. I find that over this period, years of life lost due to drug overdose increased for all education groups and for both males and females. The contribution of drug overdose to educational gradients in life expectancy has increased over time and is greater for non-Hispanic whites than for the population as a whole. Drug overdose accounts for a sizable proportion of the increases in educational gradients in life expectancy, particularly at the prime adult ages (ages 30–60), where it accounts for 25 % to 100 % of the widening in educational gradients between 1992 and 2011. Drug overdose mortality has increased more rapidly for females than for males, leading to a gender convergence. These findings shed light on the processes driving recent changes in educational gradients in life expectancy and suggest that effective measures to address the drug overdose epidemic should take into account its differential burden across education groups.


Similar content being viewed by others
Notes
This is related to the release of an abuse-deterrent reformulation of OxyContin in 2010 and significant increases in the availability of cheap, high-grade heroin throughout the United States.
In this article, I focus on the more-educated as one particular group of social elites.
These are deaths for which the underlying cause of death was ICD-9 codes E850–E858, E950.0–E950.5, E962.0, or E980.0–E980.5 prior to 1999 and ICD-10 codes X40–X44, X60–X64, X85, and Y10–Y14 from 1999 onward.
Fewer than 700 accidental poisoning deaths were recorded in the 1986–2004 NHIS files.
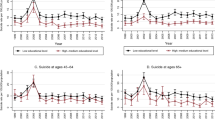
The latter measure is informative because it captures the ages at which drug overdose mortality rates are highest and have increased the most over time (see Fig. 3 in the appendix, with the online version of the article showing the figure in color), and it is less sensitive to issues of age misreporting and changes in institutionalization at older ages.
This is partly related to differences in opioid prescribing by race/ethnicity. Blacks, Hispanics, and Asians are less likely than whites to receive opioid prescriptions, even controlling for pain severity (Burgess et al. 2014; Pletcher et al. 2008). Even if they are prescribed opioids, nonwhites are more likely to live in areas where they cannot obtain them. One study in New York City found that only 25 % of pharmacies in predominantly nonwhite neighborhoods carried sufficient supplies of opioids to treat severe pain compared with 72 % of pharmacies in predominantly white neighborhoods (Morrison et al. 2000).
References
American Pain Society. (1999). Principles of analgesic use in the treatment of acute pain and cancer pain (4th ed.). Glenview, IL: American Pain Society.
Bebinger, M. (2016). FDA considering pricey implant as treatment for opioid addiction. National Public Radio Morning Edition. Retrieved from http://www.npr.org/sections/health-shots/2016/05/20/478577515/fda-considering-pricey-implant-as-treatment-for-opioid-addiction
Becker, J. B., & Hu, M. (2008). Sex differences in drug abuse. Frontiers in Neuroendocrinology, 29, 36–47.
Beltrán-Sánchez, H., Preston, S. H., & Canudas-Romo, V. (2008). An integrated approach to cause-of-death analysis: Cause-deleted life tables and decompositions of life expectancy. Demographic Research, 19(article 35), 1323–1350. doi:10.4054/DemRes.2008.19.35
Bohnert, A. S., Valenstein, M., Bair, M. J., Ganoczy, D., McCarthy, J. F., Ilgen, M. A., & Blow, F. C. (2011). Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA, 305, 1315–1321.
Burgess, D. J., Nelson, D. B., Gravely, A. A., Bair, M. J., Kerns, R. D., Higgins, D. M., . . . Partin, M. R. (2014). Racial differences in prescription of opioid analgesics for chronic noncancer pain in a national sample of veterans. Journal of Pain, 15, 447–455.
Centers for Disease Control and Prevention (CDC), & National Center for Health Statistics (NCHS). (2000/2003). Compressed mortality file 1979–1998 [CDC WONDER On-line Database, Series 20, No. 2A, 2000; & Series 20, No. 2E, 2003]. Retrieved from http://wonder.cdc.gov/cmf-icd9.html
Centers for Disease Control and Prevention (CDC), & National Center for Health Statistics (NCHS). (2015). Compressed mortality file 1999–2014 [CDC WONDER Online Database, Series 20 No. 2T, 2015]. Retrieved from http://wonder.cdc.gov/cmf-icd10.html
Chang, H., Daubresse, M., Kruszewski, S. P., & Alexander, G. C. (2014). Prevalence and treatment of pain in EDs in the United States, 2000 to 2010. American Journal of Emergency Medicine, 32, 421–431.
Chiang, C. L. (1968). An introduction to stochastic processes in biostatistics. New York, NY: Wiley.
Cicero, T. J., Ellis, M. S., Surratt, H. L., & Kurtz, S. P. (2014). The changing face of heroin use in the United States: A retrospective analysis of the past 50 years. JAMA Psychiatry, 71, 821–826.
Collins, R. (2005). Interaction ritual chains. Princeton, NJ: Princeton University Press.
Daubresse, M., Chang, H., Yu, Y., Viswanathan, S., Shah, N. D., Stafford, R. S., . . . Alexander, G. C. (2013). Ambulatory diagnosis and treatment of nonmalignant pain in the United States, 2000–2010. Medical Care, 51, 870–878.
Elo, I., & Preston, S. (1996). Educational differentials in mortality: United States, 1979–1985. Social Science & Medicine, 42, 47–57.
Faul, M., Dailey, M. W., Sugerman, D. E., Sasser, S. M., Levy, B., & Paulozzi, L. J. (2015). Disparity in naloxone administration by emergency medical service providers and the burden of drug overdose in US rural communities. American Journal of Public Health, 105(S3), e26–e32.
Hall, A. J., Logan, J. E., Toblin, R. L., Kaplan, J. A., Kraner, J. C., Bixler, D., . . . Paulozzi, L. J. (2008). Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA, 300, 2613–2620.
Hendi, A. S. (2015). Trends in U.S. life expectancy gradients: The role of changing educational composition. International Journal of Epidemiology, 44, 946–955.
Hendi, A. S. (Forthcoming). Trends in education-specific life expectancy, data quality, and shifting education distributions: A note on recent research. Demography.
Ho, J. Y. (2013). Mortality under age 50 accounts for much of the fact that US life expectancy lags that of other high-income countries. Health Affairs, 32, 459–467.
Ho, J. Y., & Fenelon, A. (2015). The contribution of smoking to educational gradients in U.S. life expectancy. Journal of Health and Social Behavior, 56, 307–322.
Hoyert, D. L., Kochanek, K. D., & Murphy, S. L. (1999). Deaths: Final data for 1997 (National Vital Statistics Reports, No. 47). Hyattsville, MD: National Center for Health Statistics.
International Narcotics Control Board. (2009). Report of the International Narcotics Control Board for 2008 (Report). New York, NY: United Nations.
Jonas, A. B., Young, A. M., Oser, C. B., Leukefeld, C. G., & Havens, J. R. (2012). OxyContin as currency: OxyContin use and increased social capital among rural Appalachian drug users. Social Science & Medicine, 74, 1602–1609.
Jones, C. M., Paulozzi, L. J., & Mack, K. A. (2014). Sources of prescription opioid pain relievers by frequency of past-year nonmedical use: United States, 2008–2011. JAMA Internal Medicine, 174, 802–803.
Kalleberg, A. L. (2011). Good jobs, bad jobs: The rise of polarized and precarious employment systems in the United States, 1970s–2000s. New York, NY: Russell Sage Foundation.
Keyes, K. M., Cerda, M., Brady, J. E., Havens, J. R., & Galea, S. (2014). Understanding the rural-urban differences in nonmedical prescription opioid use and abuse in the United States. American Journal of Public Health, 104(2), e52–e59. doi:10.2105/AJPH.2013.301709
Klaue, K. (1999). Drugs, addiction, deviance and disease as social constructs. Bulletin on Narcotics, LI(1–2), 45–55.
Kochanek, K. D., Murphy, S. L., Xu, J, Q., & Tejada-Vera, B. (2016). Deaths: Final data for 2014 (National Vital Statistics Reports, Vol. 65 No. 4). Hyattsville, MD: National Center for Health Statistics.
Link, B. G., & Phelan, J. C. (1995). Social conditions as fundamental causes of disease. Journal of Health and Social Behavior, 35(Extra issue), 80–94.
McDonald, D. C., & Carlson, K. E. (2013). Estimating the prevalence of opioid diversion by “doctor shoppers” in the United States. PloS One, 8, e69241. doi:10.1371/journal.pone.0069241
Meara, E. R., Richards, S., & Cutler, D. M. (2008). The gap gets bigger: Changes in mortality and life expectancy, by education, 1981–2000. Health Affairs, 27, 350–360.
Miech, R., Pampel, F., Kim, J., & Rogers, R. G. (2011). The enduring association between education and mortality: The role of widening and narrowing disparities. American Sociological Review, 78, 913–934.
Minkler, M., Fuller-Thomson, E., & Guralnik, J. M. (2006). Gradient of disability across the socioeconomic spectrum in the United States. New England Journal of Medicine, 355, 695–703.
Minnesota Population Center, & State Health Access Data Assistance Center. (2015). Integrated Health Interview Series (IHIS): Version 6.12. Minneapolis: University of Minnesota. Retrieved from http://ihis.us/
Morrison, R. S., Wallenstein, S., Natale, D. K., Senzel, R. S., & Huang, L. (2000). “We don’t carry that”—Failure of pharmacies in predominantly nonwhite neighborhoods to stock opioid analgesics. New England Journal of Medicine, 342, 1023–1026.
Muhuri, P. K., Gfroerer, J. C., & Davies, C. (2013). Associations of nonmedical pain reliever use and initiation of heroin use in the United States (CBHSQ Data Review report). Rockville, MD: Substance Abuse and Mental Health Services Administration (SAMHSA).
Musto, D. F. (1991). Opium, cocaine and marijuana in American history. Scientific American, 265(1), 40–47.
Oh, J., & Shin, E. H. (2003). Inequalities in nonfatal work injury: The significance of race, human capital, and occupations. Social Science & Medicine, 57, 2173–2182.
Okie, S. (2010). A flood of opioids, a rising tide of deaths. New England Journal of Medicine, 363, 1981–1985.
Pampel, F. C. (2001). Cigarette diffusion and sex differences in smoking. Journal of Health and Social Behavior, 42, 388–404.
Pampel, F. C., Krueger, P. M., & Denney, J. T. (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349–370.
Paulozzi, L. J., Budnitz, D. S., & Xi, Y. (2006). Increasing deaths from opioid analgesics in the United States. Pharmacoepidemiology and Drug Safety, 15, 618–627.
Paulozzi, L. J., Jones, C. M., Mack, K. A., & Rudd, R. A. (2011). Overdoses of prescription opioid pain relievers—United States, 1999–2008. Morbidity and Mortality Weekly Report, 60, 1487–1492.
Paulozzi, L. J., & Xi, Y. (2008). Recent changes in drug poisoning mortality in the United States by urban–rural status and by drug type. Pharmacoepidemiology and Drug Safety, 17, 997–1005.
Pletcher, M. J., Kertesz, S. G., Kohn, M. A., & Gonzales, R. (2008). Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA, 299, 70–78.
Preston, S. H., Heuveline, P., & Guillot, M. (2001). Demography: Measuring and modeling population processes. Oxford, UK: Blackwell Publishers.
Rigg, K. K., March, S. J., & Inciardi, J. A. (2010). Prescription drug abuse & diversion: Role of the pain clinic. Journal of Drug Issues, 40, 681–702.
Robbins, C. (1989). Sex differences in psychosocial consequences of alcohol and drug abuse. Journal of Health and Social Behavior, 30, 117–130.
Rostron, B. L., Boies, J. L., & Arias, E. (2010). Education reporting and classification on death certificates in the United States (Vital and Health Statistics, Series 2, No. 151). Hyattsville, MD: National Center for Health Statistics.
Rudd, R. A., Aleshire, N., Zibbell, J. E., & Gladden, R. M. (2016). Increases in drug and opioid overdose deaths—United States, 2000–2014. Morbidity and Mortality Weekly Report, 64, 1378–1382.
Seeman, T., Merkin, S. S., Crimmins, E., Koretz, B., Charette, S., & Karlamangla, A. (2008). Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994). Social Science & Medicine, 66, 72–87.
Simoni-Wastila, L., Ritter, G., & Strickler, G. (2004). Gender and other factors associated with the nonmedical use of abusable prescription drugs. Substance Use & Misuse, 39, 1–23.
Sorlie, P. D., & Johnson, N. J. (1996). Validity of education information on the death certificate. Epidemiology, 7, 437–439.
Temple, J. (2015). American pain. Guilford, CT: Lyons Press.
Warner, M., Chen, L. H., Makuc, D. M., Anderson, R. N., and Miniño, A. M. (2011). Drug poisoning deaths in the United States, 1980–2008 (NCHS Data Brief, No. 81). Hyattsville, MD: National Center for Health Statistics.
Weeden, K. A., Kim, Y., Di Carlo, M., & Grusky, D. B. (2007). Social class and earnings inequality. American Behavioral Scientist, 50, 702–736.
Xu, J. Q., Murphy, S. L., Kochanek, K. D., & Bastian, B. A. (2016). Deaths: Final data for 2013 (National Vital Statistics Reports, Vol. 64, No. 2). Hyattsville, MD: National Center for Health Statistics.
Acknowledgments
The author thanks Arun Hendi for helpful comments on earlier drafts of this article. The author is grateful to the National Center for Health Statistics for the use of the restricted-use microdata files for mortality. This research was supported in part by the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD) of the National Institutes of Health under Award Number K99 HD083519.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Age-specific death rates (per 100,000) from drug overdose by education, 1992–1996 and 2007–2011. Estimates are based on data from the CDC/NCHS Multiple Cause-of-Death files (CDC and NCHS 2000/2003, 2015) and the National Health Interview Survey (NHIS). LHS = less than high school, HS = high school, SC = some college, COL = college or more
Rights and permissions
About this article
Cite this article
Ho, J.Y. The Contribution of Drug Overdose to Educational Gradients in Life Expectancy in the United States, 1992–2011. Demography 54, 1175–1202 (2017). https://doi.org/10.1007/s13524-017-0565-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13524-017-0565-3