Abstract
Background
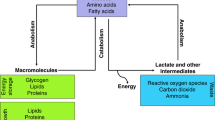
Prostate cancer is the leading cause of cancer in men, and its incidence increases with age. Among other risk factors, pre-existing metabolic diseases have been recently linked with prostate cancer, and our current knowledge recognizes prostate cancer as a condition with important metabolic anomalies as well. In malignancies, metabolic disorders are commonly associated with aberrations in mTOR, which is the master regulator of protein synthesis and energetic homeostasis. Although there are reports demonstrating the high dependency of prostate cancer cells for lipid derivatives and even for carbohydrates, the understanding regarding amino acids, and the relationship with the mTOR pathway ultimately resulting in metabolic aberrations, is still scarce.
Conclusions and perspectives
In this review, we briefly provide evidence supporting prostate cancer as a metabolic disease, and discuss what is known about mTOR signaling and prostate cancer. Next, we emphasized on the amino acids glutamine, leucine, serine, glycine, sarcosine, proline and arginine, commonly related to prostate cancer, to explore the alterations in their regulatory pathways and to link them with the associated metabolic reprogramming events seen in prostate cancer. Finally, we display potential therapeutic strategies for targeting mTOR and the referred amino acids, as experimental approaches to selectively attack prostate cancer cells.




Similar content being viewed by others
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- PCa:
-
Prostate cancer
- PSA:
-
Prostate serum antigen
- ADT:
-
Androgen deprivation therapy
- AR:
-
Androgenic receptor
- CRPC:
-
Castration-resistant prostate cancer
- BMI:
-
Body mass index
- TCA:
-
Tricarboxylic acid
- OXPHOS:
-
Oxidative phosphorylation
- MR:
-
Magnetic resonance
- HFD:
-
High fat diet
- α-KG:
-
α-Ketoglutarate
- PIN:
-
Prostatic intraepithelial neoplasia
- GLUT:
-
Glucose transporter
- HK:
-
Hexokinase
- OCR:
-
Oxygen consumption rate
- ATP:
-
Adenosine triphosphate
- SREBP:
-
Sterol regulatory element binding protein
- ROS:
-
Reactive oxygen species
- mTOR:
-
Mammalian target of rapamycin
- AMPK:
-
AMP-activated protein kinase
- mTORC1:
-
mTOR complex 1
- mTORC2:
-
mTOR complex 2
- RAPTOR:
-
Rapamycin-sensitive adaptor protein of mTOR
- RICTOR:
-
Rapamycin-insensitive companion of mTOR
- 4E-BP1:
-
Eukaryotic initiation factor 4E binding protein 1
- p70-S6K:
-
P70 S6 kinase
- PDCD4:
-
Programmed cell death 4
- PKM2:
-
Pyruvate kinase M2
- SGK:
-
Serum glucose kinase
- PKC:
-
Protein kinase C
- PKB:
-
Protein kinase B
- TSC:
-
Tuberous sclerosis complex
- PDPK1:
-
Phosphoinositide-dependent protein kinase 1
- PPP:
-
Pentose phosphate pathway
- TCGA:
-
The Cancer Genome Atlas
- FASN:
-
Fatty acid synthase
- GDPH:
-
Glycerophosphate dehydrogenase
- GS:
-
Glutamine synthetase
- GLS:
-
Glutaminase
- GAC:
-
Glutaminase C
- GAB:
-
Glutaminase B
- GLUD1:
-
Glutamate dehydrogenase 1
- BPH:
-
Benign prostatic hyperplasia
- NAA:
-
N-acetyl aspartate
- NAAG:
-
N-acetyl aspartyl glutamate
- GOT1:
-
Aspartate aminotransferase/glutamic-oxaloacetic transaminase 1
- IDH:
-
Isocitrate dehydrogenase
- EVs:
-
Extracellular vesicles
- BCAA:
-
Branched-chain amino acid
- LRR:
-
Leucine-rich repeat
- LAT:
-
L-type amino acid transporter
- POV1:
-
Prostate cancer overexpressed gene 1
- p-AKT:
-
Phosphorylated AKT
- IFN:
-
Interferon
- SLFN5:
-
Schlafen family member 5
- ATF4:
-
Activating transcription factor 4
- SILAC:
-
Stable isotope labeling by amino acids in cell culture
- FDA:
-
Food and Drug Administration
- BCATS:
-
Branched-chain aminotransferases
- SGCOP:
-
Serine, glycine, one carbon pathway
- SAM:
-
S-adenosylmethionine
- PSAT1:
-
Phosphoserine aminotransferase 1
- PHGDH:
-
Phosphoglycerate dehydrogenase
- LC-MS:
-
Liquid chromatography-mass spectrometry
- GC-MS:
-
Gas chromatography-mass spectrometry
- GNMT:
-
Glycine N-methyltransferase
- P5C:
-
Δ1-Pyrroline-5-carboxylate
- POX:
-
Proline oxidase
- PRODH:
-
Proline dehydrogenase
- LC:
-
Liquid chromatography
- OCT:
-
Ornithine carbamoyl transferase
- ASS1:
-
Argininosuccinate synthetase
- TEAD:
-
Transcriptional enhanced associate domain
- EMT:
-
Epithelial-to-mesenchymal transition
- PRMT5:
-
Protein arginine methyltransferase 5
- CARM1:
-
Coactivator-associated arginine methyltransferase
- PKCλ/ι:
-
PKC lambda/iota
- NEPC:
-
Neuroendocrine prostate cancer
- MAPK:
-
MAP kinase
- ERK:
-
Extracellular signal-regulated protein kinase
- PLCε:
-
Phospholipase epsilon
- PSHP:
-
Phosphoserine phosphatase
- CDK:
-
Cyclin-dependent kinase
- PDX:
-
Patient-derived xenograft
References
N. Kazmi, P. Haycock, K. Tsilidis, B.M. Lynch, T. Truong, R.M. Martin, S.J. Lewis, Practical Consortium CBCP, Appraising causal relationships of dietary, nutritional and physical-activity exposures with overall and aggressive prostate cancer: two-sample Mendelian-randomization study based on 79 148 prostate-cancer cases and 61 106 controls. Int. J. Epidemiol. 49(2), 587–596 (2020). https://doi.org/10.1093/ije/dyz235
L. Pantanowitz, G.M. Quiroga-Garza, L. Bien, R. Heled, D. Laifenfeld, C. Linhart, J. Sandbank, A. Albrecht Shach, V. Shalev, M. Vecsler, P. Michelow, S. Hazelhurst, R. Dhir, An artificial intelligence algorithm for prostate cancer diagnosis in whole slide images of core needle biopsies: a blinded clinical validation and deployment study. Lancet Digit. Health 2(8), e407–e416 (2020). https://doi.org/10.1016/S2589-7500(20)30159-X
W. Bulten, H. Pinckaers, H. van Boven, R. Vink, T. de Bel, B. van Ginneken, J. van der Laak, C. Hulsbergen-van de Kaa, G. Litjens, Automated deep-learning system for Gleason grading of prostate cancer using biopsies: a diagnostic study. Lancet Oncol. 21(2), 233–241 (2020). https://doi.org/10.1016/S1470-2045(19)30739-9
G. Attard, C. Parker, R.A. Eeles, F. Schroder, S.A. Tomlins, I. Tannock, C.G. Drake, J.S. de Bono, Prostate cancer. Lancet 387(10013), 70–82 (2016). https://doi.org/10.1016/S0140-6736(14)61947-4
U. Swami, T.R. McFarland, R. Nussenzveig, N. Agarwal, Advanced prostate cancer: treatment advances and future directions. Trends Cancer 6(8), 702–715 (2020). https://doi.org/10.1016/j.trecan.2020.04.010
K.K. Singh, M.M. Desouki, R.B. Franklin, L.C. Costello, Mitochondrial aconitase and citrate metabolism in malignant and nonmalignant human prostate tissues. Mol. Cancer 5, 14 (2006). https://doi.org/10.1186/1476-4598-5-14
M. Goodman, K.C. Ward, A.O. Osunkoya, M.W. Datta, D. Luthringer, A.N. Young, K. Marks, V. Cohen, J.C. Kennedy, M.J. Haber, M.B. Amin, Frequency and determinants of disagreement and error in gleason scores: a population-based study of prostate cancer. Prostate 72(13), 1389–1398 (2012). https://doi.org/10.1002/pros.22484
T. Palsdottir, T. Nordstrom, A. Karlsson, H. Gronberg, M. Clements, M. Eklund, The impact of different prostate-specific antigen (PSA) testing intervals on Gleason score at diagnosis and the risk of experiencing false-positive biopsy recommendations: a population-based cohort study. BMJ Open 9(3), e027958 (2019). https://doi.org/10.1136/bmjopen-2018-027958
P.H. Gann, Risk factors for prostate cancer. Rev. Urol. 4(Suppl 5), S3–S10 (2002)
D.J. Hazelett, S.K. Rhie, M. Gaddis, C. Yan, D.L. Lakeland, S.G. Coetzee, B.E. Henderson, H. Noushmehr, W. Cozen, Z. Kote-Jarai, R.A. Eeles, D.F. Easton, C.A. Haiman, W. Lu, P.J. Farnham, G.A. Coetzee, Ellipse G-ONc, Practical c, Comprehensive functional annotation of 77 prostate cancer risk loci. PLoS Genet. 10(1), e1004102 (2014). https://doi.org/10.1371/journal.pgen.1004102
Z.E. Stine, Z.E. Walton, B.J. Altman, A.L. Hsieh, C.V. Dang, MYC, metabolism, and cancer. Cancer Discov. 5(10), 1024–1039 (2015). https://doi.org/10.1158/2159-8290.CD-15-0507
D.P. Labbe, G. Zadra, M. Yang, J.M. Reyes, C.Y. Lin, S. Cacciatore, E.M. Ebot, A.L. Creech, F. Giunchi, M. Fiorentino, H. Elfandy, S. Syamala, E.D. Karoly, M. Alshalalfa, N. Erho, A. Ross, E.M. Schaeffer, E.A. Gibb, M. Takhar, R.B. Den, J. Lehrer, R.J. Karnes, S.J. Freedland, E. Davicioni, D.E. Spratt, L. Ellis, J.D. Jaffe, A.V. D’Amico, P.W. Kantoff, J.E. Bradner, L.A. Mucci, J.E. Chavarro, M. Loda, M. Brown, High-fat diet fuels prostate cancer progression by rewiring the metabolome and amplifying the MYC program. Nat. Commun. 10(1), 4358 (2019). https://doi.org/10.1038/s41467-019-12298-z
Y. Yang, Y. Bai, Y. He, Y. Zhao, J. Chen, L. Ma, Y. Pan, M. Hinten, J. Zhang, R.J. Karnes, M. Kohli, J.J. Westendorf, B. Li, R. Zhu, H. Huang, W. Xu, PTEN Loss Promotes Intratumoral Androgen Synthesis and Tumor Microenvironment Remodeling via Aberrant Activation of RUNX2 in Castration-Resistant Prostate Cancer. Clin. Cancer Res. 24(4), 834–846 (2018). https://doi.org/10.1158/1078-0432.CCR-17-2006
R. Soundararajan, A.M. Aparicio, C.J. Logothetis, S.A. Mani, S.N. Maity, Function of tumor suppressors in resistance to antiandrogen therapy and luminal epithelial plasticity of aggressive variant neuroendocrine prostate cancers. Front. Oncol. 8, 69 (2018). https://doi.org/10.3389/fonc.2018.00069
J.M. Lucas, C. Heinlein, T. Kim, S.A. Hernandez, M.S. Malik, L.D. True, C. Morrissey, E. Corey, B. Montgomery, E. Mostaghel, N. Clegg, I. Coleman, C.M. Brown, E.L. Schneider, C. Craik, J.A. Simon, A. Bedalov, P.S. Nelson, The androgen-regulated protease TMPRSS2 activates a proteolytic cascade involving components of the tumor microenvironment and promotes prostate cancer metastasis. Cancer Discov. 4(11), 1310–1325 (2014). https://doi.org/10.1158/2159-8290.CD-13-1010
M. Reina-Campos, J.F. Linares, A. Duran, T. Cordes, A. L’Hermitte, M.G. Badur, M.S. Bhangoo, P.K. Thorson, A. Richards, T. Rooslid, D.C. Garcia-Olmo, S.Y. Nam-Cha, A.S. Salinas-Sanchez, K. Eng, H. Beltran, D.A. Scott, C.M. Metallo, J. Moscat, M.T. Diaz-Meco, Increased Serine and one-carbon pathway metabolism by PKClambda/iota deficiency promotes neuroendocrine prostate cancer. Cancer Cell 35(3), 385-400 e389 (2019). https://doi.org/10.1016/j.ccell.2019.01.018
D.J. Vander Griend, L. Antony, S.L. Dalrymple, Y. Xu, S.B. Christensen, S.R. Denmeade, J.T. Isaacs, Amino acid containing thapsigargin analogues deplete androgen receptor protein via synthesis inhibition and induce the death of prostate cancer cells. Mol. Cancer Ther. 8(5), 1340–1349 (2009). https://doi.org/10.1158/1535-7163.MCT-08-1136
N.M. Zacharias, C. McCullough, S. Shanmugavelandy, J. Lee, Y. Lee, P. Dutta, J. McHenry, L. Nguyen, W. Norton, L.W. Jones, P.K. Bhattacharya, Metabolic differences in glutamine utilization lead to metabolic vulnerabilities in prostate cancer. Sci. Rep. 7(1), 16159 (2017). https://doi.org/10.1038/s41598-017-16327-z
M.A. Rice, S.V. Malhotra, T. Stoyanova, Second-generation antiandrogens: from discovery to standard of care in castration resistant prostate cancer. Front. Oncol. 9, 801 (2019). https://doi.org/10.3389/fonc.2019.00801
P.L. Martin, J.J. Yin, V. Seng, O. Casey, E. Corey, C. Morrissey, R.M. Simpson, K. Kelly, Androgen deprivation leads to increased carbohydrate metabolism and hexokinase 2-mediated survival in Pten/Tp53-deficient prostate cancer. Oncogene 36(4), 525–533 (2017). https://doi.org/10.1038/onc.2016.223
W. Liu, A. Le, C. Hancock, A.N. Lane, C.V. Dang, T.W. Fan, J.M. Phang, Reprogramming of proline and glutamine metabolism contributes to the proliferative and metabolic responses regulated by oncogenic transcription factor c-MYC. Proc. Natl. Acad. Sci. U. S. A. 109(23), 8983–8988 (2012). https://doi.org/10.1073/pnas.1203244109
J.B. Choi, J.P. Myong, Y. Lee, I. Kim, J.H. Kim, S.H. Hong, U.S. Ha, Does increased body mass index lead to elevated prostate cancer risk? It depends on waist circumference. BMC Cancer 20(1), 589 (2020). https://doi.org/10.1186/s12885-020-07089-5
W.W. Bassett, M.R. Cooperberg, N. Sadetsky, S. Silva, J. DuChane, D.J. Pasta, J.M. Chan, J.W. Anast, P.R. Carroll, C.J. Kane, Impact of obesity on prostate cancer recurrence after radical prostatectomy: data from CaPSURE. Urology 66(5), 1060–1065 (2005). https://doi.org/10.1016/j.urology.2005.05.040
M.R. Smith, F. Saad, B. Egerdie, P.R. Sieber, T.L. Tammela, C. Ke, B.Z. Leder, C. Goessl, Sarcopenia during androgen-deprivation therapy for prostate cancer. J. Clin. Oncol. 30(26), 3271–3276 (2012). https://doi.org/10.1200/JCO.2011.38.8850
A. Lodi, A. Saha, X. Lu, B. Wang, E. Sentandreu, M. Collins, M.G. Kolonin, J. DiGiovanni, S. Tiziani, Combinatorial treatment with natural compounds in prostate cancer inhibits prostate tumor growth and leads to key modulations of cancer cell metabolism. NPJ Precis.Oncol. 1 (2017). https://doi.org/10.1038/s41698-017-0024-z
G. Wang, D. Zhao, D.J. Spring, R.A. DePinho, Genetics and biology of prostate cancer. Genes Dev. 32(17–18), 1105–1140 (2018). https://doi.org/10.1101/gad.315739.118
W.C. Huang, X. Li, J. Liu, J. Lin, L.W. Chung, Activation of androgen receptor, lipogenesis, and oxidative stress converged by SREBP-1 is responsible for regulating growth and progression of prostate cancer cells. Mol. Cancer Res. 10(1), 133–142 (2012). https://doi.org/10.1158/1541-7786.MCR-11-0206
S.L. Ettinger, R. Sobel, T.G. Whitmore, M. Akbari, D.R. Bradley, M.E. Gleave, C.C. Nelson, Dysregulation of sterol response element-binding proteins and downstream effectors in prostate cancer during progression to androgen independence. Cancer Res. 64(6), 2212–2221 (2004). https://doi.org/10.1158/0008-5472.can-2148-2
E. Audet-Walsh, M. Vernier, T. Yee, C. Laflamme, S. Li, Y. Chen, V. Giguere, SREBF1 activity is regulated by an ar/mtor nuclear axis in prostate cancer. Mol. Cancer Res. 16(9), 1396–1405 (2018). https://doi.org/10.1158/1541-7786.MCR-17-0410
D.A. Bader, S.E. McGuire, Tumour metabolism and its unique properties in prostate adenocarcinoma. Nat. Rev. Urol. 17(4), 214–231 (2020). https://doi.org/10.1038/s41585-020-0288-x
M.A. White, C. Lin, K. Rajapakshe, J. Dong, Y. Shi, E. Tsouko, R. Mukhopadhyay, D. Jasso, W. Dawood, C. Coarfa, D.E. Frigo, Glutamine transporters are targets of multiple oncogenic signaling pathways in prostate cancer. Mol. Cancer Res. 15(8), 1017–1028 (2017). https://doi.org/10.1158/1541-7786.MCR-16-0480
V. Strmiska, P. Michalek, T. Eckschlager, M. Stiborova, V. Adam, S. Krizkova, Heger Z (2019) Prostate cancer-specific hallmarks of amino acids metabolism: towards a paradigm of precision medicine. Biochim. Biophys. Acta Rev. Cancer 2, 248–258 (1871). https://doi.org/10.1016/j.bbcan.2019.01.001
L.C. Costello, R.B. Franklin, The intermediary metabolism of the prostate: a key to understanding the pathogenesis and progression of prostate malignancy. Oncology 59(4), 269–282 (2000). https://doi.org/10.1159/000012183
M. Kratochvilova, M. Raudenska, Z. Heger, L. Richtera, N. Cernei, V. Adam, P. Babula, M. Novakova, M. Masarik, J. Gumulec, Amino acid profiling of zinc resistant prostate cancer cell lines: associations with cancer progression. Prostate 77(6), 604–616 (2017). https://doi.org/10.1002/pros.23304
M.M. Desouki, J. Geradts, B. Milon, R.B. Franklin, L.C. Costello, hZip2 and hZip3 zinc transporters are down regulated in human prostate adenocarcinomatous glands. Mol. Cancer 6, 37 (2007). https://doi.org/10.1186/1476-4598-6-37
K. Gonthier, R.T.K. Poluri, E. Audet-Walsh, Functional genomic studies reveal the androgen receptor as a master regulator of cellular energy metabolism in prostate cancer. J. Steroid Biochem. Mol. Biol. 191, 105367 (2019). https://doi.org/10.1016/j.jsbmb.2019.04.016
K.R. Halliday, C. Fenoglio-Preiser, L.O. Sillerud, Differentiation of human tumors from nonmalignant tissue by natural-abundance 13C NMR spectroscopy. Magn. Reson. Med. 7(4), 384–411 (1988). https://doi.org/10.1002/mrm.1910070403
K.D. Tousignant, A. Rockstroh, A. Taherian Fard, M.L. Lehman, C. Wang, S.J. McPherson, L.K. Philp, N. Bartonicek, M.E. Dinger, C.C. Nelson, M.C. Sadowski, Lipid uptake is an androgen-enhanced lipid supply pathway associated with prostate cancer disease progression and bone metastasis. Mol. Cancer Res. 17(5), 1166–1179 (2019). https://doi.org/10.1158/1541-7786.MCR-18-1147
S. Balaban, Z.D. Nassar, A.Y. Zhang, E. Hosseini-Beheshti, M.M. Centenera, M. Schreuder, H.M. Lin, A. Aishah, B. Varney, F. Liu-Fu, L.S. Lee, S.R. Nagarajan, R.F. Shearer, R.A. Hardie, N.L. Raftopulos, M.S. Kakani, D.N. Saunders, J. Holst, L.G. Horvath, L.M. Butler, A.J. Hoy, Extracellular fatty acids are the major contributor to lipid synthesis in prostate cancer. Mol. Cancer Res, 17(4), 949–962 (2019). https://doi.org/10.1158/1541-7786.MCR-18-0347
N. Poulose, F. Amoroso, R.E. Steele, R. Singh, C.W. Ong, I.G. Mills, Genetics of lipid metabolism in prostate cancer. Nat. Genet. 50(2), 169–171 (2018). https://doi.org/10.1038/s41588-017-0037-0
G. Carbonetti, T. Wilpshaar, J. Kroonen, K. Studholme, C. Converso, S. d’Oelsnitz, M. Kaczocha, FABP5 coordinates lipid signaling that promotes prostate cancer metastasis. Sci. Rep. 9(1), 18944 (2019). https://doi.org/10.1038/s41598-019-55418-x
S.J. Kridel, F. Axelrod, N. Rozenkrantz, J.W. Smith, Orlistat is a novel inhibitor of fatty acid synthase with antitumor activity. Cancer Res. 64(6), 2070–2075 (2004). https://doi.org/10.1158/0008-5472.can-03-3645
Q. Wang, C.G. Bailey, C. Ng, J. Tiffen, A. Thoeng, V. Minhas, M.L. Lehman, S.C. Hendy, G. Buchanan, C.C. Nelson, J.E. Rasko, J. Holst, Androgen receptor and nutrient signaling pathways coordinate the demand for increased amino acid transport during prostate cancer progression. Cancer Res. 71(24), 7525–7536 (2011). https://doi.org/10.1158/0008-5472.CAN-11-1821
H.M. Itkonen, S.S. Gorad, D.Y. Duveau, S.E. Martin, A. Barkovskaya, T.F. Bathen, S.A. Moestue, I.G. Mills, Inhibition of O-GlcNAc transferase activity reprograms prostate cancer cell metabolism. Oncotarget 7(11), 12464–12476 (2016). https://doi.org/10.18632/oncotarget.7039
K. Jividen, K.Z. Kedzierska, C.S. Yang, K. Szlachta, A. Ratan, B.M. Paschal, Genomic analysis of DNA repair genes and androgen signaling in prostate cancer. BMC Cancer 18(1), 960 (2018). https://doi.org/10.1186/s12885-018-4848-x
C.E. Massie, A. Lynch, A. Ramos-Montoya, J. Boren, R. Stark, L. Fazli, A. Warren, H. Scott, B. Madhu, N. Sharma, H. Bon, V. Zecchini, D.M. Smith, G.M. Denicola, N. Mathews, M. Osborne, J. Hadfield, S. Macarthur, B. Adryan, S.K. Lyons, K.M. Brindle, J. Griffiths, M.E. Gleave, P.S. Rennie, D.E. Neal, I.G. Mills, The androgen receptor fuels prostate cancer by regulating central metabolism and biosynthesis. EMBO J. 30(13), 2719–2733 (2011). https://doi.org/10.1038/emboj.2011.158
J.L. Gillis, J.A. Hinneh, N.K. Ryan, S. Irani, M. Moldovan, L.E. Quek, R.K. Shrestha, A.R. Hanson, J. Xie, A.J. Hoy, J. Holst, M.M. Centenera, I.G. Mills, D.J. Lynn, L.A. Selth, L.M. Butler, A feedback loop between the androgen receptor and 6-phosphogluoconate dehydrogenase (6PGD) drives prostate cancer growth. Elife 10 (2021). https://doi.org/10.7554/eLife.62592
A.A. Cluntun, M.J. Lukey, R.A. Cerione, J.W. Locasale, Glutamine metabolism in cancer: understanding the heterogeneity. Trends Cancer 3(3), 169–180 (2017). https://doi.org/10.1016/j.trecan.2017.01.005
E.L. Lieu, T. Nguyen, S. Rhyne, J. Kim, Amino acids in cancer. Exp. Mol. Med. 52(1), 15–30 (2020). https://doi.org/10.1038/s12276-020-0375-3
X. Wang, C.G. Proud, The mTOR pathway in the control of protein synthesis. Physiology (Bethesda) 21, 362–369 (2006). https://doi.org/10.1152/physiol.00024.2006
M. Kafri, E. Metzl-Raz, G. Jona, N. Barkai, The Cost of protein production. Cell. Rep. 14(1), 22–31 (2016). https://doi.org/10.1016/j.celrep.2015.12.015
M. Jhanwar-Uniyal, J.V. Wainwright, A.L. Mohan, M.E. Tobias, R. Murali, C.D. Gandhi, M.H. Schmidt, Diverse signaling mechanisms of mTOR complexes: mTORC1 and mTORC2 in forming a formidable relationship. Adv. Biol. Regul. 72, 51–62 (2019). https://doi.org/10.1016/j.jbior.2019.03.003
R.A. Saxton, D.M. Sabatini, mTOR signaling in growth, metabolism, and disease. Cell 168(6), 960–976 (2017). https://doi.org/10.1016/j.cell.2017.02.004
L.C. Kim, R.S. Cook, J. Chen, mTORC1 and mTORC2 in cancer and the tumor microenvironment. Oncogene 36(16), 2191–2201 (2017). https://doi.org/10.1038/onc.2016.363
W.J. Oh, E. Jacinto, mTOR complex 2 signaling and functions. Cell Cycle 10(14), 2305–2316 (2011). https://doi.org/10.4161/cc.10.14.16586
M. Gupta, A.E. Hendrickson, S.S. Yun, J.J. Han, P.A. Schneider, B.D. Koh, M.J. Stenson, L.E. Wellik, J.C. Shing, K.L. Peterson, K.S. Flatten, A.D. Hess, B.D. Smith, J.E. Karp, S. Barr, T.E. Witzig, S.H. Kaufmann, Dual mTORC1/mTORC2 inhibition diminishes Akt activation and induces Puma-dependent apoptosis in lymphoid malignancies. Blood 119(2), 476–487 (2012). https://doi.org/10.1182/blood-2011-04-346601
S.M. Fendt, E.L. Bell, M.A. Keibler, S.M. Davidson, G.J. Wirth, B. Fiske, J.R. Mayers, M. Schwab, G. Bellinger, A. Csibi, A. Patnaik, M.J. Blouin, L.C. Cantley, L. Guarente, J. Blenis, M.N. Pollak, A.F. Olumi, M.G. Vander Heiden, G. Stephanopoulos, Metformin decreases glucose oxidation and increases the dependency of prostate cancer cells on reductive glutamine metabolism. Cancer Res. 73(14), 4429–4438 (2013). https://doi.org/10.1158/0008-5472.CAN-13-0080
C. Magaway, E. Kim, E. Jacinto, Targeting mTOR and Metabolism in Cancer: Lessons and Innovations. Cells 8(12) (2019). https://doi.org/10.3390/cells8121584
D.A. Guertin, D.M. Sabatini, Defining the role of mTOR in cancer. Cancer Cell. 12(1), 9–22 (2007). https://doi.org/10.1016/j.ccr.2007.05.008
L.M. Lindqvist, K. Tandoc, I. Topisirovic, L. Furic, Cross-talk between protein synthesis, energy metabolism and autophagy in cancer. Curr. Opin. Genet. Dev. 48, 104–111 (2018). https://doi.org/10.1016/j.gde.2017.11.003
V. Giguere, DNA-PK, nuclear mTOR, and the androgen pathway in prostate cancer. Trends Cancer 6(4), 337–347 (2020). https://doi.org/10.1016/j.trecan.2020.01.015
N. Hay, The Akt-mTOR tango and its relevance to cancer. Cancer Cell. 8(3), 179–183 (2005). https://doi.org/10.1016/j.ccr.2005.08.008
J. Du, M. Yang, S. Chen, D. Li, Z. Chang, Z. Dong, PDK1 promotes tumor growth and metastasis in a spontaneous breast cancer model. Oncogene 35(25), 3314–3323 (2016). https://doi.org/10.1038/onc.2015.393
K. Masui, W.K. Cavenee, P.S. Mischel, mTORC2 in the center of cancer metabolic reprogramming. Trends Endocrinol. Metab. 25(7), 364–373 (2014). https://doi.org/10.1016/j.tem.2014.04.002
A.C. Hsieh, Y. Liu, M.P. Edlind, N.T. Ingolia, M.R. Janes, A. Sher, E.Y. Shi, C.R. Stumpf, C. Christensen, M.J. Bonham, S. Wang, P. Ren, M. Martin, K. Jessen, M.E. Feldman, J.S. Weissman, K.M. Shokat, C. Rommel, D. Ruggero, The translational landscape of mTOR signalling steers cancer initiation and metastasis. Nature 485(7396), 55–61 (2012). https://doi.org/10.1038/nature10912
E. Audet-Walsh, C.R. Dufour, T. Yee, F.Z. Zouanat, M. Yan, G. Kalloghlian, M. Vernier, M. Caron, G. Bourque, E. Scarlata, L. Hamel, F. Brimo, A.G. Aprikian, J. Lapointe, S. Chevalier, V. Giguere, Nuclear mTOR acts as a transcriptional integrator of the androgen signaling pathway in prostate cancer. Genes Dev. 31(12), 1228–1242 (2017). https://doi.org/10.1101/gad.299958.117
T. Jamaspishvili, D.M. Berman, A.E. Ross, H.I. Scher, A.M. De Marzo, J.A. Squire, T.L. Lotan, Clinical implications of PTEN loss in prostate cancer. Nat. Rev. Urol. 15(4), 222–234 (2018). https://doi.org/10.1038/nrurol.2018.9
H.C. Dan, M.J. Cooper, P.C. Cogswell, J.A. Duncan, J.P. Ting, A.S. Baldwin, Akt-dependent regulation of NF-{kappa}B is controlled by mTOR and Raptor in association with IKK. Genes Dev. 22(11), 1490–1500 (2008). https://doi.org/10.1101/gad.1662308
L. Wang, H. Xiong, F. Wu, Y. Zhang, J. Wang, L. Zhao, X. Guo, L.J. Chang, Y. Zhang, M.J. You, S. Koochekpour, M. Saleem, H. Huang, J. Lu, Y. Deng, Hexokinase 2-mediated Warburg effect is required for PTEN- and p53-deficiency-driven prostate cancer growth. Cell Rep. 8(5), 1461–1474 (2014). https://doi.org/10.1016/j.celrep.2014.07.053
D.A. Guertin, D.M. Stevens, M. Saitoh, S. Kinkel, K. Crosby, J.H. Sheen, D.J. Mullholland, M.A. Magnuson, H. Wu, D.M. Sabatini, mTOR complex 2 is required for the development of prostate cancer induced by Pten loss in mice. Cancer Cell 15(2), 148–159 (2009). https://doi.org/10.1016/j.ccr.2008.12.017
B. Guan, K. Wu, J. Zeng, S. Xu, L. Mu, Y. Gao, K. Wang, Z. Ma, J. Tian, Q. Shi, P. Guo, X. Wang, D. He, Y. Du, Tumor-suppressive microRNA-218 inhibits tumor angiogenesis via targeting the mTOR component RICTOR in prostate cancer. Oncotarget 8(5), 8162–8172 (2017). https://doi.org/10.18632/oncotarget.14131
S.V. Venugopal, S. Caggia, D. Gambrell-Sanders, S.A. Khan, Differential roles and activation of mammalian target of rapamycin complexes 1 and 2 during cell migration in prostate cancer cells. Prostate 80(5), 412–423 (2020). https://doi.org/10.1002/pros.23956
L. Furic, L. Rong, O. Larsson, I.H. Koumakpayi, K. Yoshida, A. Brueschke, E. Petroulakis, N. Robichaud, M. Pollak, L.A. Gaboury, P.P. Pandolfi, F. Saad, N. Sonenberg, eIF4E phosphorylation promotes tumorigenesis and is associated with prostate cancer progression. Proc. Natl. Acad. Sci. U. S. A. 107(32), 14134–14139 (2010). https://doi.org/10.1073/pnas.1005320107
V. Beilsten-Edmands, Y. Gordiyenko, J.C. Kung, S. Mohammed, C. Schmidt, C.V. Robinson, eIF2 interactions with initiator tRNA and eIF2B are regulated by post-translational modifications and conformational dynamics. Cell Discov. 1, 15020 (2015). https://doi.org/10.1038/celldisc.2015.20
H.G. Nguyen, C.S. Conn, Y. Kye, L. Xue, C.M. Forester, J.E. Cowan, A.C. Hsieh, J.T. Cunningham, C. Truillet, F. Tameire, M.J. Evans, C.P. Evans, J.C. Yang, B. Hann, C. Koumenis, P. Walter, P.R. Carroll, D. Ruggero, Development of a stress response therapy targeting aggressive prostate cancer. Sci. Transl. Med. 10(439) (2018). https://doi.org/10.1126/scitranslmed.aar2036
C.L. Amaral, L.B. Freitas, R.E. Tamura, M.R. Tavares, I.C. Pavan, M.C. Bajgelman, F.M. Simabuco, S6Ks isoforms contribute to viability, migration, docetaxel resistance and tumor formation of prostate cancer cells. BMC Cancer 16, 602 (2016). https://doi.org/10.1186/s12885-016-2629-y
A.C. Hsieh, H.G. Nguyen, L. Wen, M.P. Edlind, P.R. Carroll, W. Kim, D. Ruggero, Cell type-specific abundance of 4EBP1 primes prostate cancer sensitivity or resistance to PI3K pathway inhibitors. Sci. Signal 8(403), ra116 (2015). https://doi.org/10.1126/scisignal.aad5111
E.I.J. Lelong, P. Adjibade, F.-H. Joncas, G. Khelifi, V.S-S. Grenier, A. Zoubedi, J.-P. Lambert, P. Toren, R. Mazroui, S.M.I Hussein, Prostate cancer resistance leads to a global deregulation of translation factors and unconventional translation of long non-coding RNAs. bioRxiv:2021.2001.2005.425492 (2021). https://doi.org/10.1101/2021.01.05.425492
V. Cruzat, M. Macedo Rogero, K. Noel Keane, R. Curi, P. Newsholme, Glutamine: Metabolism and Immune Function, Supplementation and Clinical Translation. Nutrients 10(11) (2018). https://doi.org/10.3390/nu10111564
E. Roth, Nonnutritive effects of glutamine. J. Nutr. 138(10), 2025S-2031S (2008). https://doi.org/10.1093/jn/138.10.2025S
M.R. Freeman, J. Kim, M.P. Lisanti, D. Di Vizio, A metabolic perturbation by U0126 identifies a role for glutamine in resveratrol-induced cell death. Cancer Biol. Ther. 12(11), 966–977 (2011). https://doi.org/10.4161/cbt.12.11.18136
P. Newsholme, J. Procopio, M.M. Lima, T.C. Pithon-Curi, R. Curi, Glutamine and glutamate–their central role in cell metabolism and function. Cell Biochem. Funct. 21(1), 1–9 (2003). https://doi.org/10.1002/cbf.1003
M. Stumvoll, G. Perriello, C. Meyer, J. Gerich, Role of glutamine in human carbohydrate metabolism in kidney and other tissues. Kidney Int. 55(3), 778–792 (1999). https://doi.org/10.1046/j.1523-1755.1999.055003778.x
A.M. Shah, F.E. Wondisford, Tracking the carbons supplying gluconeogenesis. J. Biol. Chem. 295(42), 14419–14429 (2020). https://doi.org/10.1074/jbc.REV120.012758
S. Matsumoto, J. Haberle, J. Kido, H. Mitsubuchi, F. Endo, K. Nakamura, Urea cycle disorders-update. J. Hum. Genet. 64(9), 833–847 (2019). https://doi.org/10.1038/s10038-019-0614-4
J.M. Rumberger, T. Wu, M.A. Hering, S. Marshall, Role of hexosamine biosynthesis in glucose-mediated up-regulation of lipogenic enzyme mRNA levels: effects of glucose, glutamine, and glucosamine on glycerophosphate dehydrogenase, fatty acid synthase, and acetyl-CoA carboxylase mRNA levels. J. Biol. Chem. 278(31), 28547–28552 (2003). https://doi.org/10.1074/jbc.M302793200
R. Curi, C.J. Lagranha, S.Q. Doi, D.F. Sellitti, J. Procopio, T.C. Pithon-Curi, M. Corless, P. Newsholme, Molecular mechanisms of glutamine action. J. Cell. Physiol. 204(2), 392–401 (2005). https://doi.org/10.1002/jcp.20339
D.R. Wise, C.B. Thompson, Glutamine addiction: a new therapeutic target in cancer. Trends Biochem. Sci. 35(8), 427–433 (2010). https://doi.org/10.1016/j.tibs.2010.05.003
N. Pissimissis, E. Papageorgiou, P. Lembessis, A. Armakolas, M. Koutsilieris, The glutamatergic system expression in human PC-3 and LNCaP prostate cancer cells. Anticancer Res. 29(1), 371–377 (2009)
Y. Li, X. Li, X. Li, Y. Zhong, Y. Ji, D. Yu, M. Zhang, J.G. Wen, H. Zhang, M.A. Goscinski, J.M. Nesland, Z. Suo, PDHA1 gene knockout in prostate cancer cells results in metabolic reprogramming towards greater glutamine dependence. Oncotarget 7(33), 53837–53852 (2016). https://doi.org/10.18632/oncotarget.10782
V.R. Minciacchi, S. You, C. Spinelli, S. Morley, M. Zandian, P.J. Aspuria, L. Cavallini, C. Ciardiello, M. Reis Sobreiro, M. Morello, G. Kharmate, S.C. Jang, D.K. Kim, E. Hosseini-Beheshti, E. Tomlinson Guns, M. Gleave, Y.S. Gho, S. Mathivanan, W. Yang, M.R. Freeman, D. Di Vizio, Large oncosomes contain distinct protein cargo and represent a separate functional class of tumor-derived extracellular vesicles. Oncotarget 6(13), 11327–11341 (2015). https://doi.org/10.18632/oncotarget.3598
G. Albayrak, E. Konac, A.U. Dikmen, C.Y. Bilen, Memantine induces apoptosis and inhibits cell cycle progression in LNCaP prostate cancer cells. Hum. Exp. Toxicol. 37(9), 953–958 (2018). https://doi.org/10.1177/0960327117747025
A. Schcolnik-Cabrera, A. Chavez-Blanco, G. Dominguez-Gomez, M. Juarez, A. Vargas-Castillo, R.I. Ponce-Toledo, D. Lai, S. Hua, A.R. Tovar, N. Torres, D. Perez-Montiel, J. Diaz-Chavez, A. Duenas-Gonzalez, Pharmacological inhibition of tumor anabolism and host catabolism as a cancer therapy. Sci. Rep. 11(1), 5222 (2021). https://doi.org/10.1038/s41598-021-84538-6
J. Zhang, S. Mao, Y. Guo, Y. Wu, X. Yao, Y. Huang, Inhibition of GLS suppresses proliferation and promotes apoptosis in prostate cancer. Biosci. Rep. 39(6) (2019). https://doi.org/10.1042/BSR20181826
M. Ngollo, A. Lebert, M. Daures, G. Judes, K. Rifai, L. Dubois, J.L. Kemeny, F. Penault-Llorca, Y.J. Bignon, L. Guy, D. Bernard-Gallon, Global analysis of H3K27me3 as an epigenetic marker in prostate cancer progression. BMC Cancer 17(1), 261 (2017). https://doi.org/10.1186/s12885-017-3256-y
M.J. Salji, A. Blomme, J.H.M. Dabritz, P. Repiscak, S. Lilla, R. Patel, D. Sumpton, N.J.F. van den Broek, R. Daly, S. Zanivan, H.Y. Leung, Multi-omics & pathway analysis identify potential roles for tumor N-acetyl aspartate accumulation in murine models of castration-resistant prostate cancer. iScience 25(4), (2022). https://doi.org/10.1016/j.isci.2022.104056
K. Gonthier, R.T.K. Poluri, C. Weidmann, M. Tadros, E. Audet-Walsh, Reprogramming of isocitrate dehydrogenases expression and activity by the androgen receptor in prostate cancer. Mol. Cancer Res. 17(8), 1699–1709 (2019). https://doi.org/10.1158/1541-7786.MCR-19-0020
E. Eidelman, J. Twum-Ampofo, J. Ansari, M.M. Siddiqui, The metabolic phenotype of prostate cancer. Front. Oncol. 7, 131 (2017). https://doi.org/10.3389/fonc.2017.00131
M.J. Lukey, K.F. Wilson, R.A. Cerione, Therapeutic strategies impacting cancer cell glutamine metabolism. Future Med. Chem. 5(14), 1685–1700 (2013). https://doi.org/10.4155/fmc.13.130
M.A. Desbats, I. Giacomini, T. Prayer-Galetti, M. Montopoli, Metabolic plasticity in chemotherapy resistance. Front. Oncol. 10, 281 (2020). https://doi.org/10.3389/fonc.2020.00281
E. Aguilar, I. Marin de Mas, E. Zodda, S. Marin, F. Morrish, V. Selivanov, O. Meca-Cortes, H. Delowar, M. Pons, I. Izquierdo, T. Celia-Terrassa, P. de Atauri, J.J. Centelles, D. Hockenbery, T.M. Thomson, M. Cascante, Metabolic reprogramming and dependencies associated with epithelial cancer stem cells independent of the epithelial-mesenchymal transition program. Stem Cells 34(5), 1163–1176 (2016). https://doi.org/10.1002/stem.2286
J.A. Schneider, S.K. Logan, Revisiting the role of Wnt/beta-catenin signaling in prostate cancer. Mol. Cell. Endocrinol. 462(Pt A), 3–8 (2018). https://doi.org/10.1016/j.mce.2017.02.008
M. Holecek, Branched-chain amino acids in health and disease: metabolism, alterations in blood plasma, and as supplements. Nutr. Metab. (Lond) 15, 33 (2018). https://doi.org/10.1186/s12986-018-0271-1
P.J. Garlick, The role of leucine in the regulation of protein metabolism. J. Nutr. 135(6 Suppl), 1553S-1556S (2005). https://doi.org/10.1093/jn/135.6.1553S
P.J. Atherton, K. Smith, T. Etheridge, D. Rankin, M.J. Rennie, Distinct anabolic signalling responses to amino acids in C2C12 skeletal muscle cells. Amino Acids 38(5), 1533–1539 (2010). https://doi.org/10.1007/s00726-009-0377-x
J. Bella, K.L. Hindle, P.A. McEwan, S.C. Lovell, The leucine-rich repeat structure. Cell. Mol. Life Sci. 65(15), 2307–2333 (2008). https://doi.org/10.1007/s00018-008-8019-0
Z. Pancer, M.D. Cooper, The evolution of adaptive immunity. Annu. Rev. Immunol. 24, 497–518 (2006). https://doi.org/10.1146/annurev.immunol.24.021605.090542
Y. Chen, S. Aulia, L. Li, B.L. Tang, AMIGO and friends: an emerging family of brain-enriched, neuronal growth modulating, type I transmembrane proteins with leucine-rich repeats (LRR) and cell adhesion molecule motifs. Brain Res. Rev. 51(2), 265–274 (2006). https://doi.org/10.1016/j.brainresrev.2005.11.005
E. Liker, E. Fernandez, E. Izaurralde, E. Conti, The structure of the mRNA export factor TAP reveals a cis arrangement of a non-canonical RNP domain and an LRR domain. EMBO J. 19(21), 5587–5598 (2000). https://doi.org/10.1093/emboj/19.21.5587
C.R. Vinson, P.B. Sigler, S.L. McKnight, Scissors-grip model for DNA recognition by a family of leucine zipper proteins. Science 246(4932), 911–916 (1989). https://doi.org/10.1126/science.2683088
J. Sorensen, R. Owenius, M. Lax, S. Johansson, Regional distribution and kinetics of [18F]fluciclovine (anti-[18F]FACBC), a tracer of amino acid transport, in subjects with primary prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 40(3), 394–402 (2013). https://doi.org/10.1007/s00259-012-2291-9
Q. Wang, J. Tiffen, C.G. Bailey, M.L. Lehman, W. Ritchie, L. Fazli, C. Metierre, Y.J. Feng, E. Li, M. Gleave, G. Buchanan, C.C. Nelson, J.E. Rasko, J. Holst, Targeting amino acid transport in metastatic castration-resistant prostate cancer: effects on cell cycle, cell growth, and tumor development. J. Natl. Cancer Inst. 105(19), 1463–1473 (2013). https://doi.org/10.1093/jnci/djt241
B.K. Zhang, A.M. Moran, C.G. Bailey, J.E.J. Rasko, J. Holst, Q. Wang, EGF-activated PI3K/Akt signalling coordinates leucine uptake by regulating LAT3 expression in prostate cancer. Cell. Commun. Signal 17(1), 83 (2019). https://doi.org/10.1186/s12964-019-0400-0
H. Otsuki, T. Kimura, T. Yamaga, T. Kosaka, J.I. Suehiro, H. Sakurai, Prostate cancer cells in different androgen receptor status employ different leucine transporters. Prostate 77(2), 222–233 (2017). https://doi.org/10.1002/pros.23263
R.S. Martinez, M.J. Salji, L. Rushworth, C. Ntala, G. Rodriguez Blanco, A. Hedley, W. Clark, P. Peixoto, E. Hervouet, E. Renaude, S.H.Y. Kung, L.C.A. Galbraith, C. Nixon, S. Lilla, G.M. MacKay, L. Fazli, L. Gaughan, D. Sumpton, M.E. Gleave, S. Zanivan, A. Blomme, H.Y. Leung, SLFN5 regulates LAT1-mediated mTOR activation in castration-resistant prostate cancer. Cancer Res. 81(13), 3664–3678 (2021). https://doi.org/10.1158/0008-5472.CAN-20-3694
A. Sreekumar, L.M. Poisson, T.M. Rajendiran, A.P. Khan, Q. Cao, J. Yu, B. Laxman, R. Mehra, R.J. Lonigro, Y. Li, M.K. Nyati, A. Ahsan, S. Kalyana-Sundaram, B. Han, X. Cao, J. Byun, G.S. Omenn, D. Ghosh, S. Pennathur, D.C. Alexander, A. Berger, J.R. Shuster, J.T. Wei, S. Varambally, C. Beecher, A.M. Chinnaiyan, Metabolomic profiles delineate potential role for sarcosine in prostate cancer progression. Nature 457(7231), 910–914 (2009). https://doi.org/10.1038/nature07762
K. Bouchelouche, S.T. Tagawa, S.J. Goldsmith, B. Turkbey, J. Capala, P. Choyke, PET/CT imaging and radioimmunotherapy of prostate cancer. Semin. Nucl. Med. 41(1), 29–44 (2011). https://doi.org/10.1053/j.semnuclmed.2010.08.005
A. Turpin, E. Girard, C. Baillet, D. Pasquier, J. Olivier, A. Villers, P. Puech, N. Penel, Imaging for metastasis in prostate cancer: a review of the literature. Front. Oncol. 10, 55 (2020). https://doi.org/10.3389/fonc.2020.00055
K.L. Wallitt, S.R. Khan, S. Dubash, H.H. Tam, S. Khan, T.D. Barwick, Clinical PET imaging in prostate cancer. Radiographics 37(5), 1512–1536 (2017). https://doi.org/10.1148/rg.2017170035
Y. Song, J. Li, H.D. Shin, G. Du, L. Liu, J. Chen, One-step biosynthesis of alpha-ketoisocaproate from L-leucine by an Escherichia coli whole-cell biocatalyst expressing an L-amino acid deaminase from Proteus vulgaris. Sci. Rep. 5, 12614 (2015). https://doi.org/10.1038/srep12614
K.L. Billingsley, J.M. Park, S. Josan, R. Hurd, D. Mayer, E. Spielman-Sun, D.G. Nishimura, J.D. Brooks, D. Spielman, The feasibility of assessing branched-chain amino acid metabolism in cellular models of prostate cancer with hyperpolarized [1-(13)C]-ketoisocaproate. Magn. Reson. Imaging 32(7), 791–795 (2014). https://doi.org/10.1016/j.mri.2014.04.015
A.E. Papathanassiu, J.H. Ko, M. Imprialou, M. Bagnati, P.K. Srivastava, H.A. Vu, D. Cucchi, S.P. McAdoo, E.A. Ananieva, C. Mauro, J. Behmoaras, BCAT1 controls metabolic reprogramming in activated human macrophages and is associated with inflammatory diseases. Nat. Commun. 8, 16040 (2017). https://doi.org/10.1038/ncomms16040
E.A. Ananieva, A.C. Wilkinson, Branched-chain amino acid metabolism in cancer. Curr. Opin. Clin. Nutr. Metab. Care 21(1), 64–70 (2018). https://doi.org/10.1097/MCO.0000000000000430
E. Di Cera, Serine proteases. IUBMB Life 61(5), 510–515 (2009). https://doi.org/10.1002/iub.186
D.M. Blow, J.J. Birktoft, B.S. Hartley, Role of a buried acid group in the mechanism of action of chymotrypsin. Nature 221(5178), 337–340 (1969). https://doi.org/10.1038/221337a0
J.W. Locasale, Serine, glycine and one-carbon units: cancer metabolism in full circle. Nat. Rev. Cancer 13(8), 572–583 (2013). https://doi.org/10.1038/nrc3557
F. Giunchi, M. Fiorentino, M. Loda, The metabolic landscape of prostate cancer. Eur. Urol. Oncol. 2(1), 28–36 (2019). https://doi.org/10.1016/j.euo.2018.06.010
A. Zabala-Letona, A. Arruabarrena-Aristorena, N. Martin-Martin, S. Fernandez-Ruiz, J.D. Sutherland, M. Clasquin, J. Tomas-Cortazar, J. Jimenez, I. Torres, P. Quang, P. Ximenez-Embun, R. Bago, A. Ugalde-Olano, A. Loizaga-Iriarte, I. Lacasa-Viscasillas, M. Unda, V. Torrano, D. Cabrera, S.M. van Liempd, Y. Cendon, E. Castro, S. Murray, A. Revandkar, A. Alimonti, Y. Zhang, A. Barnett, G. Lein, D. Pirman, A.R. Cortazar, L. Arreal, L. Prudkin, I. Astobiza, L. Valcarcel-Jimenez, P. Zuniga-Garcia, I. Fernandez-Dominguez, M. Piva, A. Caro-Maldonado, P. Sanchez-Mosquera, M. Castillo-Martin, V. Serra, N. Beraza, A. Gentilella, G. Thomas, M. Azkargorta, F. Elortza, R. Farras, D. Olmos, A. Efeyan, J. Anguita, J. Munoz, J.M. Falcon-Perez, R. Barrio, T. Macarulla, J.M. Mato, M.L. Martinez-Chantar, C. Cordon-Cardo, A.M. Aransay, K. Marks, J. Baselga, J. Tabernero, P. Nuciforo, B.D. Manning, K. Marjon, A. Carracedo, mTORC1-dependent AMD1 regulation sustains polyamine metabolism in prostate cancer. Nature 547(7661), 109–113 (2017). https://doi.org/10.1038/nature22964
L.M. Duan, J.Y. Liu, C.W. Yu, J.X. Fan, T. Li, J.X. Yang, Y.B. Zheng, F.C. Liu, Z.T. He, H.L. Yuan, X.H. Wu, C.L. Luo, PLCepsilon knockdown prevents serine/glycine metabolism and proliferation of prostate cancer by suppressing YAP. Am. J. Cancer Res. 10(1), 196–210 (2020)
Z. Heger, J. Gumulec, N. Cernei, H. Polanska, M. Raudenska, M. Masarik, T. Eckschlager, M. Stiborova, V. Adam, R. Kizek, Relation of exposure to amino acids involved in sarcosine metabolic pathway on behavior of non-tumor and malignant prostatic cell lines. Prostate 76(7), 679–690 (2016). https://doi.org/10.1002/pros.23159
Y.H. Song, M. Shiota, K. Kuroiwa, S. Naito, Y. Oda, The important role of glycine N-methyltransferase in the carcinogenesis and progression of prostate cancer. Mod. Pathol. 24(9), 1272–1280 (2011). https://doi.org/10.1038/modpathol.2011.76
A.P. Khan, T.M. Rajendiran, B. Ateeq, I.A. Asangani, J.N. Athanikar, A.K. Yocum, R. Mehra, J. Siddiqui, G. Palapattu, J.T. Wei, G. Michailidis, A. Sreekumar, A.M. Chinnaiyan, The role of sarcosine metabolism in prostate cancer progression. Neoplasia 15(5), 491–501 (2013). https://doi.org/10.1593/neo.13314
S. Ottaviani, G.N. Brooke, C. O’Hanlon-Brown, J. Waxman, S. Ali, L. Buluwela, Characterisation of the androgen regulation of glycine N-methyltransferase in prostate cancer cells. J. Mol. Endocrinol. 51(3), 301–312 (2013). https://doi.org/10.1530/JME-13-0169
J. Gumulec, M. Raudenska, D. Pacik, M. Plevova, A. Sorokac-Kubolkova, Z. Lackova, N. Cernei, V. Strmiska, O. Zitka, Z. Heger, V. Adam, Post-treatment urinary sarcosine as a predictor of recurrent relapses in patients with prostate cancer. Cancer Med. 7(11), 5411–5419 (2018). https://doi.org/10.1002/cam4.1767
F. Jentzmik, C. Stephan, M. Lein, K. Miller, B. Kamlage, B. Bethan, G. Kristiansen, K. Jung, Sarcosine in prostate cancer tissue is not a differential metabolite for prostate cancer aggressiveness and biochemical progression. J. Urol. 185(2), 706–711 (2011). https://doi.org/10.1016/j.juro.2010.09.077
S. Melnikov, J. Mailliot, L. Rigger, S. Neuner, B.S. Shin, G. Yusupova, T.E. Dever, R. Micura, M. Yusupov, Molecular insights into protein synthesis with proline residues. EMBO Rep. 17(12), 1776–1784 (2016). https://doi.org/10.15252/embr.201642943
M. Levitt, Effect of proline residues on protein folding. J. Mol. Biol. 145(1), 251–263 (1981). https://doi.org/10.1016/0022-2836(81)90342-9
A. Barbul, Proline precursors to sustain Mammalian collagen synthesis. J. Nutr. 138(10), 2021S-2024S (2008). https://doi.org/10.1093/jn/138.10.2021S
C.J. Doillon, M.G. Dunn, E. Bender, F.H. Silver, Collagen fiber formation in repair tissue: development of strength and toughness. Coll. Relat. Res. 5(6), 481–492 (1985). https://doi.org/10.1016/s0174-173x(85)80002-9
C. D’Aniello, E.J. Patriarca, J.M. Phang, G. Minchiotti, Proline metabolism in tumor growth and metastatic progression. Front. Oncol. 10, 776 (2020). https://doi.org/10.3389/fonc.2020.00776
K. Wang, W. Zhang, Z. Wang, M. Gao, X. Wang, W. Han, N. Zhang, X. Xu, Flavokawain A inhibits prostate cancer cells by inducing cell cycle arrest and cell apoptosis and regulating the glutamine metabolism pathway. J. Pharm. Biomed. Anal. 186, 113288 (2020). https://doi.org/10.1016/j.jpba.2020.113288
S.K. Natarajan, W. Zhu, X. Liang, L. Zhang, A.J. Demers, M.C. Zimmerman, M.A. Simpson, D.F. Becker, Proline dehydrogenase is essential for proline protection against hydrogen peroxide-induced cell death. Free Radic. Biol. Med. 53(5), 1181–1191 (2012). https://doi.org/10.1016/j.freeradbiomed.2012.07.002
Z. Heger, N. Cernei, J. Gumulec, M. Masarik, T. Eckschlager, R. Hrabec, O. Zitka, V. Adam, R. Kizek, Determination of common urine substances as an assay for improving prostate carcinoma diagnostics. Oncol. Rep. 31(4), 1846–1854 (2014). https://doi.org/10.3892/or.2014.3054
M. Liu, Y. Wang, C. Yang, Y. Ruan, C. Bai, Q. Chu, Y. Cui, C. Chen, G. Ying, B. Li, Inhibiting both proline biosynthesis and lipogenesis synergistically suppresses tumor growth. J. Exp. Med. 217(3) (2020). https://doi.org/10.1084/jem.20191226
W.D. Sroka, B.A. Boughton, P. Reddy, U. Roessner, P. Slupski, P. Jarzemski, A. Dabrowska, M.J. Markuszewski, M.P. Marszall, Determination of amino acids in urine of patients with prostate cancer and benign prostate growth. Eur. J. Cancer Prev. 26(2), 131–134 (2017). https://doi.org/10.1097/CEJ.0000000000000248
B. Delage, D.A. Fennell, L. Nicholson, I. McNeish, N.R. Lemoine, T. Crook, P.W. Szlosarek, Arginine deprivation and argininosuccinate synthetase expression in the treatment of cancer. Int. J. Cancer 126(12), 2762–2772 (2010). https://doi.org/10.1002/ijc.25202
C.T. Armstrong, P.E. Mason, J.L. Anderson, C.E. Dempsey, Arginine side chain interactions and the role of arginine as a gating charge carrier in voltage sensitive ion channels. Sci. Rep. 6, 21759 (2016). https://doi.org/10.1038/srep21759
M.J. Harms, J.L. Schlessman, G.R. Sue, B. Garcia-Moreno, Arginine residues at internal positions in a protein are always charged. Proc. Natl. Acad. Sci. U. S. A. 108(47), 18954–18959 (2011). https://doi.org/10.1073/pnas.1104808108
C.A. Fitch, G. Platzer, M. Okon, B.E. Garcia-Moreno, L.P. McIntosh, Arginine: Its pKa value revisited. Protein Sci. 24(5), 752–761 (2015). https://doi.org/10.1002/pro.2647
R.C. Blantz, J. Satriano, F. Gabbai, C. Kelly, Biological effects of arginine metabolites. Acta. Physiol. Scand. 168(1), 21–25 (2000). https://doi.org/10.1046/j.1365-201x.2000.00646.x
A.A. Reyes, I.E. Karl, S. Klahr, Role of arginine in health and in renal disease. Am. J. Physiol. 267(3 Pt 2), F331-346 (1994). https://doi.org/10.1152/ajprenal.1994.267.3.F331
E.C. Hsueh, S.M. Knebel, W.H. Lo, Y.C. Leung, P.N. Cheng, C.T. Hsueh, Deprivation of arginine by recombinant human arginase in prostate cancer cells. J. Hematol. Oncol. 5, 17 (2012). https://doi.org/10.1186/1756-8722-5-17
C.L. Chen, S.C. Hsu, T.Y. Chung, C.Y. Chu, H.J. Wang, P.W. Hsiao, S.D. Yeh, D.K. Ann, Y. Yen, H.J. Kung, Arginine is an epigenetic regulator targeting TEAD4 to modulate OXPHOS in prostate cancer cells. Nat. Commun. 12(1), 2398 (2021). https://doi.org/10.1038/s41467-021-22652-9
A. Shukla-Dave, M. Castillo-Martin, M. Chen, J. Lobo, N. Gladoun, A. Collazo-Lorduy, F.M. Khan, V. Ponomarev, Z. Yi, W. Zhang, P.P. Pandolfi, H. Hricak, C. Cordon-Cardo, Ornithine decarboxylase is sufficient for prostate tumorigenesis via androgen receptor signaling. Am. J. Pathol. 186(12), 3131–3145 (2016). https://doi.org/10.1016/j.ajpath.2016.08.021
P.W. Szlosarek, Arginine deprivation and autophagic cell death in cancer. Proc. Natl. Acad. Sci. U. S. A. 111(39), 14015–14016 (2014). https://doi.org/10.1073/pnas.1416560111
X. Deng, G. Shao, H.T. Zhang, C. Li, D. Zhang, L. Cheng, B.D. Elzey, R. Pili, T.L. Ratliff, J. Huang, C.D. Hu, Protein arginine methyltransferase 5 functions as an epigenetic activator of the androgen receptor to promote prostate cancer cell growth. Oncogene 36(9), 1223–1231 (2017). https://doi.org/10.1038/onc.2016.287
I. Dudka, E. Thysell, K. Lundquist, H. Antti, D. Iglesias-Gato, A. Flores-Morales, A. Bergh, P. Wikstrom, G. Grobner, Comprehensive metabolomics analysis of prostate cancer tissue in relation to tumor aggressiveness and TMPRSS2-ERG fusion status. BMC Cancer 20(1), 437 (2020). https://doi.org/10.1186/s12885-020-06908-z
Z. Mounir, J.M. Korn, T. Westerling, F. Lin, C.A. Kirby, M. Schirle, G. McAllister, G. Hoffman, N. Ramadan, A. Hartung, Y. Feng, D.R. Kipp, C. Quinn, M. Fodor, J. Baird, M. Schoumacher, R. Meyer, J. Deeds, G. Buchwalter, T. Stams, N. Keen, W.R. Sellers, M. Brown, R.A. Pagliarini, ERG signaling in prostate cancer is driven through PRMT5-dependent methylation of the Androgen Receptor. Elife 5 (2016). https://doi.org/10.7554/eLife.13964
S. Majumder, Y. Liu, O.H. Ford 3rd., J.L. Mohler, Y.E. Whang, Involvement of arginine methyltransferase CARM1 in androgen receptor function and prostate cancer cell viability. Prostate 66(12), 1292–1301 (2006). https://doi.org/10.1002/pros.20438
O. Alhalabi, A. Naing, R. Groisberg, A. Hahn, S. Zhang, S.C. Berkey, A.M. Tsimberidou, J. Rodon, T.A. Yap, S. Pant, A.Y. Shah, A. Zurita-Saavedra, N. Tannir, F. Meric-Bernstam, V. Subbiah, Phase I study of mTORC1–2 inhibitor sapanisertib (TAK-228) in combination with carboplatin plus paclitaxelin patients with advanced solid malignancies and mTOR pathway alterations [abstract]. Cancer Res. 81(13) (2021). https://doi.org/10.1158/1538-7445.AM2021-CT109
S. Li, J. Sheng, Z. Liu, Y. Fan, C. Zhang, T. Lv, S. Hu, J. Jin, W. Yu, Y. Song, Potent antitumour of the mTORC1/2 dual inhibitor AZD2014 in docetaxel-sensitive and docetaxel-resistant castration-resistant prostate cancer cells. J. Cell. Mol. Med. 25(5), 2436–2449 (2021). https://doi.org/10.1111/jcmm.16155
R.S. Wahdan-Alaswad, K.L. Bane, K. Song, D.T. Shola, J.A. Garcia, D. Danielpour, Inhibition of mTORC1 kinase activates Smads 1 and 5 but not Smad8 in human prostate cancer cells, mediating cytostatic response to rapamycin. Mol. Cancer Res. 10(6), 821–833 (2012). https://doi.org/10.1158/1541-7786.MCR-11-0615
L. Graham, K. Banda, A. Torres, B.S. Carver, Y. Chen, K. Pisano, G. Shelkey, T. Curley, H.I. Scher, T.L. Lotan, A.C. Hsieh, D.E. Rathkopf, A phase II study of the dual mTOR inhibitor MLN0128 in patients with metastatic castration resistant prostate cancer. Invest. New Drugs 36(3), 458–467 (2018). https://doi.org/10.1007/s10637-018-0578-9
F. La Manna, M. De Menna, N. Patel, S. Karkampouna, M.R. De Filippo, I. Klima, P. Kloen, L. Beimers, G.N. Thalmann, R.C.M. Pelger, E. Jacinto, M. Kruithof-de Julio, Dual-mTOR inhibitor rapalink-1 reduces prostate cancer patient-derived xenograft growth and alters tumor heterogeneity. Front. Oncol. 10, 1012 (2020). https://doi.org/10.3389/fonc.2020.01012
Y. Yasumizu, A. Miyajima, T. Kosaka, Y. Miyazaki, E. Kikuchi, M. Oya, Dual PI3K/mTOR inhibitor NVP-BEZ235 sensitizes docetaxel in castration resistant prostate cancer. J. Urol. 191(1), 227–234 (2014). https://doi.org/10.1016/j.juro.2013.07.101
M.S. Neshat, I.K. Mellinghoff, C. Tran, B. Stiles, G. Thomas, R. Petersen, P. Frost, J.J. Gibbons, H. Wu, C.L. Sawyers, Enhanced sensitivity of PTEN-deficient tumors to inhibition of FRAP/mTOR. Proc. Natl. Acad. Sci. U. S. A. 98(18), 10314–10319 (2001). https://doi.org/10.1073/pnas.171076798
A. Mancini, A. Colapietro, S. Pompili, A. Del Fattore, S. Delle Monache, L.A. Biordi, A. Angelucci, V. Mattei, C. Liang, G.L. Gravina, C. Festuccia, Dual PI3 K/mTOR inhibition reduces prostate cancer bone engraftment altering tumor-induced bone remodeling. Tumour Biol. 40(4), (2018). https://doi.org/10.1177/1010428318771773
D.E. Butler, C. Marlein, H.F. Walker, F.M. Frame, V.M. Mann, M.S. Simms, B.R. Davies, A.T. Collins, N.J. Maitland, Inhibition of the PI3K/AKT/mTOR pathway activates autophagy and compensatory Ras/Raf/MEK/ERK signalling in prostate cancer. Oncotarget 8(34), 56698–56713 (2017). https://doi.org/10.18632/oncotarget.18082
L. Xu, Y. Yin, Y. Li, X. Chen, Y. Chang, H. Zhang, J. Liu, J. Beasley, P. McCaw, H. Zhang, S. Young, J. Groth, Q. Wang, J.W. Locasale, X. Gao, D.G. Tang, X. Dong, Y. He, D. George, H. Hu, J. Huang, A glutaminase isoform switch drives therapeutic resistance and disease progression of prostate cancer. Proc. Natl. Acad. Sci. U. S. A. 118(13) (2021). https://doi.org/10.1073/pnas.2012748118
Z. Heger, H. Polanska, M.A. Merlos Rodrigo, R. Guran, P. Kulich, P. Kopel, M. Masarik, T. Eckschlager, M. Stiborova, R. Kizek, V. Adam, Prostate tumor attenuation in the nu/nu murine model due to anti-sarcosine antibodies in folate-targeted liposomes. Sci. Rep. 6, 33379 (2016). https://doi.org/10.1038/srep33379
Y. Yan, L. Chang, H. Tian, L. Wang, Y. Zhang, T. Yang, G. Li, W. Hu, K. Shah, G. Chen, Y. Guo, 1-Pyrroline-5-carboxylate released by prostate Cancer cell inhibit T cell proliferation and function by targeting SHP1/cytochrome c oxidoreductase/ROS Axis. J. Immunother Cancer 6(1), 148 (2018). https://doi.org/10.1186/s40425-018-0466-z
T. Zeng, L. Zhu, M. Liao, W. Zhuo, S. Yang, W. Wu, D. Wang, Knockdown of PYCR1 inhibits cell proliferation and colony formation via cell cycle arrest and apoptosis in prostate cancer. Med. Oncol. 34(2), 27 (2017). https://doi.org/10.1007/s12032-016-0870-5
C.A. Changou, Y.R. Chen, L. Xing, Y. Yen, F.Y. Chuang, R.H. Cheng, R.J. Bold, D.K. Ann, H.J. Kung, Arginine starvation-associated atypical cellular death involves mitochondrial dysfunction, nuclear DNA leakage, and chromatin autophagy. Proc. Natl. Acad. Sci. U. S. A. 111(39), 14147–14152 (2014). https://doi.org/10.1073/pnas.1404171111
B.Y. Shorning, M.S. Dass, M.J. Smalley, H.B. Pearson, The PI3K-AKT-mTOR Pathway and Prostate Cancer: At the Crossroads of AR, MAPK, and WNT Signaling. Int. J. Mol. Sci. 21(12) (2020). https://doi.org/10.3390/ijms21124507
J. Chen, P. Shao, Q. Cao, P. Li, J. Li, H. Cai, J. Zhu, M. Wang, Z. Zhang, C. Qin, C. Yin, Genetic variations in a PTEN/AKT/mTOR axis and prostate cancer risk in a Chinese population. PLoS ONE 7(7), e40817 (2012). https://doi.org/10.1371/journal.pone.0040817
D. Campa, A. Husing, A. Stein, L. Dostal, H. Boeing, T. Pischon, A. Tjonneland, N. Roswall, K. Overvad, J.N. Ostergaard, L. Rodriguez, N. Sala, M.J. Sanchez, N. Larranaga, J.M. Huerta, A. Barricarte, K.T. Khaw, N. Wareham, R.C. Travis, N.E. Allen, P. Lagiou, A. Trichopoulou, D. Trichopoulos, D. Palli, S. Sieri, R. Tumino, C. Sacerdote, H. van Kranen, H.B. Bueno-de-Mesquita, G. Hallmans, M. Johansson, I. Romieu, M. Jenab, D.G. Cox, A. Siddiq, E. Riboli, F. Canzian, R. Kaaks, Genetic variability of the mTOR pathway and prostate cancer risk in the European Prospective Investigation on Cancer (EPIC). PLoS ONE 6(2), e16914 (2011). https://doi.org/10.1371/journal.pone.0016914
B. Bhattacharya, P. Home, A. Ganguly, S. Ray, A. Ghosh, M.R. Islam, V. French, C. Marsh, S. Gunewardena, H. Okae, T. Arima, S. Paul, Atypical protein kinase C iota (PKClambda/iota) ensures mammalian development by establishing the maternal-fetal exchange interface. Proc. Natl. Acad. Sci. U. S. A. 117(25), 14280–14291 (2020). https://doi.org/10.1073/pnas.1920201117
C. Cao, T. Subhawong, J.M. Albert, K.W. Kim, L. Geng, K.R. Sekhar, Y.J. Gi, B. Lu, Inhibition of mammalian target of rapamycin or apoptotic pathway induces autophagy and radiosensitizes PTEN null prostate cancer cells. Cancer Res. 66(20), 10040–10047 (2006). https://doi.org/10.1158/0008-5472.CAN-06-0802
P. Toren, S. Kim, T. Cordonnier, C. Crafter, B.R. Davies, L. Fazli, M.E. Gleave, A. Zoubeidi, Combination AZD5363 with enzalutamide significantly delays enzalutamide-resistant prostate cancer in preclinical models. Eur. Urol. 67(6), 986–990 (2015). https://doi.org/10.1016/j.eururo.2014.08.006
W. Wang, T. Shen, B. Dong, C.J. Creighton, Y. Meng, W. Zhou, Q. Shi, H. Zhou, Y. Zhang, D.D. Moore, F. Yang, MAPK4 overexpression promotes tumor progression via noncanonical activation of AKT/mTOR signaling. J. Clin. Invest. 129(3), 1015–1029 (2019). https://doi.org/10.1172/JCI97712
Z. Lu, S. Xu, ERK1/2 MAP kinases in cell survival and apoptosis. IUBMB Life 58(11), 621–631 (2006). https://doi.org/10.1080/15216540600957438
L. Yuan, X. Sheng, A.K. Willson, D.R. Roque, J.E. Stine, H. Guo, H.M. Jones, C. Zhou, V.L. Bae-Jump, Glutamine promotes ovarian cancer cell proliferation through the mTOR/S6 pathway. Endocr. Relat. Cancer 22(4), 577–591 (2015). https://doi.org/10.1530/ERC-15-0192
N. Floc’h, C.W. Kinkade, T. Kobayashi, A. Aytes, C. Lefebvre, A. Mitrofanova, R.D. Cardiff, A. Califano, M.M. Shen, C. Abate-Shen, Dual targeting of the Akt/mTOR signaling pathway inhibits castration-resistant prostate cancer in a genetically engineered mouse model. Cancer Res. 72(17), 4483–4493 (2012). https://doi.org/10.1158/0008-5472.CAN-12-0283
S.J. Kwon, Y.J. Lee, Effect of low glutamine/glucose on hypoxia-induced elevation of hypoxia-inducible factor-1alpha in human pancreatic cancer MiaPaCa-2 and human prostatic cancer DU-145 cells. Clin. Cancer Res. 11(13), 4694–4700 (2005). https://doi.org/10.1158/1078-0432.CCR-04-2530
L. Sleire, H.E. Forde, I.A. Netland, L. Leiss, B.S. Skeie, P.O. Enger, Drug repurposing in cancer. Pharmacol. Res. 124, 74–91 (2017). https://doi.org/10.1016/j.phrs.2017.07.013
S. Pushpakom, F. Iorio, P.A. Eyers, K.J. Escott, S. Hopper, A. Wells, A. Doig, T. Guilliams, J. Latimer, C. McNamee, A. Norris, P. Sanseau, D. Cavalla, M. Pirmohamed, Drug repurposing: progress, challenges and recommendations. Nat. Rev. Drug Discov. 18(1), 41–58 (2019). https://doi.org/10.1038/nrd.2018.168
D. Juarez-Lopez, A. Schcolnik-Cabrera, Drug repurposing: considerations to surpass while re-directing old compounds for new treatments. Arch. Med. Res. 52(3), 243–251 (2021). https://doi.org/10.1016/j.arcmed.2020.10.021
A. Schcolnik-Cabrera, G. Dominguez-Gomez, A. Duenas-Gonzalez, Comparison of DNA demethylating and histone deacetylase inhibitors hydralazine-valproate versus vorinostat-decitabine incutaneous t-cell lymphoma in HUT78 cells. Am. J. Blood Res. 8(2), 5–16 (2018)
C.K. Singh, M.A. Ndiaye, N. Ahmad, Resveratrol and cancer: challenges for clinical translation. Biochim. Biophys. Acta 1852(6), 1178–1185 (2015). https://doi.org/10.1016/j.bbadis.2014.11.004
W.M. Al-Madhagi, N.M. Hashim, N.A. Awadh Ali, H. Taha, A.A. Alhadi, A.A. Abdullah, O. Sharhan, R. Othman, Bioassay-guided isolation and in silico study of antibacterial compounds from petroleum ether extract of peperomia blanda (Jacq.) Kunth. J. Chem. Inf. Model 59(5), 1858–1872 (2019). https://doi.org/10.1021/acs.jcim.8b00969
Q. Wang, R.A. Hardie, A.J. Hoy, M. van Geldermalsen, D. Gao, L. Fazli, M.C. Sadowski, S. Balaban, M. Schreuder, R. Nagarajah, J.J. Wong, C. Metierre, N. Pinello, N.J. Otte, M.L. Lehman, M. Gleave, C.C. Nelson, C.G. Bailey, W. Ritchie, J.E. Rasko, J. Holst, Targeting ASCT2-mediated glutamine uptake blocks prostate cancer growth and tumour development. J. Pathol. 236(3), 278–289 (2015). https://doi.org/10.1002/path.4518
G. Forlani, G. Sabbioni, D. Ragno, D. Petrollino, M. Borgatti, Phenyl-substituted aminomethylene-bisphosphonates inhibit human P5C reductase and show antiproliferative activity against proline-hyperproducing tumour cells. J. Enzyme Inhib. Med. Chem. 36(1), 1248–1257 (2021). https://doi.org/10.1080/14756366.2021.1919890
Acknowledgements
Alejandro Schcolnik-Cabrera would like to thank the Fonds de Recherche Santé du Québec (FRQS) for the postdoctoral fellowship provided (307595). Daniel Juárez-López would like to thank CONACyT-México for the scholarship provided (388590/288329), and to the Programa de Posgrado en Ciencias Biológicas, Plan de Doctorado en Ciencias Biológicas, UNAM.
Author information
Authors and Affiliations
Contributions
Conceptualization: Alejandro Schcolnik-Cabrera; literature search: Alejandro Schcolnik-Cabrera; writing: Alejandro Schcolnik-Cabrera and Daniel Juárez-López; image preparation: Daniel Juárez-López. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
All authors consented to the publication.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Schcolnik-Cabrera, A., Juárez-López, D. Dual contribution of the mTOR pathway and of the metabolism of amino acids in prostate cancer. Cell Oncol. 45, 831–859 (2022). https://doi.org/10.1007/s13402-022-00706-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13402-022-00706-4