Abstract
Aims
To examine the incidence of interventions for diabetic retinopathy and serious limb complications and to elucidate the patient attributes related to the incidence of each intervention based on real-world claims data from Japan.
Materials and methods
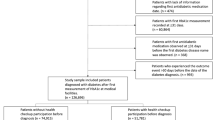
A retrospective longitudinal study design involving a 9 year (2009–2018) claims database obtained from the JMDC Inc. Patients with type 2 diabetes aged 20–74 years taking antidiabetic medications were divided into two groups: “patients with newly initiated antidiabetic medication” (Group 1, n = 47,201) and “patients with continuing antidiabetic medication” (Group 2, n = 82,332). The incidence rate for each intervention was analyzed. We also divided Group 1 into the former and latter periods and investigated temporal changes.
Results
The incidences of the first retinopathy intervention (laser photocoagulation, vitrectomy, or intraocular injection), vitrectomy, and lower-limb amputations in Group 1 were 7.46, 2.37, and 0.31 /1000 person-years, respectively. Those in Group 2 were about 1.2–1.5 times higher. Older age, insulin use, and being dependents rather than insured persons were associated with a higher incidence in both groups after adjustment. While the incidence of the interventions for retinopathy hardly changed during the observation period, that of lower-limb amputations decreased by 40%, with less statistical significance (p = 0.11).
Conclusions
We showed the incidences of the first retinopathy interventions and lower-limb amputations and their secular trends in patients with diabetes, stratified by whether the antidiabetic medication was newly initiated or not. Older age, insulin use, and being dependents were risk factors of these interventions for diabetic complications.

Similar content being viewed by others
References
Lee R, Wong TY, Sabanayagam C. Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond). 2015;2:17. https://doi.org/10.1186/s40662-015-0026-2.
van Netten JJ, Raspovic A, Lavery LA, Monteiro-Soares M, Rasmussen A, Sacco ICN, et al. Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review. Diabetes Metab Res Rev. 2020;36(Suppl 1): e3270. https://doi.org/10.1002/dmrr.3270.
Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990–2010. N Engl J Med. 2014;370(16):1514–23. https://doi.org/10.1056/NEJMoa1310799.
Yamana H, Moriwaki M, Horiguchi H, Kodan M, Fushimi K, Yasunaga H. Validity of diagnoses, procedures, and laboratory data in Japanese administrative data. J Epidemiol. 2017;27(10):476–82. https://doi.org/10.1016/j.je.2016.09.009.
Tanaka H, Sugiyama T, Ihana-Sugiyama N, Ueki K, Kobayashi Y, Ohsugi M. Changes in the quality of diabetes care in Japan between 2007 and 2015: a repeated cross-sectional study using claims data. Diabetes Res Clin Pract. 2019;149:188–99. https://doi.org/10.1016/j.diabres.2019.02.001.
Okumura Y, Sakata N, Takahashi K, Nishi D, Tachimori H. Epidemiology of overdose episodes from the period prior to hospitalization for drug poisoning until discharge in Japan: an exploratory descriptive study using a nationwide claims database. J Epidemiol. 2017;27(8):373–80. https://doi.org/10.1016/j.je.2016.08.010.
Nagai K, Tanaka T, Kodaira N, Kimura S, Takahashi Y, Nakayama T. Data resource profile: JMDC claims database sourced from health insurance societies. J Gen Fam Med. 2021;22(3):118–27. https://doi.org/10.1002/jgf2.422.
Ministry of Health, Labour and Welfare: various information of medical fee. The standard procedure codes. https://shinryohoshu.mhlw.go.jp/shinryohoshu/searchMenu/%3bjsessionid=C712C29505D8F0139F6073C8EB3466E1 (2021). Accessed 16 May 2021
Hara K, Tomio J, Svensson T, Ohkuma R, Svensson AK, Yamazaki T. Association measures of claims-based algorithms for common chronic conditions were assessed using regularly collected data in Japan. J Clin Epidemiol. 2018;99:84–95. https://doi.org/10.1016/j.jclinepi.2018.03.004.
EPHMRA.: EPHMRA anatomical classification guidelines 2018. https://www.ephmra.org/media/1884/atcguidelines2018final.pdf (2018). Accessed 16 May 2021
Okui T, Nojiri C, Kimura S, Abe K, Maeno S, Minami M, et al. Performance evaluation of case definitions of type 1 diabetes for health insurance claims data in Japan. BMC Med Inform Decis Mak. 2021;21(1):52. https://doi.org/10.1186/s12911-021-01422-z.
Chubak J, Pocobelli G, Weiss NS. Tradeoffs between accuracy measures for electronic health care data algorithms. J Clin Epidemiol. 2012;65(3):343-9.e2. https://doi.org/10.1016/j.jclinepi.2011.09.002.
Quan H, Li B, Couris CM, Fushimi K, Graham P, Hider P, et al. Updating and validating the Charlson comorbidity index and score for risk adjustment in hospital discharge abstracts using data from 6 countries. Am J Epidemiol. 2011;173(6):676–82. https://doi.org/10.1093/aje/kwq433.
Mori T, Hamada S, Yoshie S, Jeon B, Jin X, Takahashi H, et al. The associations of multimorbidity with the sum of annual medical and long-term care expenditures in Japan. BMC Geriatr. 2019;19(1):69. https://doi.org/10.1186/s12877-019-1057-7.
Fujita M, Sato Y, Nagashima K, Takahashi S, Hata A. Validity assessment of self-reported medication use by comparing to pharmacy insurance claims. BMJ Open. 2015;5(11): e009490. https://doi.org/10.1136/bmjopen-2015-009490.
Kawasaki R, Tanaka S, Tanaka S, Yamamoto T, Sone H, Ohashi Y, et al. Incidence and progression of diabetic retinopathy in Japanese adults with type 2 diabetes: 8 year follow-up study of the Japan diabetes complications study (JDCS). Diabetologia. 2011;54(9):2288–94. https://doi.org/10.1007/s00125-011-2199-0.
Salinero-Fort M, San Andrés-Rebollo FJ, de Burgos-Lunar C, Arrieta-Blanco FJ, Gómez-Campelo P. Four-year incidence of diabetic retinopathy in a Spanish cohort: the MADIABETES study. PLoS ONE. 2013;8(10): e76417. https://doi.org/10.1371/journal.pone.0076417.
Johannesson A, Larsson GU, Ramstrand N, Turkiewicz A, Wiréhn AB, Atroshi I. Incidence of lower-limb amputation in the diabetic and nondiabetic general population: a 10-year population-based cohort study of initial unilateral and contralateral amputations and reamputations. Diabetes Care. 2009;32(2):275–80. https://doi.org/10.2337/dc08-1639.
Iwase M, Fujii H, Nakamura U, Ohkuma T, Ide H, Jodai-Kitamura T, et al. Incidence of diabetic foot ulcer in Japanese patients with type 2 diabetes mellitus: the Fukuoka diabetes registry. Diabetes Res Clin Pract. 2018;137:183–9. https://doi.org/10.1016/j.diabres.2018.01.020.
Abbott CA, Garrow AP, Carrington AL, Morris J, Van Ross ER, Boulton AJ. Foot ulcer risk is lower in South-Asian and african-Caribbean compared with European diabetic patients in the U.K.: the North-West diabetes foot care study. Diabetes Care. 2005;28(8):1869–75. https://doi.org/10.2337/diacare.28.8.1869.
Kaneko M, Fujihara K, Harada MY, Osawa T, Yamamoto M, Kitazawa M, et al. Rates and risk factors for amputation in people with diabetes in Japan: a historical cohort study using a nationwide claims database. J Foot Ankle Res. 2021;14(1):29. https://doi.org/10.1186/s13047-021-00474-8.
Fukushima S, Nakagami T, Suto C, Hirose A, Uchigata Y. Prevalence of retinopathy and its risk factors in a Japanese population. J Diabetes Investig. 2013;4(4):349–54. https://doi.org/10.1111/jdi.12044.
Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–64. https://doi.org/10.2337/dc11-1909.
Miyajima S, Shirai A, Yamamoto S, Okada N, Matsushita T. Risk factors for major limb amputations in diabetic foot gangrene patients. Diabetes Res Clin Pract. 2006;71(3):272–9. https://doi.org/10.1016/j.diabres.2005.07.005.
Adler AI, Erqou S, Lima TA, Robinson AH. Association between glycated haemoglobin and the risk of lower extremity amputation in patients with diabetes mellitus-review and meta-analysis. Diabetologia. 2010;53(5):840–9. https://doi.org/10.1007/s00125-009-1638-7.
Ministry of Health, Labour and Welfare: report about improvement of consultation rate of dependents. https://www.mhlw.go.jp/stf/shingi/2r9852000001y23e-att/2r9852000001y27x.pdf (2011). Accessed 16 May 2021.
Kume A, Kashiwagi K. Systemic and ocular diseases associated with the development of diabetic macular edema among Japanese patients with diabetes mellitus. BMC Ophthalmol. 2020;20(1):309. https://doi.org/10.1186/s12886-020-01578-8.
Kawasaki R, Konta T, Nishida K. Lipid-lowering medication is associated with decreased risk of diabetic retinopathy and the need for treatment in patients with type 2 diabetes: a real-world observational analysis of a health claims database. Diabetes Obes Metab. 2018;20(10):2351–60. https://doi.org/10.1111/dom.13372.
Sugiyama T, Oba K, Kobayashi Y. Risk-stratified incidence of renal replacement therapy initiation: a longitudinal analysis using medical claims and health checkup data. Tohoku J Exp Med. 2019;248(2):125–35. https://doi.org/10.1620/tjem.248.125.
Yamamoto M, Fujihara K, Ishizawa M, Osawa T, Kaneko M, Ishiguro H, et al. Pulse pressure is a stronger predictor than systolic blood pressure for severe eye diseases in diabetes mellitus. J Am Heart Assoc. 2019;8(8): e010627. https://doi.org/10.1161/jaha.118.010627.
Keech AC, Mitchell P, Summanen PA, O’Day J, Davis TM, Moffitt MS, et al. Effect of fenofibrate on the need for laser treatment for diabetic retinopathy (FIELD study): a randomised controlled trial. Lancet. 2007;370(9600):1687–97. https://doi.org/10.1016/s0140-6736(07)61607-9.
Arya S, Khakharia A, Binney ZO, DeMartino RR, Brewster LP, Goodney PP, et al. Association of statin dose with amputation and survival in patients with peripheral artery disease. Circulation. 2018;137(14):1435–46. https://doi.org/10.1161/circulationaha.117.032361.
Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care. 2008;31(1):99–101. https://doi.org/10.2337/dc07-1178.
Song SJ, Han K, Choi KS, Ko SH, Rhee EJ, Park CY, et al. Trends in diabetic retinopathy and related medical practices among type 2 diabetes patients: results from the National Insurance Service Survey 2006–2013. J Diabetes Investig. 2018;9(1):173–8. https://doi.org/10.1111/jdi.12655.
Boyko EJ, Seelig AD, Ahroni JH. Limb- and person-level risk factors for lower-limb amputation in the prospective seattle diabetic foot study. Diabetes Care. 2018;41(4):891–8. https://doi.org/10.2337/dc17-2210.
Gandhi SK, Waschbusch M, Michael M, Zhang M, Li X, Juhaeri J, et al. Age- and sex-specific incidence of non-traumatic lower limb amputation in patients with type 2 diabetes mellitus in a U.S. claims database. Diabetes Res Clin Practice. 2020;169:108452. https://doi.org/10.1016/j.diabres.2020.108452.
Wright MA, Steffens D, Huilgol RL. Vascular surgery trends in Australia: 2001–2015: less open surgery, less limb loss and more endovascular intervention. ANZ J Surg. 2019;89(4):309–13. https://doi.org/10.1111/ans.14878.
Kamitani F, Nishioka Y, Noda T, Myojin T, Kubo S, Higashino T, et al. Incidence of lower limb amputation in people with and without diabetes: a nationwide 5-year cohort study in Japan. BMJ Open. 2021;11(8): e048436. https://doi.org/10.1136/bmjopen-2020-048436.
Acknowledgements
This study was supported by the Grant of National Center or Global Health and Medicine (26-D-002) and JSPS KAKENHI Grant Number JP19K19451. The JMDC Claims Database was accessible through the contract with the JMDC Inc. The authors complied with the RECORD Statement (Supporting file 8). TS received his salary from University of Tsukuba in FY2018 and FY2019 based on the collaborative research fund between University of Tsukuba and the JMDC Inc (NT was a PI of the research fund), although the present study was not related to the joint research project. The authors instead paid for the database use. The JMDC Inc. did not involve in any of the study design, analysis, and interpretation of data, writing of the report, or any restrictions regarding the submission of the report for publication, while the JMDC Inc. involved in generic data collection (not specific to the present study purpose). UK was at an advisory role at Poxel SA and ERX Pharmaceuticals, received honoraria from Abbott Japan, Novo Nordisk Pharma Ltd., Ono, MSD K.K., Dainihon-Sumitomo, Mitsubishi-Tanabe, Takeda, Kyowa-Kirin, and Daiichi-Sankyo, received research funding from Novo Nordisk Pharam Ltd., Eli Lilly Japan, Nippon Boehringer Ingelheim Co., Ltd, MSD K.K., Abbott Japan, Astellas, Kyowa-Kirin, Dainihon-Sumitomo, Sanofi K.K., and Mitsubishi-Tanabe, and received subsidies or donations from Novo Nordisk Pharma Ltd., Eli Lilly Japan, Astellas, Takeda, and Ono. MO received honoraria from Novartis Pharma, Sanofi K.K., Eli Lilly Japan, and Novo Nordisk Pharma Ltd., received research funding from Novo Nordisk Pharma Ltd, Nippon Boehringer Ingelheim Co., Ltd, Eli Lilly Japan, MSD K.K., Kyowa Kirin, Abbott Japan, and Sanofi K.K., and received subsidies from Sumintomo Dainippon Pharma Co., Ltd., Novartis Pharma, and Mitsubishi Tanabe Pharma Co. TN received research funding from JMDC Inc. (described above) and SMS CO.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Yanagisawa-Sugita, A., Sugiyama, T., Ihana-Sugiyama, N. et al. Incidence of interventions for diabetic retinopathy and serious lower-limb complications and its related factors in patients with type 2 diabetes using a real-world large claims database. Diabetol Int 13, 548–560 (2022). https://doi.org/10.1007/s13340-021-00566-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00566-7