Abstract
Introduction
We tested whether birth weight might be associated with gluteofemoral fat mass and insulin sensitivity later in life.
Materials and methods
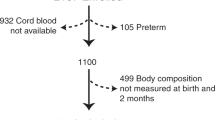
Body size trajectory since birth, body composition at age 20, and markers of insulin resistance were measured in 316 Japanese women. A subset of 148 women underwent a 75 g oral glucose tolerance test. Multiple linear regression analyses were used to identify most important determinants of birth weight.
Results
Birth weight was correlated positively with height and weight at age 12, 15, and 20 years (all p < 0.001 except for weight at 12 years, p = 0.03). Although it showed no correlation with BMI at age 12 and 15, it was correlated positively with current BMI (p = 0.006). It showed positive correlations with lean mass in arms, legs, trunk, and the whole body at age 20 (all p < 0.001). Additionally, it was correlated positively with leg (gluteofemoral) fat mass (p = 0.007), although there was no correlation with total body and trunk fat mass. Furthermore, weight at birth showed inverse correlations with 2-h postglucose insulin concentrations (p = 0.008) whereas it was not correlated with fasting insulin and homeostasis model assessment-insulin resistance. In a multiple regression analysis, which included anthropometric and biochemical variables as independent variables, appendicular muscle mass (standardized β 0.394, p < 0.001) emerged as a single determinant of birth weight (R2 = 0.15). In a model which included gluteofemoral fat mass and 2-h postglucose insulin, birth weight was associated with gluteofemoral fat mass (standardized β 0.240, p = 0.003) and 2-h postglucose insulin concentrations (standardized β − 0.217, p = 0.007) (R2 = 0.09).
Conclusions
Birth weight was associated positively with gluteofemoral fat mass and inversely with 2-h postglucose insulin concentrations, a marker of insulin resistance.

Similar content being viewed by others
Data availability
The ethics committee of the University does not allow us to open data except for a manuscript.
References
Carlsson S, Persson PG, Alvarsson M, et al. Low birth weight, family history of diabetes, and glucose intolerance in Swedish middle-aged men. Diabetes Care. 1999;22:1043–7.
Oya J, Nakagami T, Kurita M, et al. Association of birth weight with diabetes and insulin sensitivity or secretion in the Japanese general population. J Diabetes Investig. 2015;6:430–5.
Katanoda K, Noda M, Goto A, et al. Impact of birth weight on adult-onset diabetes mellitus in relation to current body mass index: The Japan Nurses’ Health Study. J Epidemiol. 2017;27:428–34.
Yokoyama M, Saito I, Ueno M, et al. Low birthweight is associated with type 2 diabetes mellitus in Japanese adults: The Toon Health Study. J Diabetes Investig. 2020;11:1643–50.
Knop MR, Geng TT, Gorny AW, et al. Birth weight and risk of type 2 diabetes mellitus, cardiovascular disease, and hypertension in adults: a meta-analysis of 7 646 267 participants from 135 studies. J Am Heart Assoc. 2018 Dec 4;7(23):e008870.
Harder T, Rodekamp E, Schellong K, et al. Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol. 2007;165:849–57.
Zhao H, Song A, Zhang Y, et al. The association between birth weight and the risk of type 2 diabetes mellitus: a systematic review and meta-analysis. Endocr J. 2018;65:923–33.
Fernandez-Twinn DS, Hjort L, Novakovic B, et al. Intrauterine programming of obesity and type 2 diabetes. Diabetologia. 2019;62:1789–801.
Isganaitis E. Developmental programming of body composition: update on evidence and mechanisms. Curr Diab Rep. 2019;19(8):60.
Wang T, Huang T, Li Y, et al. Low birth weight and risk of type 2 diabetes: a Mendelian randomisation study. Diabetologia. 2016;59:1920–7.
Zanetti D, Tikkanen E, Gustafsson S, et al. Birth weight, type 2 diabetes mellitus, and cardiovascular disease: addressing the Barker hypothesis with Mendelian randomization. Circ Genom Precis Med. 2018 Jun;11(6):e002054.
Zeng P, Zhou X. Causal association between birth weight and adult diseases: evidence from a Mendelian randomization analysis. Front Genet. 2019;10(10):618.
BIRTH-GENE (BIG) Study Working Group. Association of birth weight with type 2 diabetes and glycemic traits: a Mendelian randomization study. JAMA Netw Open. 2019 Sep 4;2(9):e1910915.
Chomtho S, Wells JC, Williams JE, et al. Associations between birth weight and later body composition: evidence from the 4-component model. Am J Clin Nutr. 2008;88:1040–8.
Ylihärsilä H, Kajantie E, Osmond C, et al. Birth size, adult body composition and muscle strength in later life. Int J Obes (Lond). 2007;31:1392–9.
Liu J, Au Yeung SL, He B, et al. The effect of birth weight on body composition: Evidence from a birth cohort and a Mendelian randomization study. PLoS One. 2019 Sep 10;14(9):e0222141.
Son JW, Lee SS, Kim SR, et al. Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES. Diabetologia. 2017;60:865–72.
Scott RA, Fall T, Pasko D, Barker A, et al. Common genetic variants highlight the role of insulin resistance and body fat distribution in type 2 diabetes, independent of obesity. Diabetes. 2014;63:4378–87.
Lotta LA, Gulati P, Day FR, et al. Integrative genomic analysis implicates limited peripheral adipose storage capacity in the pathogenesis of human insulin resistance. Nat Genet. 2017;49:17–26.
Morimoto Y, Maskarinec G, Conroy SM, et al. Asian ethnicity is associated with a higher trunk/peripheral fat ratio in women and adolescent girls. J Epidemiol. 2012;22:130–5.
Ohmi H, Hirooka K, Hata A, et al. Recent trend of increase in proportion of low birth weight infants in Japan. Int J Epidemiol. 2001;30:1269–71.
Honda M, Tsuboi A, Minato-Inokawa S, et al. Reduced birth weight, decreased early-phase insulin secretion, and increased glucose concentrations after oral glucose tolerance test in Japanese women aged 20 years with family history of type 2 diabetes. J Diabetes Res. 2020;14(2020):8822135.
Kitaoka K, Takeuchi M, Tsuboi A, et al. Increased adipose and muscle insulin sensitivity without changes in serum adiponectin in young female collegiate athletes. Metab Syndr Relat Disord. 2017;15:246–51.
Tsuboi A, Minato S, Yano M, et al. Association of serum orosomucoid with 30-min plasma glucose and glucose excursion during oral glucose tolerance tests in non-obese young Japanese women. BMJ Open Diabetes Res Care. 2018 Apr 29;6(1):e000508.
Matthews DR, Hosker JP, Rudenski AS, et al. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412–9.
Kitaoka K, Tsuboi A, Minato-Inokawa S, et al. Determinants and correlates of adipose tissue insulin resistance index in Japanese women without diabetes and obesity. BMJ Open Diabetes Res Care. 2020 Sep;8(1):e001686.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22:1462–70.
Vella CA, Burgos X, Ellis CJ, et al. Associations of insulin resistance with cardiovascular risk factors and inflammatory cytokines in normal-weight Hispanic women. Diabetes Care. 2013;36:1377–83.
Tanaka S, Wu B, Honda M, et al. Associations of lower-body fat mass with favorable profile of lipoproteins and adipokines in healthy, slim women in early adulthood. J Atheroscler Thromb. 2011;18:365–72.
Fernandez-Twinn DS, Hjort L, Novakovic B, et al. Intrauterine programming of obesity and type 2 diabetes. Diabetologia. 2019;62(10):1789–801.
Ravelli AC, van der Meulen JH, Michels RP, et al. Glucose tolerance in adults after prenatal exposure to famine. Lancet. 1998;351:173–7.
Manolopoulos KN, Karpe F, Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond). 2010;34:949–59.
Scott RA, Fall T, Pasko D, et al. Common genetic variants highlight the role of insulin resistance and body fat distribution in type 2 diabetes, independent of obesity. Diabetes. 2014;63:4378–87.
Yaghootkar H, Scott RA, White CC, et al. Genetic evidence for a normal-weight “metabolically obese” phenotype linking insulin resistance, hypertension, coronary artery disease, and type 2 diabetes. Diabetes. 2014;63:4369–77.
Stefan N, Schick F, Häring HU. Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans. Cell Metab. 2017;26:292–300.
Wu B, Huang J, Fukuo K, et al. Different associations of trunk and lower-body fat mass distribution with cardiometabolic risk factors between healthy middle-aged men and women. Int J Endocrinol. 2018;4(2018):1289485.
Lotta LA, Wittemans LBL, Zuber V, et al. Association of genetic variants related to gluteofemoral vs abdominal fat distribution with type 2 diabetes, coronary disease, and cardiovascular risk factors. JAMA. 2018;320:2553–63.
Chen GC, Arthur R, Iyengar NM, et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur Heart J. 2019;40:2849–55.
Virtue S, Vidal-Puig A. Adipose tissue expandability, lipotoxicity and the metabolic syndrome–an allostatic perspective. Biochim Biophys Acta. 2010;1801:338–49.
Smith U, Kahn BB. Adipose tissue regulates insulin sensitivity: role of adipogenesis, de novo lipogenesis and novel lipids. J Intern Med. 2016;280:465–75.
The National Health and Nutrition Survey. Ministry of Health, Labour and Welfare. 2019. Accessed 8 Aug 2021. Welcome to Ministry of Health, Labour and Welfare (mhlw.go.jp)
Luke A. Ethnicity and the BMI-body fat relationship. Br J Nutr. 2009;102:485–7.
Acknowledgements
We thank all participants for their dedicated and conscientious collaboration.
Funding
This research received no specific grant.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no duality of interest associated with this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Honda, M., Tsuboi, A., Minato-Inokawa, S. et al. Birth weight was associated positively with gluteofemoral fat mass and inversely with 2-h postglucose insulin concentrations, a marker of insulin resistance, in young normal-weight Japanese women. Diabetol Int 13, 375–380 (2022). https://doi.org/10.1007/s13340-021-00543-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00543-0