Abstract
Aim
This study aimed to explore the work-related factors related to forgetting to take oral diabetes medication during the working day among Japanese employees with diabetes.
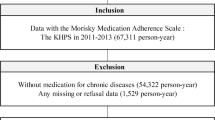
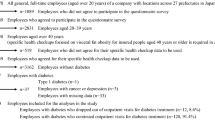
Methods
This worksite-based study was designed to clarify the important work-related factors for preventing the aggravation of diabetes among working-age people and support for coexisting diabetes treatment and work (Ryoritsu Shien). This cross-sectional survey was conducted in 2018. The participants were full-time employees with type 2 diabetes aged over 40 years who took oral diabetes medication during the working day. The participants were classified into forgetting and non-forgetting groups. Their characteristics and work-related factors were evaluated using a self-administered questionnaire and specific health checkup data.
Results
Of the 93 employees with diabetes, 22 (23.7%) were classified into the forgetting group. After adjusting for confounding factors, irregular meal times during the working day was positively associated with forgetting to take oral diabetes medication during the working day [multivariable-adjusted odds ratio (OR), 7.08; 95% confidence interval (CI): 1.38–36.32, irregular vs. regular]. Skipping meals during the working day was positively associated with forgetting to take oral diabetes medication during the working day (multivariable-adjusted OR 3.55, 95% CI 1.14–11.09 presence vs. absence).
Conclusions
Our findings suggest that irregular meal times and skipping meals during the working day are important factors related to forgetting to take oral diabetes medication during the working day among Japanese male employees with diabetes.

Similar content being viewed by others
References
International Diabetes Federation. IDF Diabetes Atlas 9th edition 2019. https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf. Accessed 1 Apr 2021.
Ho PM, Rumsfeld JS, Masoudi FA, McClure DL, Plomondon ME, Steiner JF, et al. Effect of medication nonadherence on hospitalization and mortality among patients with diabetes mellitus. Arch Intern Med. 2006;166:1836–41.
Fukuda H, Mizobe M. Impact of nonadherence on complication risks and healthcare costs in patients newly-diagnosed with diabetes. Diabetes Res Clin Pract. 2017;123:55–62.
Lin LK, Sun Y, Heng BH, Chew DEK, Chong PN. Medication adherence and glycemic control among newly diagnosed diabetes patients. BMJ Open Diabetes Res Care. 2017. https://doi.org/10.1136/bmjdrc-2017-000429.
Ando S, Ito H, Tanaka M, Tsugami E, Araki R, Matsumoto S, et al. The current status and background factors of unused drugs in patients with type 2 diabetes: a cross-sectional study using a questionnaire survey. J Japan Diab Soc. 2018;61:375–81 (in Japanese).
Japan organization of Occupational Health and Safety. Support manual for coexistence of treatment and work for workers with diabetes 2017. https://www.johas.go.jp/Portals/0/data0/kinrosyashien/pdf/bwt-manual-dm01.pdf. Accessed 1 Apr 2021 (in Japanese).
Ministry of Health, Labour and Welfare. Guidelines for supporting coexistence of treatment and work in workplace 2020. https://www.mhlw.go.jp/content/11200000/000614130.pdf. Accessed 1 Apr 2021 (in Japanese).
Kirkman MS, Rowan-Martin MT, Levin R, Fonseca VA, Schmittdiel JA, Herman WH, et al. Determinants of adherence to diabetes medications: findings from a large pharmacy claims database. Diabetes Care. 2015;38:604–9.
Marzec LN, Maddox TM. Medication adherence in patients with diabetes and dyslipidemia: associated factors and strategies for improvement. Curr Cardiol Rep. 2013;15:418.
Sonoda N, Watanabe S, Ohno Y, Godai K, Hatamochi C, Sugimoto Y, et al. Work-related, personal, and diabetes-related factors relevant to dropout from outpatient diabetes treatment visits among Japanese mafle employees with diabetes. Diabetol Int. 2020;11:261–8.
Morimoto A, Watanabe S, Ohno Y, Godai K, Hatamochi C, Sugimoto Y, et al. Associations among work-related stress and mental fatigue, and regular exercise in Japanese employees with or without diabetes. Diabetol Int. 2020;11:105–13.
Kawakami N, Fujigaki Y. Reliability and validity of the Japanese version of job content questionnaire: replication and extension in computer company employees. Ind Health. 1996;34:295–306.
Kawakami N, Kobayashi F, Araki S, Haratani T, Furui H. Assessment of job stress dimensions based on the Job demands-control model of employees of telecommunication and electric power companies in Japan: reliability and validity of the Japanese version of job content questionnaire. Int J Behav Med. 1995;2:358–75.
Chuang LL, Lin KC, Hsu AL, Wu CY, Chang KC, Li YC, et al. Reliability and validity of a vertical numerical rating scale supplemented with a faces rating scale in measuring fatigue after stroke. Health Qual Life Outcomes. 2015;13:91.
Soejima Y, Munemoto T, Masuda A, Uwatoko Y, Miyata M, Tei C. Effects of waon therapy on chronic fatigue syndrome: a pilot study. Intern Med. 2015;54:333–8.
Mendoza TR, Wang XS, Cleeland CS, Morrissey M, Johnson BA, Wendt JK, et al. The rapid assessment of fatigue severity in cancer patients: use of the brief fatigue inventory. Cancer. 1999;88:1186–96.
Tanaka K, Obara T, Kobayashi M, Shinki T, Shibamiya T, Nishimura M, et al. Medication compliance and intentional discontinuation of taking medication among outpatients. J Drug Interact Res. 2009;32:21–7 (in Japanese).
Osanai Y, Katsura S, Sato H, Kimura R, Kodama H, Takasugi K, et al. Evaluation of the factors influencing medicine-taking behavior for the patients taking oral medication. Jpn J Soc Hosp Pharm. 2015;34:72–80 (in Japanese).
Tanaka R, Tsuji M, Kusuhara K, Kawamoto T, Japan Environment and Children’s Study Group. Association between time-related work factors and dietary behaviors: results from the Japan Environment and Children’s Study (JECS). Environ Health Prev Med. 2018. https://doi.org/10.1186/s12199-018-0753-9.
Ministry of Health, Labor and Welfare. An overview of the national health and nutrition survey 2016 Results. https://www.mhlw.go.jp/bunya/kenkou/eiyou/dl/h28-houkoku-03.pdf. Accessed 4 Apr 2021 (in Japanese).
Mallion JM, Schmitt D. Patient compliance in the treatment of arterial hypertension. J Hypertens. 2001;19(12):2281–3.
Kanda K, Okada Y, Morita E, Sugimoto H, Tanaka Y. Problems related to the treatment of working diabetic patient. J Japan Diab Soc. 2005;48:309–15 (in Japanese).
Acknowledgements
This work was supported by a Grant-in-Aid for Scientific Research (B) from the Japan Society for the Promotion of Science (Grant Number: 18H03118).
Author information
Authors and Affiliations
Contributions
NS designed this study, acquired data, performed the data analyses, and wrote the manuscript. SW and YO designed this study, acquired data, performed data interpretation, and contributed to editing the manuscript. CH, YS, MS, and ML performed data interpretation and contributed to editing the manuscript. AM designed this study, acquired data, performed data interpretation, and contributed to editing the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Informed consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the 2013 Declaration of Helsinki. Informed consent or substitute for it was obtained from all patients for being included in this study. The study protocol was written in accordance with the 2013 Declaration of Helsinki and was approved by the Institutional Review Boards of Osaka University (approval date, December 24, 2017; approval no., 17233) and Osaka Prefecture University (approval date, March 2, 2018; approval no., 29–62). Informed consent was obtained from all participants who were included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Sonoda, N., Watanabe, S., Ohno, Y. et al. Work-related factors related to forgetting to take oral diabetes medication during the working day among Japanese male employees with diabetes. Diabetol Int 13, 253–261 (2022). https://doi.org/10.1007/s13340-021-00532-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13340-021-00532-3