Abstract
Introduction
Health2Sync (H2S) is a digital health technology platform that provides coaching and titration support to patients with diabetes. The Mallya cap converts a conventional insulin pen into a smart connected device that can automatically synchronize dose values and associated timestamps (upon injection) to the H2S platform. This single-arm real-world study evaluated the effectiveness of insulin glargine 300 U/mL (Gla-300) combined with H2S and Mallya cap (Gla-300 + Cap + App program) on clinical outcomes among users with type 2 diabetes (T2D) in Taiwan.
Methods
Adults (aged ≥ 20 years) with T2D who were registered H2S users and initiated Mallya cap for a new/existing Gla-300 regimen (identification period May 1, 2021–May 31, 2022) were included in this retrospective cohort study. Follow-up data from H2S were collected for 90 days. Glycated hemoglobin (HbA1c) change (baseline to follow-up) and HbA1c goal attainment were primary outcomes. Hypoglycemia incidence and usage metrics of Mallya cap were secondary outcomes.
Results
Of 83 participants, 38.6% were new Gla-300 users. HbA1c was reduced in both new (− 2.4 [2.7] %, − 26.2 [29.5] mmol/mol) and previous Gla-300 users (− 0.5 [1.6] %, − 5.5 [17.5] mmol/mol). Reduction in HbA1c was significant (p < 0.05) in both groups. At follow-up, 43.4% of users had a reduction of > 0.5%. Mean HbA1c reductions increased numerically with higher baseline HbA1c and with longer duration of Mallya cap usage.
Conclusions
Use of digital technology within a connected ecosystem such as Gla-300 + Cap + App program could help people with type 2 diabetes to improve their glycemic condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Connected digital health ecosystems have the potential to reduce barriers for optimal basal insulin therapy in people with type 2 diabetes. |
We assessed the real-world effectiveness of using insulin glargine 300 units/mL (Gla-300) in conjunction with the Mallya cap and Health2Sync (H2S) app, in people with type 2 diabetes in Taiwan. |
What was learned from the study? |
Glycemic control improved with Gla-300 + Mallya cap + H2S app. |
Using the Mallya cap and H2S app may support diabetes self-care behaviors to improve treatment outcomes in people with type 2 diabetes on basal insulin. |
Introduction
The International Diabetes Federation (IDF) Atlas reported that in 2021, 537 million people had diabetes globally; of these, type 2 diabetes is estimated to account for over 90% of cases [1, 2]. This number is predicted to increase by 46% to 783 million by 2045, with 94% of the rise expected to occur in low- and middle-income countries [1]. In South East Asia, the number of people living with diabetes is expected to increase by approximately 68% during this period, from 90 to 152 million [1]. This substantial change is likely to be driven by several factors, including the increasing westernization of lifestyles and diets, as well as Asian populations having a higher risk of developing diabetes at lower body mass index (BMI) [3, 4]. In Taiwan, the IDF 2021 estimate for the number of people with diabetes was 2.5 million [1]. Previous estimates indicated that the prevalence of type 2 diabetes (T2D) in Taiwan was approximately 0.7 million in 2000 and 1.6 million in 2007, which suggests increasing prevalence of diabetes in Taiwan [5], particularly among people over 65 and under 40 years of age [6].
In a Taiwanese real-world registry study, 836 people with type 2 diabetes with mean baseline HbA1c 10.1% (87.0 mmol/mol) on oral antihyperglycemic drugs were treated with basal insulin (BI) for 24 weeks [7]. Mean HbA1c at 24 weeks was reduced to 8.7% (72.0 mmol/mol), and only 11.9% achieved the target of HbA1c < 7.0% (53.0 mmol/mol). Treatment adherence in the study was high and most participants administered their BI daily. This observation reveals that suboptimal insulin titration may be responsible for the low rate of HbA1c target achievement. A more recent study based on data from the Taiwan Diabetes Registry included participants with T2D diagnosed within 6 months (n = 3297) or with long-term follow-up (n = 1201) [8]. This study reported mean HbA1c values of 8.4% (68.0 mmol/mol) and 7.6% (60.0 mmol/mol), respectively, [8] which suggests that many patients with T2D in Taiwan are still not achieving HbA1c < 7.0% (53.0 mmol/mol) and that further improvements in diabetes management are needed.
Suboptimal insulin titration has been widely observed in patients with T2D, and may reflect patient concerns regarding the risk of hypoglycemia [9, 10]. However, the second-generation BI analogue insulin glargine 300 U/mL (Gla-300) offers a more stable and prolonged pharmacokinetic and pharmacodymamic profile compared with first-generation BI analogues [11], and has been shown to provide lower rates of hypoglycemia (particularly overnight) in Asia Pacific and Japanese populations with T2D [12, 13]. Nevertheless, evidence suggests that Gla-300 is still suboptimally titrated in real-world practice, limiting its clinical potential [14].
Digital health technology and monitoring systems that document the quality of diabetes care can help people with diabetes to manage BI titration, improving glycemic control and clinical outcomes [2, 15]. Health technologies may help reduce the barriers to optimal insulin therapy with connected systems simplifying dose recording and glucose monitoring, which may empower patients in clinical conversations and help to make the connection between insulin use and blood glucose levels [2, 16]. Health2Sync (H2S) is a digital platform that provides diabetes management/self-management functionality, including coaching and titration advice from physicians for patients to follow [17, 18]. Diabetes apps such as H2S can be linked to smart devices such as the Mallya cap, which converts a conventional insulin pen into a connected device that automatically records treatment information (e.g., dose, time/date) [19]. Gla-300 treatment with support from a connected digital ecosystem solution including the H2S app plus Mallya cap may assist patients with their diabetes management. The aim of this study was to evaluate the effectiveness of the Gla-300 + Cap + App program on clinical outcomes among patients with T2D in Taiwan.
Methods
Data Collection
The H2S app and web-based Patient Management platform were used to collect the data from registered users, as has been previously described [20, 21]. Data collected from the H2S app were either entered by healthcare providers along with the measurement timing or synchronized from clinical laboratories, hospitals, or National Health Insurance (NHI) coverage in real time. Data from the H2S app comprised synchronized data from electronic medical records, patient glucose meters, and the Mallya cap, including vitals, lab results, diagnoses, treatment prescriptions, insulin dose, self-monitored blood glucose values, and hypoglycemia incidence, in addition to data that were patient-reported or entered by care providers such as demographics and disease characteristics (diabetes type and duration).
Study Design
This was a retrospective cohort study including users with T2D registered on the H2S app and initiating Mallya cap use for a new or existing Gla-300 regimen. Users were identified between May 1, 2021 and May 31, 2022 and the study period was January 31, 2021 to August 31, 2022. The index date was defined as the date of the first record of insulin dose captured by Mallya cap during the user identification period. The baseline period was up to 90 days prior to the index date, while the follow-up period began on the index date and ended at 90 days after the index date. This study was conducted in accordance with the guidelines for Good Epidemiology Practice and the Declaration of Helsinki. The study was approved by the local Institutional Review Board of the National Taiwan University Hospital (202211018RSC) and Kaohsiung Chang Gung Hospital (202201756B0A3). The study used de-identified data from H2S retrospectively and patients were not recruited specifically for this study. All patients who registered to use the H2S app provided consent for their data to be analyzed for research purposes. Permission was obtained from the owners of H2S to conduct this research using data from the platform.
Study Population
Inclusion criteria were as follows: users with T2D registered on the H2S app who had at least one Mallya cap-synced record during the baseline and follow-up periods (date of the first record as index date) for a new or existing Gla-300 regimen during the user identification period; active Mallya cap use with synced insulin dose records for ≥ 3 days per week for the first 2 weeks after the index date (inclusive); and age ≥ 20 years old at index date. Participants were required to have had at least one HbA1c value (based on hospital or NHI records) in the baseline period through the 14-day post-index period (to allow for capture of HbA1c values for tests that were conducted in the baseline period but reported within 14 days post-index); and at least one HbA1c value (hospital or NHI records) in the 15–90-day post-index follow-up period (plus a 30-day grace period to allow for capture of HbA1c values from tests conducted at the end of the follow-up period). Users whose diabetes status could not be confirmed through International Classification of Diseases 10th Revision (ICD-10) diagnostic codes or self-reported diabetes type information, or those with type 1 diabetes (T1D), were excluded.
Baseline Variables
Key baseline variables in the study were defined as follows. Comorbidities were listed as continuous and categorical variables and defined using the Charlson comorbidity index. Diabetic complications were considered individually. HbA1c value reported was that closest to the index date during the 90-day pre-index and 14-day post-index periods. Fasting blood glucose reported was that obtained closest to the index date during the baseline period. Hypoglycemia incidence was defined as blood glucose value ≤ 70 mg/ dL or at least one ICD-10 code for hypoglycemia during the baseline period. H2S tenure was defined as the interval (in days) between the index date and the first self-reported or synced observation after the app registration date.
Study Outcomes
The primary outcomes were change in HbA1c from baseline to follow-up and HbA1c goal attainment, including the proportion of users that reached the target of 7.0% (< 53.0 mmol/mol) during the follow-up period, and the proportion of users that had a reduction of > 0.5% (5.5 mmol/mol) from baseline to follow-up. Follow-up HbA1c was defined as the value recorded closest to day 90 in the follow-up period. Secondary outcomes included occurrence of hypoglycemia (anytime and nocturnal), and usage metrics for Mallya cap. Nocturnal hypoglycemia was assessed according to two separate time windows (i.e., standard window of 00:00–05:59 and expanded window of 22:00–07:00) and two alternate blood glucose thresholds (i.e., ≤ 70 mg/dL [≤ 3.9 mmol/L] and < 54 mg/dL [3.0 mmol/L]). Duration of Mallya cap use was defined as the difference (in days) between date of last Mallya cap use during follow-up and index date. The mean length of gaps between Mallya cap use was calculated by dividing the number of days of no synced values by the number of gaps in use during follow-up. Mallya cap discontinuation was defined as no synced record for ≥ 28 days following the last synced record during the 90-day follow-up period.
Statistical Analysis
Sample size justification was based on precision estimate (confidence interval for the HbA1c change in 3 months). With expected standard deviation (SD) of 0.9% and expected precision of ± 0.2%, the required sample size was 81. Study variables (including baseline covariates and outcome measures) were analyzed descriptively and are reported for the overall study population. Missing values were categorized as “Unknown/Missing” for categorical variables. Chi-square and t tests were used to evaluate the statistical significance of differences in categorical and continuous variables, respectively. Corresponding p values are reported with a significance level of α = 0.05. Paired t tests were used to evaluate the average change in HbA1c from baseline to follow-up.
The primary endpoint (change in HbA1c) was stratified by prior use of Gla-300, baseline HbA1c category and duration of Mallya cap use (in months). New Gla-300 users were defined as those with a first Gla-300 dose on the index date or within the 14-day period prior to the index date and no Gla-300 use at any time before the 14-day period prior to the index date. Previous Gla-300 users were those whose first Gla-300 dose occurred before the 14-day period prior to the index date.
Results
Study Population
In total, 83 patients with type 2 diabetes were included (Supplementary Fig. 1), of whom 38.6% were new Gla-300 users. Of the 83 patients, 55.4% were male, mean (SD) age at index date was 49.2 (13.1) years and 31.3% had a diabetes duration of > 10 years (Table 1). New Gla-300 users were younger on average (mean [SD] age 45.5 [14.9] versus 51.6 [11.2] years, p = 0.03) and had a shorter duration of diabetes compared with previous users (9.4% versus 45.1% with duration > 10 years). The mean (SD) HbA1c at baseline was 8.4 (2.2) % (68.3 [24.0] mmol/mol) overall, and significantly higher for new Gla-300 users (9.6 [2.3] %, 81.4 [25.1] mmol/mol) versus previous Gla-300 users (7.7 [1.8] %, 60.6 [19.7] mmol/mol, p < 0.01). The mean (SD) total daily BI dose in the baseline period was 18.8 (12.1) units and 19.9 (13.2) units in the new and previous Gla-300 user groups, respectively. In the baseline period, 10 patients (12.0%) experienced hypoglycemia.
HbA1c Change and Goal Attainment
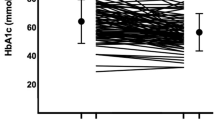
Mean (SD) HbA1c change from baseline to follow-up was − 1.2 (2.3) % (− 13.1 [25.1] mmol/mol) for the total population, − 2.4 (2.7) % (− 26.2 [29.5] mmol/mol) in new Gla-300 users, and − 0.5 (1.6) % (− 5.5 [17.5] mmol/mol) in previous Gla-300 users (Fig. 1a); this change was statistically significant in all groups (p < 0.05). Overall, users with HbA1c ≥ 10.0% (86.0 mmol/mol) at baseline experienced the largest change in HbA1c level in the follow-up period. Similar trends were observed for both new and previous Gla-300 users with larger reductions in HbA1c as baseline HbA1c increased (Supplementary Table 1). For the total population, mean change in HbA1c was greatest with 3 months’ duration of Mallya cap use (− 1.3 [2.1] %, − 14.2 [23.0] mmol/mol) compared with < 2 months (− 1.1 [2.5] %, − 12.0 [27.3] mmol/mol) or 2 to < 3 months (− 1.2 [2.3] %, − 13.1 [25.1] mmol/mol) (Fig. 1b).
Overall, the proportion of users achieving HbA1c < 7.0% (53.0 mmol/mol) increased from 32.5% at baseline to 44.6% at follow-up (Fig. 2a); this increase was mainly in new Gla-300 users, of whom 12.5% had HbA1c < 7.0% (53.0 mmol/mol) at baseline versus 40.6% at follow-up. Stratification by baseline HbA1c showed that the goal of HbA1c < 7.0% (53.0 mmol/mol) at follow-up was achieved by 77.8% of users who had a baseline HbA1c of < 7.0% (53.0 mmol/mol). Among higher-baseline HbA1c groups, target achievement ranged from 18.2% for users with baseline HbA1c of 9.0–9.9% (75.0–85.0 mmol/mol) to 37.5% of users with baseline HbA1c of ≥ 10.0% (86.0 mmol/mol, Supplementary Table 1).
Stratification by Mallya cap use showed that HbA1c < 7.0% (53.0 mmol/mol) at follow-up was achieved by 48.0%, 45.0%, and 42.1% of users with Mallya cap use duration of < 2 months, 2 to < 3 months, and 3 months, respectively (Fig. 2b). No obvious trend in Mallya cap use was observed for new (50.0%, 14.3% and 46.7% at < 2, 2 to < 3 months and 3 months, respectively) or previous Gla-300 users (46.7%, 61.5% and 39.1% at < 2, 2 to < 3 months, and 3 months, respectively).
HbA1c reduction > 0.5% (5.5 mmol/mol) was achieved by 65.6% of new Gla-300 users and 29.4% of previous Gla-300 users (Fig. 3a). The proportion of users with a HbA1c reduction from baseline to follow-up of > 0.5% (5.5 mmol/mol) increased steadily with baseline HbA1c, from 7.4% of users with a baseline HbA1c of < 7.0% (53.0 mmol/mol) achieving this reduction up to 100% of users with a baseline HbA1c ≥ 10.0% (86.0 mmol/mol) achieving this goal (Supplementary Table 1). An HbA1c reduction of > 0.5% (5.5 mmol/mol) was achieved by 36.0%, 40.0%, and 50.0% of users with Mallya cap use duration of < 2 months, 2 to < 3 months, and 3 months, respectively (Fig. 3b). Similar trends were observed for new (60.0%, 57.1%, and 73.3% at < 2, 2 to < 3, and 3 months, respectively) and previous Gla-300 users (20.0%, 30.8%, and 34.8% at < 2, 2 to < 3, and 3 months, respectively).
Mallya Cap Usage
Mean (SD) duration of Mallya cap use was 71.4 (25.4) days and median (range) was 87 (13–91) days. During this period, the mean (SD) number of days that Mallya cap was used to capture insulin dose values was 57.8 (25.2) days (median [range] 62 [13–90] days). The mean (SD) length of gaps between Mallya cap use was 2.4 (6.0) days (median [range] 1.3 [0–54] days) and 4 (4.8%) participants discontinued Mallya cap use during the follow-up period.
At follow-up, the mean (SD) total daily Gla-300 dose recorded using Mallya cap and H2S App was 22.2 (14.7) units and 23.4 (13.4) units in the new and previous Gla-300 user groups, respectively. The mean change in Gla-300 dose from baseline to follow-up was similar between the two groups (mean [SD], 3.3 [16.5] units in new user group and 3.4 [9.2] units in previous user group).
Hypoglycemia
In total, 27.7% of the 83 patients experienced any hypoglycemia during follow-up, with an event rate of 3 per person per year (PPPY; Supplementary Table 2). When a standard time window was used to assess nocturnal hypoglycemia, six program users (7.2%) experienced nocturnal hypoglycemia ≤ 70 mg/dL (≤ 3.9 mmol/L), while one user (1.2%) experienced nocturnal hypoglycemia < 54 mg/dL (3.0 mmol/L), with an event rate of 0.6 PPPY and 0.1 PPPY, respectively. When an expanded window was used to assess nocturnal hypoglycemia, the proportions of patients experiencing nocturnal hypoglycemia ≤ 70 mg/dL (3.9 mmol/L) and < 54 mg/dL (3.0 mmol/L) increased to 15.7% and 4.8%, respectively. The event rates were 1.5 and 0.2 PPPY for ≤ 70 mg/dL (3.9 mmol/L) and < 54 mg/dL (3.0 mmol/L), respectively.
Discussion
This study showed that the use of Gla-300 along with the Mallya cap and H2S app in a small Taiwanese population with T2D was associated with meaningful reductions in mean HbA1c. Mean HbA1c reductions increased numerically with higher baseline HbA1c and with longer duration of Mallya cap usage. HbA1c reductions were largest in new Gla-300 users compared with prior Gla-300 users, though this may be attributed in part to initiating or switching to Gla-300 therapy and to the higher baseline HbA1c values for new Gla-300 users (mean 9.6% [81.0 mmol/mol] versus 7.7% [61.0 mmol/mol] for prior users) and a lower proportion of patients having baseline HbA1c < 7.0% (53.0 mmol/mol) (13% of new users versus 45% of prior users). For new Gla-300 users, at follow-up mean change in HbA1c was − 2.4% (− 26.2 mmol/mol), 41% achieved HbA1c < 7.0% (53.0 mmol/mol), and 66% had a HbA1c reduction > 0.5%. For prior Gla-300 users, mean change in HbA1c was − 0.5% (− 5.5 mmol/mol) and 47% achieved HbA1c < 7.0% (53.0 mmol/mol); 29% had a HbA1c reduction > 0.5%. Overall, total daily Gla-300 dose increased from baseline to follow-up with a mean increment of 3 units observed in both groups. These findings suggest that use of digital healthcare tools within a connected ecosystem such as the Mallya cap and H2S app along with Gla-300 can improve diabetes care-related behaviors and treatment outcomes, even in participants who have already received Gla-300. An HbA1c reduction > 0.5% (5.5 mmol/mol) was achieved by half of all those who used Mallya cap for 3 months.
The mean age of participants in this study was younger than that reported for a 2016 Taiwanese registry study (49.2 versus 62.2 years) [7], but was closer to that reported for a 2021 Taiwanese registry study (54.4 years) [8]. It was notable that approximately 50% of participants in the current study were aged between 20 and 49 years old, suggesting that young-onset diabetes is now an emerging issue in Taiwan. Mean baseline HbA1c values of 9.6% (81.0 mmol/mol) in the new Gla-300 group were similar to values of 10.1% (87.0 mmol/mol) reported in a BI-naïve Taiwanese population in the 2016 study [7] and higher than the 8.4% (68.0 mmol/mol) value reported in the newly diagnosed group from the 2021 study [8]. Following treatment, the improvement in proportion of participants achieving HbA1c < 7.0% (53.0 mmol/mol) in this study from 32.5% to 44.6% was comparable to the improvement in the 2016 study (11.9%) [7], although notably the 2016 study only included participants with suboptimal glycemic control at baseline (HbA1c > 7.0% [53.0 mmol/mol]).
Gla-300 offers a more stable and prolonged pharmacokinetic and pharmacodymamic profile compared with first-generation BI analogues [11], and has been associated with lower rates of hypoglycemia versus the first-generation BI analogue Gla-100 [12, 13]. In this study, less than one-third of participants experienced any hypoglycemia with a mean rate of 3 events PPPY over a 90-day follow-up. By comparison, in the DELIVER program of retrospective cohort studies comparing Gla-300 versus other BIs, the rate of any hypoglycemia ranged from 0.35 to 0.85 PPY with 6 months follow-up [22]. However, it is notable that the mean HbA1c reduction for new Gla-300 users in the current study (2.4%) was greater than that reported in DELIVER, even in the naïve-patient populations with the biggest HbA1c reduction (1.5–1.7%). These results may reflect the convenience of a daily app for self-recording of blood glucose levels and hypoglycemia events, resulting in a higher number of events being captured. Additionally, the impact of using the Mallya cap and H2S app could drive more active BI titration, particularly in new Gla-300 users, which may translate to a higher rate of hypoglycemia, as has been reported previously with patient-led active titration [23].
Digital systems such as the H2S app and platform can help healthcare providers to supervise more patients by allowing remote monitoring of insulin treatment. Therefore, studies such as this are important to analyze the contribution of H2S and Mallya cap to diabetes management, in particular with initiating and titrating BI. In one real-world study, moderate- or high-frequency use of the H2S app was associated with greater improvements in HbA1c values compared with those who used the app less often [20]. Strengths of this study include the automatic recording of insulin dose, which enables accurate measurement and timing of doses. This provided detailed information on adherence, removing the need for assumptions that can lead to bias in real-world studies where adherence data is typically derived from claims databases and electronic medical records. The convenience of the digital ecosystem enables patients to record events such as hypoglycemic episodes soon after they occur, minimizing the recall bias associated with reporting events only at appointments. A number of potential study limitations should be highlighted. Firstly, there was no control group in this study to assess the effectiveness of the program versus standard care or Gla-300 alone without Mallya Cap, and the small sample size may not allow robust statistical inference, particularly for some subgroup analyses. Also, as only 16% of the overall study population were aged ≥ 65 years, further studies with a larger proportion of older patients may be useful to further understand the benefit of the digital ecosystem to patients of all ages. As a result of the nature of H2S data, behaviors such as exercise that could have impacted glycemic control could not be analyzed. Additionally, medication use and diagnosis information prior to H2S app registration were not available, potentially introducing bias to the definition of new users, and to the reporting of results such as diabetes duration and comorbidities. Identifying diabetes and comorbidities relied on use of the ICD-10 diagnosis field, leading to the potential for coding inaccuracies. Furthermore, patient comorbidity burden may also have been underestimated for patients without electronic medical records. Environmental factors in the laboratory may have affected HbA1c measurement, and erroneous self-reported information (e.g., manual entry of self-monitored blood glucose) is a possibility. Finally, prescription drug data were used to indicate prescribed medications, but the data do not confirm whether medication other than Gla-300 was used by the patient.
Conclusion
Overall, our study results suggest that the Gla-300 + Cap + App program could help to improve the glycemic condition of patients with T2D and may aid both new and previous insulin users in conquering clinical inertia. The single-arm, real-world study design had inherent limitations; nevertheless, use of the Mallya cap + H2S app program resulted in reductions of HbA1c and high goal attainment for both new and previous Gla-300 users. Further prospective studies and randomized controlled trials are needed to confirm these findings.
Data Availability
The datasets containing participant-level data generated during and/or analyzed during the current study are available on reasonable request from qualified researchers. Participant-level data will be anonymized, and study documents will be redacted to protect the privacy of study participants. Further details on Sanofi’s data sharing criteria, eligible studies, and process for requesting access can be found at https://www.vivli.org/.
References
IDF Diabetes Atlas 10th Edition. Brussels: International Diabetes Federation; 2021.
Kerr D, Edelman S, Vespasiani G, Khunti K. New digital health technologies for insulin initiation and optimization for people with type 2 diabetes. Endocr Pract. 2022;28:811–21.
Ma RC, Chan JC. Type 2 diabetes in East Asians: similarities and differences with populations in Europe and the United States. Ann N Y Acad Sci. 2013;1281:64–91.
Rhee EJ. Diabetes in Asians. Endocrinol Metab (Seoul). 2015;30:263–9.
Lin CC, Li CI, Hsiao CY, et al. Time trend analysis of the prevalence and incidence of diagnosed type 2 diabetes among adults in Taiwan from 2000 to 2007: a population-based study. BMC Public Health. 2013;13:318.
Hsu C-C, Tu S-T, Sheu WH-H. Diabetes Atlas: achievements and challenges in diabetes care in Taiwan. J Formos Med Assoc. 2019;2019(118):S130–4.
Chien MN, Chen YL, Hung YJ, et al. Glycemic control and adherence to basal insulin therapy in Taiwanese patients with type 2 diabetes mellitus. J Diabetes Investig. 2016;7:881–8.
Wang J-S, Lo S-H, Yeh Y-P, et al. Distinct associations of self-monitoring of blood glucose with glycemic control and hypoglycemia between groups of recently diagnosed and long-term follow-up type 2 diabetes: the Taiwan Diabetes Registry. Int J Clin Pract. 2021;75:e14410.
Tien KJ, Hung YJ, Chen JF, et al. Basal insulin therapy: unmet medical needs in Asia and the new insulin glargine in diabetes treatment. J Diabetes Investig. 2019;10:560–70.
Chun J, Strong J, Urquhart S. Insulin initiation and titration in patients with type 2 diabetes. Diabetes Spectr. 2019;32:104–11.
Becker RH, Nowotny I, Teichert L, Bergmann K, Kapitza C. Low within- and between-day variability in exposure to new insulin glargine 300 U/ml. Diabetes Obes Metab. 2015;17:261–7.
Ji L, Kang ES, Dong X, et al. Efficacy and safety of insulin glargine 300 U/mL versus insulin glargine 100 U/mL in Asia Pacific insulin-naive people with type 2 diabetes: the EDITION AP randomized controlled trial. Diabetes Obes Metab. 2020;22:612–21.
Terauchi Y, Koyama M, Cheng X, et al. New insulin glargine 300 U/ml versus glargine 100 U/ml in Japanese people with type 2 diabetes using basal insulin and oral antihyperglycaemic drugs: glucose control and hypoglycaemia in a randomized controlled trial (EDITION JP 2). Diabetes Obes Metab. 2016;18:366–74.
Galstyan GR, Tirosh A, Vargas-Uricoechea H, et al. Real-world effectiveness and safety of insulin glargine 300 U/mL in insulin-naive people with type 2 diabetes: the ATOS study. Diabetes Ther. 2022;13:1187–202.
Yen FS, Hwu CM. Challenges of optimizing insulin therapy for patients with type 2 diabetes mellitus. J Diabetes Investig. 2021;12:1523–5.
Polonsky WH, Arsenault J, Fisher L, et al. Initiating insulin: how to help people with type 2 diabetes start and continue insulin successfully. Int J Clin Pract. 2017;71:e12973.
Health2Sync. Comprehensive Chronic Disease Management. Turn data into informative analysis and manage chronic diseases efficiently. 2023. https://www.health2sync.com. Accessed Mar 9, 2024.
Bramwell SE, Meyerowitz-Katz G, Ferguson C, et al. The effect of an mHealth intervention for titration of insulin for type 2 diabetes: a pilot study. Eur J Cardiovasc Nurs. 2020;19:386–92.
Mallya. Mallya turns your insulin pen into a smart device! 2023. https://my-mallya.com/en/. Accessed Mar 9, 2024.
Tu YZ, Chang YT, Chiou HY, Lai K. The effects of continuous usage of a diabetes management app on glycemic control in real-world clinical practice: retrospective analysis. J Med Internet Res. 2021;23:e23227.
Chang YT, Tu YZ, Chiou HY, Lai K, Yu NC. Real-world benefits of diabetes management app use and self-monitoring of blood glucose on glycemic control: retrospective analyses. JMIR Mhealth Uhealth. 2022;10:e31764.
Blonde L, Bailey T, Sullivan SD, Freemantle N. Insulin glargine 300 units/mL for the treatment of individuals with type 2 diabetes in the real world: a review of the DELIVER programme. Diabetes Obes Metab. 2021;23:1713–21.
Castellana M, Procino F, Sardone R, Trimboli P, Giannelli G. Efficacy and safety of patient-led versus physician-led titration of basal insulin in patients with uncontrolled type 2 diabetes: a meta-analysis of randomized controlled trials. BMJ Open Diabetes Res Care. 2020;8:e001477.
Acknowledgements
The authors thank the patients and study investigators for their contributions and Pierre Evenou, PhD (Sanofi) for coordinating the development, facilitating author discussions, and providing a courtesy review of this manuscript.
Medical Writing and Editorial Assistance
Editorial support and medical writing assistance was provided by Louise Gildea, PhD and Arthur Holland, PhD at Fishawack Communications Ltd, part of Avalere Health, and was funded by Sanofi.
Funding
This study and the Journal Rapid Service Fee for this publication was sponsored by Sanofi.
Author information
Authors and Affiliations
Contributions
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article and are guarantors of this work. As such, all authors had full access to all the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis. Fang Liz Zhou, Nancy Cui, Aakash Gandhi, and Tsung-Ying Lee participated in conception and design of the study and Jung-Fu Chen and Chih-Yuan Wang participated in data acquisition. Chih-Yuan Wang, Fang Liz Zhou, Aakash Gandhi, Tsung-Ying Lee, Nancy Cui, Jiuo-Shan Mao and Jung-Fu Chen participated in data analysis and interpretation, and the writing, reviewing, and editing of the manuscript, with final responsibility for approving the published version.
Corresponding author
Ethics declarations
Conflict of Interest
Chih-Yuan Wang: Nothing to disclose. Fang Liz Zhou, Aakash Gandhi, Nancy Cui and Jiuo-Shan Mao: Employees of Sanofi; may hold shares and/or stock options in the company. Tsung-Ying Lee: Intern of Sanofi at time of study. Jung-Fu Chen: Nothing to disclose.
Ethical Approval
This study was conducted in accordance with the guidelines for Good Epidemiology Practice and the Declaration of Helsinki. The study was approved by the local Institutional Review Board review of the National Taiwan University Hospital (202211018RSC) and Kaohsiung Chang Gung Hospital (202201756B0A3). The study used de-identified data from H2S retrospectively and patients were not recruited specifically for this study. All patients who registered to use the H2S app provided consent for their data to be analyzed for research purposes. Permission was obtained from the owners of H2S to conduct this research using data from the platform.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wang, CY., Zhou, F.L., Gandhi, A.B. et al. Real-World Effectiveness of the Gla-300 + Cap + App Program in Adult Users Living with Type 2 Diabetes in Taiwan. Diabetes Ther 15, 1389–1401 (2024). https://doi.org/10.1007/s13300-024-01570-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01570-1