Abstract
Purpose
Rheumatic heart disease is a major cause of mitral valve (MV) dysfunction, particularly in disadvantaged areas and developing countries. There lacks a critical understanding of the disease biomechanics, and as such, the purpose of this study was to generate the first ex vivo porcine model of rheumatic MV disease by simulating the human pathophysiology and hemodynamics.
Methods
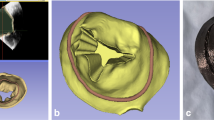
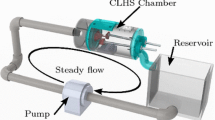
Healthy porcine valves were altered with heat treatment, commissural suturing, and cyanoacrylate tissue coating, all of which approximate the pathology of leaflet stiffening and thickening as well as commissural fusion. Hemodynamic data, echocardiography, and high-speed videography were collected in a paired manner for control and model valves (n = 4) in an ex vivo left heart simulator. Valve leaflets were characterized in an Instron tensile testing machine to understand the mechanical changes of the model (n = 18).
Results
The model showed significant differences indicative of rheumatic disease: increased regurgitant fractions (p < 0.001), reduced effective orifice areas (p < 0.001), augmented transmitral mean gradients (p < 0.001), and increased leaflet stiffness (p = 0.025).
Conclusion
This work represents the creation of the first ex vivo model of rheumatic MV disease, bearing close similarity to the human pathophysiology and hemodynamics, and it will be used to extensively study both established and new treatment techniques, benefitting the millions of affected victims.







Similar content being viewed by others
Data Availability
All data is made available in this manuscript.
Code Availability
Not required.
Abbreviations
- RHD:
-
Rheumatic heart disease
- MV:
-
Mitral valve
- 3D:
-
Three-dimensional
References
Agozzino, L., A. Falco, F. de Vivo, C. de Vincentiis, L. de Luca, S. Esposito, et al. Surgical pathology of the mitral valve: gross and histological study of 1288 surgically excised valves. Int. J. Cardiol. 37:79–89, 1992. https://doi.org/10.1016/0167-5273(92)90135-p.
Al-Atassi, T., H. D. Toeg, R. Jafar, B. Sohmer, M. Labrosse, and M. Boodhwani. Impact of aortic annular geometry on aortic valve insufficiency: insights from a preclinical, ex vivo, porcine model. J. Thorac. Cardiovasc. Surg. 150:656–664, 2015. https://doi.org/10.1016/j.jtcvs.2015.06.060.
Antunes, M. J. Repair of the rheumatic mitral valve: is the controversy over? Asian Cardiovasc. Thorac. Ann. 28:374–376, 2020. https://doi.org/10.1177/0218492320927316.
Banerjee, T., S. Mukherjee, S. Ghosh, M. Biswas, S. Dutta, S. Pattari, et al. Clinical significance of markers of collagen metabolism in rheumatic mitral valve disease. PLoS ONE. 9:e90527, 2014. https://doi.org/10.1371/journal.pone.0090527.
Barber, J. E., F. K. Kasper, N. B. Ratliff, D. M. Cosgrove, B. P. Griffin, and I. Vesely. Mechanical properties of myxomatous mitral valves. J. Thorac. Cardiovasc. Surg. 122:955–962, 2001. https://doi.org/10.1067/mtc.2001.117621.
Bennett, J., J. Zhang, W. Leung, S. Jack, J. Oliver, R. Webb, et al. Rising ethnic inequalities in acute rheumatic fever and rheumatic heart disease, New Zealand, 2000–2018. Emerg. Infect. Dis. 27:191791, 2021. https://doi.org/10.3201/eid2701.191791.
Carapetis, J. R., A. C. Steer, E. K. Mulholland, and M. Weber. The global burden of group A streptococcal diseases. Lancet Infect. Dis. 5:685–694, 2005. https://doi.org/10.1016/S1473-3099(05)70267-X.
Chauvaud, S., J. F. Fuzellier, A. Berrebi, A. Deloche, J. N. Fabiani, and A. Carpentier. Long-term (29 years) results of reconstructive surgery in rheumatic mitral valve insufficiency. Circulation. 104:I12–I15, 2001. https://doi.org/10.1161/hc37t1.094707.
Cheunsuchon, P., T. Chuangsuwanich, N. Samanthai, M. Warnnissorn, P. Leksrisakul, and P. Thongcharoen. Surgical pathology and etiology of 278 surgically removed mitral valves with pure regurgitation in Thailand. Cardiovasc. Pathol. 16:104–110, 2007. https://doi.org/10.1016/j.carpath.2006.08.005.
Coffey, S., R. Roberts-Thomson, A. Brown, J. Carapetis, M. Chen, M. Enriquez-Sarano, et al. Global epidemiology of valvular heart disease. Nat. Rev. Cardiol. 2021. https://doi.org/10.1038/s41569-021-00570-z.
Essop, M. R., and V. T. Nkomo. Rheumatic and nonrheumatic valvular heart disease: epidemiology, management, and prevention in Africa. Circulation. 112:3584–3591, 2005. https://doi.org/10.1161/CIRCULATIONAHA.105.539775.
Folger, G. M., R. Hajar, A. Robida, and H. A. Hajar. Occurrence of valvar heart disease in acute rheumatic fever without evident carditis: colour-flow Doppler identification. Br. Heart J. 67:434–438, 1992. https://doi.org/10.1136/hrt.67.6.434.
Fu, G., Z. Zhou, S. Huang, G. Chen, M. Liang, L. Huang, et al. Mitral valve surgery in patients with rheumatic heart disease: repair vs. replacement. Front. Cardiovasc. Med. 8:685746, 2021. https://doi.org/10.3389/fcvm.2021.685746.
GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 392:1789–1858, 2018. https://doi.org/10.1016/S0140-6736(18)32279-7.
Imbrie-Moore, A. M., M. H. Park, M. J. Paulsen, M. Sellke, R. Kulkami, H. Wang, et al. Biomimetic six-axis robots replicate human cardiac papillary muscle motion: pioneering the next generation of biomechanical heart simulator technology. J. R. Soc. Interface. 17:20200614, 2020. https://doi.org/10.1098/rsif.2020.0614.
Imbrie-Moore, A. M., C. C. Paullin, M. J. Paulsen, F. Grady, H. Wang, C. E. Hironaka, et al. A novel 3D-Printed preferential posterior mitral annular dilation device delineates regurgitation onset threshold in an ex vivo heart simulator. Med. Eng. Phys. 77:10–18, 2020. https://doi.org/10.1016/j.medengphy.2020.01.005.
Imbrie-Moore, A. M., M. J. Paulsen, A. D. Thakore, H. Wang, C. E. Hironaka, H. J. Lucian, et al. Ex vivo biomechanical study of apical versus papillary neochord anchoring for mitral regurgitation. Ann. Thorac. Surg. 108:90–97, 2019. https://doi.org/10.1016/j.athoracsur.2019.01.053.
Imbrie-Moore, A. M., M. J. Paulsen, Y. Zhu, H. Wang, H. J. Lucian, J. M. Farry, et al. A novel cross-species model of Barlow’s disease to biomechanically analyze repair techniques in an ex vivo left heart simulator. J. Thorac. Cardiovasc. Surg. 161:1776–1783, 2021. https://doi.org/10.1016/j.jtcvs.2020.01.086.
International Standard. ISO 5840–1:2015 (E): Cardiovascular Implants: Cardiac Valve Prostheses. Geneva: ISO Copyright Office, 2015.
Jaine, R., M. Baker, and K. Venugopal. Acute rheumatic fever associated with household crowding in a developed country. Pediatr. Infect. Dis J. 30:315–319, 2011. https://doi.org/10.1097/INF.0b013e3181fbd85b.
Jiao, Y., T. Luo, H. Zhang, J. Han, Y. Li, Y. Jia, et al. Repair versus replacement of mitral valves in cases of severe rheumatic mitral stenosis: mid-term clinical outcomes. J. Thorac. Dis. 11:3951–3961, 2019. https://doi.org/10.21037/jtd.2019.08.101.
Kabukçu, M., E. Arslantas, I. Ates, F. Demircioglu, and F. Ersel. Clinical, echocardiographic, and hemodynamic characteristics of rheumatic mitral valve stenosis and atrial fibrillation. Angiology. 56:159–163, 2005. https://doi.org/10.1177/000331970505600206.
Kheradvar, A., E. M. Groves, C. A. Simmons, B. Griffith, S. H. Alavi, R. Tranquillo, et al. Emerging trends in heart valve engineering: Part III. Novel technologies for mitral valve repair and replacement. Ann. Biomed. Eng. 43:858–870, 2015. https://doi.org/10.1007/s10439-014-1129-y.
Kumar, R. K., M. J. Antunes, A. Beaton, M. Mirabel, V. T. Nkomo, E. Okello, et al. Contemporary diagnosis and management of rheumatic heart disease: implications for closing the gap: a scientific statement from the american heart association. Circulation. 142:e337–e357, 2020. https://doi.org/10.1161/CIR.0000000000000921.
Kunzelman, K. S., and R. P. Cochran. Stress/strain characteristics of porcine mitral valve tissue: parallel versus perpendicular collagen orientation. J. Card. Surg. 7:71–78, 1992. https://doi.org/10.1111/j.1540-8191.1992.tb00777.x.
Lally, C., A. J. Reid, and P. J. Prendergast. Elastic behavior of porcine coronary artery tissue under uniaxial and equibiaxial tension. Ann. Biomed. Eng. 32:1355–1364, 2004. https://doi.org/10.1114/b:abme.0000042224.23927.ce.
Laudari, S., and G. Subramanyam. A study of spectrum of rheumatic heart disease in a tertiary care hospital in Central Nepal. Int. J. Cardiol. Heart Vasc. 15:26–30, 2017. https://doi.org/10.1016/j.ijcha.2017.03.007.
Lim, K. O., and D. R. Boughner. Mechanical properties of human mitral valve chordae tendineae: variation with size and strain rate. Can. J. Physiol. Pharmacol. 53:330–339, 1975. https://doi.org/10.1139/y75-048.
Lis, Y., M. C. Burleigh, D. J. Parker, A. H. Child, J. Hogg, and M. J. Davies. Biochemical characterization of individual normal, floppy and rheumatic human mitral valves. Biochem. J. 244:597–603, 1987. https://doi.org/10.1042/bj2440597.
Liu, M., L. Lu, R. Sun, Y. Zheng, and P. Zhang. Rheumatic heart disease: causes, symptoms, and treatments. Cell Biochem. Biophys. 72:861–863, 2015. https://doi.org/10.1007/s12013-015-0552-5.
Lorusso, R., M. De Bonis, G. De Cicco, F. Maisano, C. Fucci, and O. Alfieri. Mitral insufficiency and its different aetiologies: old and new insights for appropriate surgical indications and treatment. J. Cardiovasc. Med. 8:108–113, 2007. https://doi.org/10.2459/01.JCM.0000260211.02468.0a.
Marijon, E., P. Ou, D. S. Celermajer, B. Ferreira, A. O. Mocumbi, D. Jani, et al. Prevalence of rheumatic heart disease detected by echocardiographic screening. N. Engl. J. Med. 357:470–476, 2007. https://doi.org/10.1056/NEJMoa065085.
Park, M. H., Y. Zhu, A. M. Imbrie-Moore, H. Wang, M. Marin-Cuartas, M. J. Paulsen, et al. Heart valve biomechanics: the frontiers of modeling modalities and the expansive capabilities of ex vivo heart simulation. Front. Cardiovasc. Med. 8:673689, 2021. https://doi.org/10.3389/fcvm.2021.673689.
Passos, L. S. A., M. C. P. Nunes, and E. Aikawa. Rheumatic heart valve disease pathophysiology and underlying mechanisms. Front. Cardiovasc. Med. 7:612716, 2020. https://doi.org/10.3389/fcvm.2020.612716.
Paulsen, M. J., A. M. Imbrie-Moore, H. Wang, J. H. Bae, C. E. Hironaka, J. M. Farry, et al. Mitral chordae tendineae force profile characterization using a posterior ventricular anchoring neochordal repair model for mitral regurgitation in a three-dimensional-printed ex vivo left heart simulator. Eur. J. Cardiothorac. Surg. 57:535–544, 2020. https://doi.org/10.1093/ejcts/ezz258.
De Santo, L. S., G. Romano, A. Della Corte, F. Tizzano, A. Petraio, C. Amarelli, et al. Mitral mechanical replacement in young rheumatic women: analysis of long-term survival, valve-related complications, and pregnancy outcomes over a 3707-patient-year follow-up. J. Thorac. Cardiovasc. Surg. 130:13–19, 2005. https://doi.org/10.1016/j.jtcvs.2004.11.032.
Seckeler, M. D., and T. R. Hoke. The worldwide epidemiology of acute rheumatic fever and rheumatic heart disease. Clin. Epidemiol. 3:67–84, 2011. https://doi.org/10.2147/CLEP.S12977.
Siefert, A. W., J.-P.M. Rabbah, E. L. Pierce, K. S. Kunzelman, and A. P. Yoganathan. Quantitative evaluation of annuloplasty on mitral valve chordae tendineae forces to supplement surgical planning model development. Cardiovasc. Eng. Technol. 5:35–43, 2014. https://doi.org/10.1007/s13239-014-0175-9.
Sliwa, K., M. Carrington, B. M. Mayosi, E. Zigiriadis, R. Mvungi, and S. Stewart. Incidence and characteristics of newly diagnosed rheumatic heart disease in urban African adults: insights from the heart of Soweto study. Eur. Heart J. 31:719–727, 2010. https://doi.org/10.1093/eurheartj/ehp530.
Uricchio, J. F., L. Bentivoglio, J. Dickens, and H. Goldberg. The value of left heart catheterization in patients with rheumatic mitral valve disease. Dis. Chest. 34:525–536, 1958. https://doi.org/10.1378/chest.34.5.525.
Vasan, R. S., S. Shrivastava, M. Vijayakumar, R. Narang, B. C. Lister, and J. Narula. Echocardiographic evaluation of patients with acute rheumatic fever and rheumatic carditis. Circulation. 94:73–82, 1996. https://doi.org/10.1161/01.cir.94.1.73.
Veasy, L. G., L. Y. Tani, and H. R. Hill. Persistence of acute rheumatic fever in the intermountain area of the United States. J. Pediatr. 124:9–16, 1994. https://doi.org/10.1016/s0022-3476(94)70247-0.
Watkins, D. A., A. Z. Beaton, J. R. Carapetis, G. Karthikeyan, B. M. Mayosi, R. Wyber, et al. Rheumatic heart disease worldwide: JACC scientific expert panel. J. Am. Coll. Cardiol. 72:1397–1416, 2018. https://doi.org/10.1016/j.jacc.2018.06.063.
Watkins, D. A., C. O. Johnson, S. M. Colquhoun, G. Karthikeyan, A. Beaton, G. Bukhman, et al. Global, regional, and national burden of rheumatic heart disease, 1990–2015. N. Engl. J. Med. 377:713–722, 2017. https://doi.org/10.1056/NEJMoa1603693.
Zakkar, M., E. Amirak, K. M. J. Chan, and P. P. Punjabi. Rheumatic mitral valve disease: current surgical status. Prog. Cardiovasc. Dis. 51:478–481, 2009. https://doi.org/10.1016/j.pcad.2008.08.008.
Zhu, Y., A. M. Imbrie-Moore, M. J. Paulsen, B. Priromprintr, M. H. Park, H. Wang, et al. A novel aortic regurgitation model from cusp prolapse with hemodynamic validation using an ex vivo left heart simulator. J. Cardiovasc. Transl. Res. 2020. https://doi.org/10.1007/s12265-020-10038-z.
Zhu, Y., A. M. Imbrie-Moore, M. J. Paulsen, B. Priromprintr, H. Wang, H. J. Lucian, et al. Novel bicuspid aortic valve model with aortic regurgitation for hemodynamic status analysis using an ex vivo simulator. J. Thorac. Cardiovasc. Surg. 2020. https://doi.org/10.1016/j.jtcvs.2020.06.028.
Zühlke, L. J., and A. C. Steer. Estimates of the global burden of rheumatic heart disease. Glob. Heart. 8:189–195, 2013. https://doi.org/10.1016/j.gheart.2013.08.008.
Acknowledgments
This work was supported by the National Institutes of Health (NIH R01 HL152155-03, YJW), the National Science Foundation Graduate Research Fellowship Program (DGE-1656518, AMI), the Stanford Graduate Fellowship (AMI), and the Thoracic Surgery Foundation Resident Research Fellowship (YZ). We would also like to thank the generous donation by Donald and Sally O’Neal to support this research effort.
Funding
This work was supported by the National Institutes of Health (NIH R01 HL152155-03 YJW), the National Science Foundation Graduate Research Fellowship Program (DGE-1656518, AMI), the Stanford Graduate Fellowship (AMI), and the Thoracic Surgery Foundation Resident Research Fellowship (YZ).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflicts of interest.
Ethical Approval
Not required.
Consent to Participate
Not required.
Consent for Publication
All authors consent to publication of this manuscript.
Additional information
Associate Editor Pedro del Nido oversaw the review of this article.
Associate Editor Pedro del Nido, M.D. oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (MP4 36706 kb)
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Park, M.H., Pandya, P.K., Zhu, Y. et al. A Novel Rheumatic Mitral Valve Disease Model with Ex Vivo Hemodynamic and Biomechanical Validation. Cardiovasc Eng Tech 14, 129–140 (2023). https://doi.org/10.1007/s13239-022-00641-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-022-00641-3