Abstract
Purpose
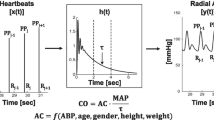
Through pulse contour analysis (PCA) devices would enable to obtain non-invasive operator-independent cardiac output (CO) measurements [CO(PCA)]. The agreement between CO(PCA) and data from two-dimensional [CO(2D)] or Doppler [CO(VTI)] echocardiography (references) remains controversial.
Aims
To analyze: (1) CO(PCA), CO(2D) and CO(VTI) agreement, (2) determinants of methods’ differences in measured CO values.
Methods
Simultaneous echocardiography and PCA records (Mobil-O-Graph/Germany) were obtained in 130 subjects (age: 29 ± 17 years). Hemodynamic (e.g., heart rate [HR]), arterial (e.g., arterial stiffness, augmentation index [AIx]) and cardiac structural–functional (e.g., left ventricle end-diastolic diameters [LVEDD]) parameters were obtained. Data from the entire group (all; 10–85 years), children (≤ 16 years), adolescents (17–24 years) and adults (> 24 years) were separately analyzed.
Results
The highest Lin’s concordance correlation coefficient (CCC) were obtained when analyzing CO(PCA)/CO(2D) association (0.672, 0.785, 0.721, 0.487 for all, children, adolescents and adults, respectively); CCC levels were higher at younger ages. Bland–Altman’s systematic errors between CO(PCA)/CO(2D) were 0.12, 0.17, 0.07 and 0.14 L/min, for all, children, adolescents and adults, respectively (non-significant). CO(VTI)/CO(PCA) systematic error only reached significance in adults (0.34 L/min, p = 0.002). Bland–Altman’s proportional errors were not statistically significant when CO(PCA)/CO(2D) differences were analysed in children and adolescents. Higher AIx and LVEDD levels associated greater CO(2D)/CO(PCA) differences; higher AIx and HR levels were associated to differences between CO(VTI) and CO(PCA).
Conclusion
CO(PCA) had systematic (< 0.17 L/min) and percent (≤ 30%) errors, which allow us to postulate that its use allows reaching levels comparable to those of echocardiography. Differences in CO-data between methods were associated with arterial and cardiac properties.



Similar content being viewed by others
References
Abu-Arafeh, A., H. Jordan, and G. Drummond. Reporting of method comparison studies: a review of advice, an assessment of current practice, and specific suggestions for future reports. Br. J. Anaesth. 117(5):569–575, 2016.
Bergamaschi, V., G. L. Vignazia, A. Messina, D. Colombo, G. Cammarota, F. D. Corte, E. Traversi, and P. Navalesi. Transthoracic echocardiographic assessment of cardiac output in mechanically ventilated critically ill patients by intensive care unit physicians. Rev. Bras. Anestesiol. 69(1):20–26, 2019.
Bland, J. M., and D. G. Altman. Measuring agreement in method comparison studies. Stat. Methods Med. Res. 8:135–160, 1999.
Broch, O., B. Bein, M. Gruenewald, S. Masing, K. Huenges, A. Haneya, M. Steinfath, and J. Renner. Accuracy of cardiac output by nine different pulse contour algorithms in cardiac surgery patients: a comparison with transpulmonary thermodilution. Biomed. Res. Int. 2016:3468015, 2016.
Camporota, L., and R. Beale. Pitfalls in haemodynamic monitoring based on the arterial pressure waveform. Crit. Care 14(2):124, 2010.
Cecconi, M., A. Rhodes, J. Poloniecki, G. Della Rocca, and R. M. Grounds. Bench-to-bedside review: the importance of the precision of the reference technique in method comparison studies—with specific reference to the measurement of cardiac output. Crit. Care 13(1):201, 2009.
Critchley, L. A., and J. A. Critchley. A meta-analysis of studies using bias and precision statistics to compare cardiac output measurement techniques. J. Clin. Monit. Comput. 15(2):85–91, 1999.
Curcio, S., V. García-Espinosa, M. Arana, I. Farro, P. Chiesa, G. Giachetto, Y. Zócalo, and D. Bia. Growing-related changes in arterial properties of healthy children, adolescents, and young adults nonexposed to cardiovascular risk factors: analysis of gender-related differences. Int. J. Hypertens. 2016:4982676, 2016.
de Wilde, R. B., J. J. Schreuder, P. C. van den Berg, and J. R. Jansen. An evaluation of cardiac output by five arterial pulse contour techniques during cardiac surgery. Anaesthesia 62(8):760–768, 2007.
Díaz, A., Y. Zócalo, and D. Bia. Reference intervals and percentile curves of echocardiographic left ventricular mass, relative wall thickness and ejection fraction in healthy children and adolescents. Pediatr. Cardiol. 40(2):283–301, 2019.
Díaz, A., Y. Zócalo, D. Bia, F. Sabino, V. Rodríguez, and E. I. Cabrera Fischer. Reference intervals of aortic pulse wave velocity assessed with an oscillometric device in healthy children and adolescents from Argentina. Clin. Exp. Hypertens. 41(2):101–112, 2019.
Díaz, A., Y. Zócalo, D. Bia, S. Wray, and E. C. Fischer. Reference intervals and percentiles for carotid-femoral pulse wave velocity in a healthy population aged between 9 and 87 years. J. Clin. Hypertens. (Greenwich) 20(4):659–671, 2018.
Díaz, A., Y. Zócalo, E. Cabrera-Fischer, and D. Bia. Reference intervals and percentile curve for left ventricular outflow tract (LVOT), velocity time integral (VTI), and LVOT-VTI-derived hemodynamic parameters in healthy children and adolescents: Analysis of echocardiographic methods association and agreement. Echocardiography 35(12):2014–2034, 2018.
García, X., L. Mateu, J. Maynar, J. Mercadal, A. Ochagavía, and A. Ferrandiz. Estimating cardiac output. Utility in the clinical practice. Available invasive and non-invasive monitoring. Med. Intensiva 35(9):552–561, 2011.
Gottdiener, J. S., J. Bednarz, R. Devereux, J. Gardin, A. Klein, W. J. Manning, A. Morehead, D. Kitzman, J. Oh, M. Quinones, N. B. Schiller, J. H. Stein, and N. J. Weissman. American Society of Echocardiography. American Society of Echocardiography recommendations for use of echocardiography in clinical trials. J. Am. Soc. Echocardiogr. 17(10):1086–1190, 2004.
Grensemann, J. Cardiac output monitoring by pulse contour analysis, the technical basics of less-invasive techniques. Front. Med. (Lausanne) 5:64, 2018.
Joosten, A., O. Desebbe, K. Suehiro, L. S. Murphy, M. Essiet, B. Alexander, M. O. Fischer, L. Barvais, L. Van Obbergh, D. Maucort-Boulch, and M. Cannesson. Accuracy and precision of non-invasive cardiac output monitoring devices in perioperative medicine: a systematic review and meta-analysis†. Br. J. Anaesth. 118(3):298–310, 2017.
Lang, R. M., L. P. Badano, V. Mor-Avi, J. Afilalo, A. Armstrong, L. Ernande, F. A. Flachskampf, E. Foster, S. A. Goldstein, T. Kuznetsova, P. Lancellotti, D. Muraru, M. H. Picard, E. R. Rietzschel, L. Rudski, K. T. Spencer, W. Tsang, and J. U. Voigt. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 16(3):233–270, 2015.
Majonga, E. D., A. M. Rehman, G. McHugh, H. A. Mujuru, K. Nathoo, M. S. Patel, S. Munyati, J. O. Odland, K. Kranzer, J. P. Kaski, and R. A. Ferrand. Echocardiographic reference ranges in older children and adolescents in sub-Saharan Africa. Int. J. Cardiol. 248:409–413, 2017.
Monnet, X., and J. L. Teboul. Passive leg raising: five rules, not a drop of fluid!. Crit. Care 19:18, 2015.
Odor, P. M., S. Bampoe, and M. Cecconi. Cardiac output monitoring: validation studies-how results should be presented. Curr. Anesthesiol. Rep. 7(4):410–415, 2017.
Papaioannou, T. G., D. Soulis, O. Vardoulis, A. Protogerou, P. P. Sfikakis, N. Stergiopulos, and C. Stefanadis. First in vivo application and evaluation of a novel method for non-invasive estimation of cardiac output. Med. Eng. Phys. 36(10):1352–1357, 2014.
Peyton, P. J., and S. W. Chong. Minimally invasive measurement of cardiac output during surgery and critical care: a meta-analysis of accuracy and precision. Anesthesiology 113(5):1220–1235, 2010.
Pickett, J. D., E. Bridges, P. A. Kritek, and J. D. Whitney. Passive leg-raising and prediction of fluid responsiveness: systematic review. Crit. Care Nurse. 37(2):32–47, 2017.
Porter, T. R., S. K. Shillcutt, M. S. Adams, G. Desjardins, K. E. Glas, J. J. Olson, and R. W. Troughton. Guidelines for the use of echocardiography as a monitor for therapeutic intervention in adults: a report from the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 28(1):40–56, 2015.
Schlöglhofer, T., H. Gilly, and H. Schima. Semi-invasive measurement of cardiac output based on pulse contour: a review and analysis. Can. J. Anaesth. 61(5):452–479, 2014.
Suehiro, K., A. Joosten, L. S. Murphy, O. Desebbe, B. Alexander, S. H. Kim, and M. Cannesson. Accuracy and precision of minimally-invasive cardiac output monitoring in children: a systematic review and meta-analysis. J. Clin. Monit. Comput. 30(5):603–620, 2016.
Townsend, R. R., H. R. Black, J. A. Chirinos, P. U. Feig, K. C. Ferdinand, M. Germain, C. Rosendorff, S. P. Steigerwalt, and J. A. Stepanek. Clinical use of pulse wave analysis: proceedings from a symposium sponsored by North American Artery. J. Clin. Hypertens. (Greenwich) 17(7):503–513, 2015.
Villavicencio, C., J. Leache, J. Marin, I. Oliva, A. Rodriguez, M. Bodí, and N. J. Soni. Basic critical care echocardiography training of intensivists allows reproducible and reliable measurements of cardiac output. Ultrasound. J. 11(1):5, 2019.
Wassertheurer, S., J. Kropf, T. Weber, M. van der Giet, J. Baulmann, M. Ammer, B. Hametner, C. C. Mayer, B. Eber, and D. Magometschnigg. A new oscillometric method for pulse wave analysis: comparison with a common tonometric method. J. Hum. Hypertens. 24(8):498–504, 2010.
Weber, T., S. Wassertheurer, M. Rammer, E. Maurer, B. Hametner, C. C. Mayer, J. Kropf, and B. Eber. Validation of a brachial cuff-based method for estimating central systolic blood pressure. Hypertension 58(5):825–832, 2011.
Weiss, W., C. Gohlisch, C. Harsch-Gladisch, M. Tölle, W. Zidek, and M. van der Giet. Oscillometric estimation of central blood pressure: validation of the Mobil-O-Graph in comparison with the SphygmoCor device. Blood Press. Monit. 17(3):128–131, 2012.
Wetterslev, M., H. Møller-Sørensen, R. R. Johansen, and A. Perner. Systematic review of cardiac output measurements by echocardiography vs. thermodilution: the techniques are not interchangeable. Intensive Care Med. 42(8):1223–1233, 2016.
World Health Organization. Child and adolescent health and development. In: http://www.searo.who.int/entity/child_adolescent/topics/adolescent_health/en/). Accessed 30 August 2019.
Zocalo, Y., J. M. Castro, V. Garcia-Espinosa, S. Curcio, P. Chiesa, G. Giachetto, E. I. Cabrera-Fischer, and D. Bia. Forward and backward aortic components and reflection indexes in children and adolescents: determinants and role in high pressure states. Curr. Hypertens. Rev. 14(2):137–153, 2018.
Zócalo, Y., S. Curcio, V. García-Espinosa, P. Chiesa, G. Giachetto, and D. Bia. Comparative analysis of arterial parameters variations associated with inter-individual variations in peripheral and aortic blood pressure: cross-sectional study in healthy subjects aged 2–84 years. High Blood Press. Cardiovasc. Prev. 24(4):437–451, 2017.
Zocalo, Y., M. Marin, S. Curcio, V. Garcia-Espinosa, P. Chiesa, G. Giachetto, E. I. Cabrera-Fischer, and D. Bia. Increases in peripheral systolic pressure levels and z-score associate gradual aortic pressure increase and functional arterial impairment in children and adolescents. Curr. Hypertens. Rev. 14(2):170–182, 2018.
Disclousure of interest
Yanina Zócalo, Alejandro Díaz, and Daniel Bia have no conflicts of interest to declare.
Funding
This work was supported by the Agencia Nacional de Investigación e Innovación (ANII) under Grant (PRSCT-008-020) and Espacio Interdisciplinario (EI) and Comisión Sectorial de Investigación Científica (CSIC-Udelar) of the Republic University, Uruguay. Additionally, this work was supported by extrabudgetary funds generated by CUiiDARTE Centre and Project. None of these organizations influenced the study design or collection, analysis, and interpretation of data; the writing of the report; or the decision to submit the manuscript for publication.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
13239_2019_439_MOESM6_ESM.tif
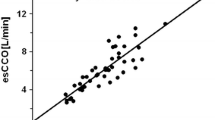
Figure S1 Association analysis (correlation) between cardiac output (CO) obtained by different methods, for the entire group (All) and age related subgroups. Regression and equality lines are shown in each scatter-diagram. (TIFF 656 kb)
13239_2019_439_MOESM7_ESM.tif
Figure S2 Association analysis (correlation) between cardiac output (CO) obtained with different Mobil-O-Graph related signal quality scores, for the entire group (All) and age-related subgroups. Regression and equality lines are shown in each scatter-diagram. (TIFF 230 kb)
Rights and permissions
About this article
Cite this article
Zócalo, Y., Díaz, A. & Bia, D. Cardiac Output Monitoring in Children, Adolescents and Adults Based on Pulse Contour Analysis: Comparison with Echocardiography-Derived Data and Identification of Factors Associated with Their Differences. Cardiovasc Eng Tech 11, 67–83 (2020). https://doi.org/10.1007/s13239-019-00439-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-019-00439-w