Abstract
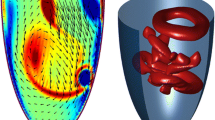
This study aims to investigate the capability of smoothed particle hydrodynamics (SPH), a fully Lagrangian mesh-free method, to simulate the bulk blood flow dynamics in two realistic left ventricular (LV) models. Three dimensional geometries and motion of the LV, proximal left atrium and aortic root are extracted from cardiac magnetic resonance imaging and multi-slice computed tomography imaging data. SPH simulation results are analyzed and compared with those obtained using a traditional finite volume-based numerical method, and to in vivo phase contrast magnetic resonance imaging and echocardiography data, in terms of the large-scale blood flow phenomena usually clinically measured. A quantitative comparison of the velocity fields and global flow parameters between the in silico models and the in vivo data shows a reasonable agreement, given the inherent uncertainties and limitations in the modeling and imaging techniques. The results indicate the capability of SPH as a promising tool for predicting clinically relevant large-scale LV flow information.










Similar content being viewed by others
References
Adami, S. Modeling and Simulation of Multiphase Phenomena with Smoothed Particle Hydrodynamics. München: Technische Universität München, 2014.
Chnafa, C., S. Mendez, and F. Nicoud. Image-based large-eddy simulation in a realistic left heart. Comput. Fluids 94:173–187, 2014.
Christiansen, J. P., T. D. Karamitsos, and S. G. Myerson. Assessment of valvular heart disease by cardiovascular magnetic resonance imaging: a review. Heart Lung Circ. 20(2):73–82, 2011.
Colagrossi, A., and M. Landrini. Numerical simulation of interfacial flows by smoothed particle hydrodynamics. J. Comput. Phys. 191(2):448–475, 2003.
Demirdžić, I., and M. Perić. Space conservation law in finite volume calculations of fluid flow. Int. J. Numer. Methods Fluids 8(9):1037–1050, 1988.
Domenichini, F., et al. Combined experimental and numerical analysis of the flow structure into the left ventricle. J. Biomech. 40(9):1988–1994, 2007.
Doost, S. N., et al. The numerical analysis of non-Newtonian blood flow in human patient-specific left ventricle. Comput. Methods Programs Biomed. 127:232–247, 2016.
Ferziger, J. H., and M. Peric. Computational Methods for Fluid Dynamics. New York: Springer, 2012.
Frayne, R., et al. Accuracy of MR phase contrast velocity measurements for unsteady flow. J. Magn. Reson. Imaging 5(4):428–431, 1995.
Fujimoto, S., et al. Magnetic resonance velocity mapping of normal human transmitral velocity profiles. Heart Vessels 10(5):236–240, 1995.
Guide AB. Version 2016. Providence, RI: Dassault Systémes Simulia Corp, 2016.
Hu, X. Y., and N. A. Adams. A multi-phase SPH method for macroscopic and mesoscopic flows. J. Comput. Phys. 213(2):844–861, 2006.
Hughes, T. J. R., W. K. Liu, and T. K. Zimmermann. Lagrangian–Eulerian finite element formulation for incompressible viscous flows. Comput. Methods Appl. Mech. Eng. 29(3):329–349, 1981.
Imanparast, A., N. Fatouraee, and F. Sharif. The impact of valve simplifications on left ventricular hemodynamics in a three dimensional simulation based on in vivo MRI data. J. Biomech. 49(9):1482–1489, 2016.
Khalafvand, S., L. Zhong, and E. Ng. Three-dimensional CFD/MRI modeling reveals that ventricular surgical restoration improves ventricular function by modifying intraventricular blood flow. Int. J. Numer. Methods Biomed. Eng. 30(10):1044–1056, 2014.
Kilner, P. J., P. D. Gatehouse, and D. N. Firmin. Flow measurement by magnetic resonance: a unique asset worth optimising. J. Cardiovasc. Magn. Reson. 9(4):723–728, 2007.
Kim, W. Y., et al. Left ventricular blood flow patterns in normal subjects: a quantitative analysis by three-dimensional magnetic resonance velocity mapping. J. Am. Coll. Cardiol. 26(1):224–238, 1995.
Kitajima, H. D., et al. Comparison of particle image velocimetry and phase contrast MRI in a patient-specific extracardiac total cavopulmonary connection. J. Biomech. Eng. 130(4):041004, 2008.
Kulp, S., et al. Practical patient-specific cardiac blood flow simulations using SPH. In: Biomedical Imaging (ISBI), 2013 IEEE 10th International Symposium on. IEEE, 2013.
Lantz, J., et al. Patient-specific simulation of cardiac blood flow from high-resolution computed tomography. J. Biomech. Eng. 138(12):121004, 2016.
Le, T. B., and F. Sotiropoulos. On the three-dimensional vortical structure of early diastolic flow in a patient-specific left ventricle. Eur. J. Mech. B 35:20–24, 2012.
Le, T. B., and F. Sotiropoulos. Fluid–structure interaction of an aortic heart valve prosthesis driven by an animated anatomic left ventricle. J. Comput. Phys. 244:41–62, 2013.
Lee, V. S., et al. Flow quantification using fast cine phase-contrast MR imaging, conventional cine phase-contrast MR imaging, and Doppler sonography: in vitro and in vivo validation. AJR 169(4):1125–1131, 1997.
Liu, G.-R. Meshfree Methods: Moving Beyond the Finite Element Method. New York: Taylor & Francis, 2009.
Liu, M., and G. Liu. Smoothed particle hydrodynamics (SPH): an overview and recent developments. Arch. Comput. Methods Eng. 17(1):25–76, 2010.
Liu, X., and C. M. Duraiswamy. N, Fluid–Structure interaction analysis of prosthetic aortic valve using abaqus smoothed particle hydrodynamic (SPH) analysis. In: ASME emerging technologies’ 6th frontiers in biomedical devices conference & exhibition, Irvine, CA, 2011.
Lorenz, C. H., et al. Normal human right and left ventricular mass, systolic function, and gender differences by cine magnetic resonance imaging. J. Cardiovasc. Magn. Reson. 1(1):7–21, 1999.
Maciá, F., et al. Theoretical analysis of the no-slip boundary condition enforcement in SPH methods. Prog. Theor. Phys. 125(6):1091–1121, 2011.
Mao, W., K. Li, and W. Sun. Fluid–structure interaction study of transcatheter aortic valve dynamics using smoothed particle hydrodynamics. Cardiovasc. Eng. Technol. 7(4):374–388, 2016.
Markl, M., et al. Time-resolved 3D MR velocity mapping at 3T: improved navigator-gated assessment of vascular anatomy and blood flow. J. Magn. Reson. Imaging 25(4):824–831, 2007.
Marom, G. Numerical methods for fluid–structure interaction models of aortic valves. Arch. Comput. Methods Eng. 22(4):595–620, 2015.
Marrone, S., et al. An accurate SPH modeling of viscous flows around bodies at low and moderate Reynolds numbers. J. Comput. Phys. 245:456–475, 2013.
Mihalef, V., et al. Patient-specific modelling of whole heart anatomy, dynamics and haemodynamics from four-dimensional cardiac CT images. Interface Focus 1(3):286–296, 2011.
Mittal, R., et al. Computational modeling of cardiac hemodynamics: current status and future outlook. J. Comput. Phys. 305:1065–1082, 2016.
Monaghan, J. J. Smoothed particle hydrodynamics. Annu. Rev Astron. Astrophys. 30:543–574, 1992.
Monaghan, J. A turbulence model for smoothed particle hydrodynamics. Eur. J. Mech. B 30(4):360–370, 2011.
Moosavi, M.-H., et al. Numerical simulation of blood flow in the left ventricle and aortic sinus using magnetic resonance imaging and computational fluid dynamics. Comput. Methods Biomech. Biomed. Eng. 17(7):740–749, 2014.
Morris, J. P., P. J. Fox, and Y. Zhu. Modeling low Reynolds number incompressible flows using SPH. J. Comput. Phys. 136(1):214–226, 1997.
Müller, M., S. Schirm, and M. Teschner. Interactive blood simulation for virtual surgery based on smoothed particle hydrodynamics. Technol. Health Care 12(1):25–31, 2004.
Otto, C. M. Textbook of Clinical Echocardiography. Amsterdam: Elsevier Health Sciences, 2013.
Pedrizzetti, G., et al. The vortex [mdash] an early predictor of cardiovascular outcome? Nat. Rev. Cardiol. 11(9):545–553, 2014.
Peskin, C. S. Flow patterns around heart valves: a numerical method. J. Comput. Phys. 10(2):252–271, 1972.
Saber, N. R., et al. Computational flow modeling of the left ventricle based on in vivo MRI data: initial experience. Ann. Biomed. Eng. 29(4):275–283, 2001.
Saber, N. R., et al. Progress towards patient-specific computational flow modeling of the left heart via combination of magnetic resonance imaging with computational fluid dynamics. Ann. Biomed. Eng. 31(1):42–52, 2003.
Seo, J. H., and R. Mittal. Effect of diastolic flow patterns on the function of the left ventricle. Phys. Fluids (1994-present) 25(11):110801, 2013.
Seo, J. H., et al. Multiphysics computational models for cardiac flow and virtual cardiography. Int. J. Numer. Methods Biomed. Eng. 29(8):850–869, 2013.
Shahriari, S., I. Hassan, and L. Kadem. Validation of a smoothed particle hydrodynamics code for internal flow simulations: application to hemodynamics in a realistic left heart cavity model. In: ASME 2010 3rd Joint US-European Fluids Engineering Summer Meeting collocated with 8th International Conference on Nanochannels, Microchannels, and Minichannels. American Society of Mechanical Engineers, 2010.
Shahriari, S., et al. Smoothed particle hydrodynamics method applied to pulsatile flow inside a rigid two-dimensional model of left heart cavity. Int. J. Numer. Methods Biomed. Eng. 28(11):1121–1143, 2012.
Shahriari, S., I. Hassan, and L. Kadem. Modeling unsteady flow characteristics using smoothed particle hydrodynamics. Appl. Math. Model. 37(3):1431–1450, 2013.
Sinnott, M., P.W. Cleary, and M. Prakash. An investigation of pulsatile blood flow in a bifurcation artery using a grid-free method. In: Fifth International Conference on CFD in the Process Industries, CSIRO, Melbourne, Australia, 2006.
Stankovic, Z., et al. 4D flow imaging with MRI. Cardiovasc. Diagn. Ther. 4(2):173–192, 2014.
Toma, M., et al. Fluid–structure interaction and structural analyses using a comprehensive mitral valve model with 3D chordal structure. Int. J. Numer. Methods Biomed. Eng. 2016. doi:10.1002/cnm.2815.
Uribe, S., et al. Four-dimensional (4D) flow of the whole heart and great vessels using real-time respiratory self-gating. Magn. Reson. Med. 62(4):984–992, 2009.
Vedula, V., et al. Effect of trabeculae and papillary muscles on the hemodynamics of the left ventricle. Theor. Comput. Fluid Dyn. 30(1–2):3–21, 2015.
Violeau, D., and R. Issa. Numerical modelling of complex turbulent free-surface flows with the SPH method: an overview. Int. J. Numer. Methods Fluids 53(2):277–304, 2007.
Wang, Q., et al. Dimensional analysis of aortic root geometry during diastole using 3D models reconstructed from clinical 64-slice computed tomography images. Cardiovasc. Eng. Technol. 2(4):324–333, 2011.
Wang, Q., et al. Simulations of transcatheter aortic valve implantation: implications for aortic root rupture. Biomech. Model. Mechanobiol. 14(1):29–38, 2015.
WHO. Cardiovascular Diseases (CVDs) Fact Sheet. Geneva: WHO, 2016.
Yamaguchi, T., et al. Particle-based methods for multiscale modeling of blood flow in the circulation and in devices: challenges and future directions. Ann. Biomed. Eng. 38(3):1225–1235, 2010.
Zheng, X., et al. Computational modeling and analysis of intracardiac flows in simple models of the left ventricle. Eur. J. Mech. B 35:31–39, 2012.
Zhu, Y., P. J. Fox, and J. P. Morris. A pore-scale numerical model for flow through porous media. Int. J. Numer. Anal. Methods Geomech. 23(9):881–904, 1999.
Acknowledgments
This work was supported in part by the NIH HL104080 and HL127570 Grants. Andrés Caballero is in part supported by a Fulbright-Colciencias fellowship. Wenbin Mao and Liang Liang are in part supported by American Heart Association post-doctoral fellowships, 15POST25910002 and 16POST30210003, respectively. John Oshinski receives research grant support from Siemens Medical Solutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5).
Human and Animal Rights
No animal studies were carried out by the authors for this article.
Informed consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Associate Editors Karyn Kunzelman and Ajit P. Yoganathan oversaw the review of this article.
Appendix
Appendix
Mesh Independence Study
Tests on mesh sensitivity were performed on the LV-CFD models by comparing results obtained with three different mesh densities: coarse (100,000, 150,000 elements), medium (200,000, 270,000 elements), and fine (500,000, 640,000 elements), for Subject 1 and Subject 2, respectively. The \(L_{1}\)- relative error norm (\(E_{L1}\)) of the instantaneous velocity profile along the LVOT plane center line at peak systole for Subject 1 was 8.6% between the coarse and fine meshes, and 4.8% between the medium and fine meshes. For Subject 2, \(E_{L1}\) was 5.2% between the coarse and fine meshes, and 3.9% between the medium and fine meshes. Similarly, \(E_{L1}\) of the instantaneous velocity profile along the MA plane centerline at the E-wave for Subject 1 was 10.3% between the coarse and fine meshes, and about 4.4% between the medium and fine meshes. For Subject 2, \(E_{L1}\) was 9.8% between the coarse and fine meshes, and 4.9% between the medium and fine meshes. A reasonable convergence was therefore achieved on the medium grid resolution in terms of the intraventricular flow field. Therefore, the CFD results presented in this study employed the medium mesh density (Fig. 11).
Rights and permissions
About this article
Cite this article
Caballero, A., Mao, W., Liang, L. et al. Modeling Left Ventricular Blood Flow Using Smoothed Particle Hydrodynamics. Cardiovasc Eng Tech 8, 465–479 (2017). https://doi.org/10.1007/s13239-017-0324-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-017-0324-z