Abstract
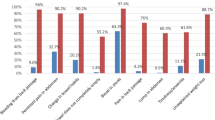
Colorectal and stomach cancers are the top ranking cancers in Oman. Most of the patients are diagnosed at advanced disease stages. The aim of this study is to explore the knowledge of risk factors, symptoms and the time needed to seek medical care for stomach cancer and colorectal cancer (CRC) among Omani participants attending 28 local health centres (LHCs) in the governorate of Muscat, the capital city of Oman. The Bowel Cancer/CRC Awareness Measure (CAM) questionnaire (translated into Arabic) was used to collect data from Omani adult participants (aged 18 years and above) who attended the LHCs during the study period. There was a total of 405 participants in the study out of the 500 who were invited (response rate = 81%). The most recognised risk factors were excessive drinking of alcohol (73.1%) and smoking (70.6%); the least recognised were doing less exercise (37.3%), eating food which was high in salt (26.8%) and a diagnosis of diabetes mellitus (24.9%). Multinomial logistic regression showed that young participants recognised more risk factors than older participants; highly educated participants recognised more risk factors than the less-educated and married participants recognised more risk factors than single participants. Participants with a high level of education were more likely to identify signs and symptoms of stomach cancer and CRC than less-educated participants. Multinomial logistic regression showed women were more likely than men to report barriers to seeking medical help (fear, difficulty in arranging transport, worried what the doctor might find). Also, participants with less education were more likely to report barriers than the highly educated (worried about wasting the doctor’s time, difficulty in arranging transport, did not feel confident talking about symptoms, embarrassed, scared, worried what doctor might find). The majority of participants (93.6%) were not aware of any CRC screening programme or had undergone any screening (98.3) for CRC. Only 52.6% of participants would have a colonoscopy if the doctors advised; the main reasons for refusal were embarrassment (40.0%), lack of trust in the doctors (33.3%) and religious or culture beliefs (21.3%). Around 39% of participants would prefer to have their colonoscopy examination abroad. There is an urgent need to increase the public’s awareness of stomach cancer and CRC in Oman, particularly with evidence emerging of an increase in the incidence. School curriculums could include sessions on cancer education and the information be reiterated to students periodically. A strategy to establish a CRC screening programme in Oman might be paramount as the incidence of CRC increased.



Similar content being viewed by others
References
World Health Organization. Cancer—fact sheet. 2015. http://www.who.int/mediacentre/factsheets/fs297/en/. Updated February 2017 (Accessed 30.5.2017)
Center MM, Jemal A, Ward E (2009) International trends in colorectal cancer incidence rates. Cancer Epidemiol Biomark Prev 18(6):1688
Marley AR, Nan H (2016) Epidemiology of colorectal cancer. Int J Mol Epidemiol Genet 7(3):105–114
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D (2011) Global cancer statistics. CA A Cancer Journal for Clinicians 61(2):69–90
Niksic M, Rachet B, Duffy SW, Quaresma M, Moller H, Forbes LJ (2016) Is cancer survival associated with cancer symptom awareness and barriers to seeking medical help in England? An ecological study. Br J Cancer 115(7):876–886
Al-Azri M, Al-Maskari A, Al-Matroushi S, Al-Awisi H, Davidson R, Panchatcharam SM et al (2016) Awareness of cancer symptoms and barriers to seeking medical help among adult people attending primary care settings in Oman. Health Services Research and Managerial Epidemiology 3:1–10
Oberoi DV, Jiwa M, McManus A, Hodder R (2015) Men’s help-seeking behavior with regards to lower bowel symptoms. Am J Health Behav 39(2):212–221
Pedersen AF, Hansen RP, Vedsted P (2013) Patient delay in colorectal cancer patients: associations with rectal bleeding and thoughts about cancer. PLoS One 8(7):e69700
Weller D (2006) Colorectal cancer in primary care: even with national screening, primary care can do more to cut mortality. BMJ 333(7558):54–55
Esteva M, Leiva A, Ramos MÕ, Pita-Fern_Éndez S, Gonz_Élez-Luj_Én L, Casamitjana M et al (2013). Factors related with symptom duration until diagnosis and treatment of symptomatic colorectal cancer. BMC Cancer 13(1):1–13
Adelstein BA, Macaskill P, Turner RM, Irwig L (2012) Patients who take their symptoms less seriously are more likely to have colorectal cancer. BMC Gastroenterol 12(1):1–9
MacDonald S, Macleod U, Campbell NC, Weller D, Mitchell E (2006) Systematic review of factors influencing patient and practitioner delay in diagnosis of upper gastrointestinal cancer. Br J Cancer 94(9):1272–1280
Simon AE, Waller J, Robb K, Wardle J (2010) Patient delay in presentation of possible cancer symptoms: the contribution of knowledge and attitudes in a population sample from the United Kingdom. Cancer Epidemiol Biomark Prev 19(9):2272–2277
Przybyla AG, Crockett JA, Rex JC, Culumovic PJ (2014) Current screening guidelines overlook a significant number of patients treated for colorectal cancer. Am Surg 80(6):539–543
Ministry of National Economy (2010). Oman census summary http://www.data.gov.om/ (Accessed 30.5.2017)
Al-Lawati JA, Mabry R, Mohammed AJ (2008) Addressing the threat of chronic diseases in Oman. Prev Chronic Dis 5(3):A99
Ministry of Health (2013). Cancer incidence in Oman. Department of Non-Communicable Disease. Directorate General of Primary Health care. Ministry of Health, Sultanat of Oman
Al-Madouj, Eldali A, Al-Zahrani A (2011). Ten-year cancer incidence among nationals of the GCC states 1998–2007 (prepared under the supervision of Executive Board Of Health Ministers’ Council For the Gulf Cooperation Council State
Kumar S, Burney IA, Zahid KF, Souza D, Belushi MA, Mufti TD et al (2015) Colorectal cancer patient characteristics, treatment and survival in Oman: a single center study. Asian Pac J Cancer Prev 16(12):4853–4858
Cancer Research UK University College London, King’s College London, Oxford University. Bowel Cancer Awareness Measure (CAM) toolkit version 2.1. 2011. Cancer Research UK
Power E, Simon A, Juszczyk D, Hiom S, Wardle J (2011) Assessing awareness of colorectal cancer symptoms: measure development and results from a population survey in the UK. BMC Cancer 11(1):366
Al-Azri M, Al-Hamedi I, Al-Awisi H, Al-Hinai M, Davidson R (2015) Public awareness of warning signs and symptoms of cancer in Oman: a community-based survey of adults. Asian Pac J Cancer Prev 16(7):2731–2737
Rahim HF, Sibai A, Khader Y, Hwalla N, Fadhil I, Alsiyabi H et al (2014) Non-communicable diseases in the Arab world. Lancet 383(9914):356–367
Robb K, Stubbings S, Ramirez A, Macleod U, Austoker J, Waller J et al. Public awareness of cancer in Britain: a population-based survey of adults. Br J Cancer 101(S2):S18-S23
Forbes LJL, Simon AE, Warburton F, Boniface D, Brain KE, Dessaix A et al (2013) Differences in cancer awareness and beliefs between Australia, Canada, Denmark, Norway, Sweden and the UK (the International Cancer Benchmarking Partnership): do they contribute to differences in cancer survival? Br J Cancer 108(2):292–300
Al-Azri MH (2016) Delay in cancer diagnosis: causes and possible solutions. Oman Med J 31(5):325–326
Lynes K, Kazmi SA, Robery JD, Wong S, Gilbert D, Thaha MA (2016). Public appreciation of lifestyle risk factors for colorectal cancer and awareness of bowel cancer screening: a cross-sectional study. International journal of surgery 36, part a:312-318
Albano JD, Ward E, Jemal A, Anderson R, Cokkinides VE, Murray T et al (2007) Cancer mortality in the United States by education level and race. J Natl Cancer Inst 99(18):1384–1394
Mulligan CR, Meram AD, Proctor C, Wu H, Zhu K, Marrogi AJ (2006) Unlimited access to care: effect on racial disparity and prognostic factors in lung cancer. Cancer Epidemiol Biomark Prev 15(1):25
Vu M, Azmat A, Radejko T, Padela AI (2016) Predictors of delayed healthcare seeking among American Muslim women. J Women's Health 25(6):586–593
Al-Azri M, Al-Awisi H, Al-Rasbi S, El-Shafie K, Al-Hinai M, Al-Habsi H et al (2014) Psychosocial impact of breast cancer diagnosis among Omani women. Oman Medical Journal 29(6):437
Smith LK, Pope C, Botha JL (2003) Patients’ help-seeking experiences and delay in cancer presentation: a qualitative synthesis. Lancet 366(9488):825–831
Burgess C, Hunter MS, Ramirez AJ (2001) A qualitative study of delay among women reporting symptoms of breast cancer. Br J Gen Pract 51(473):967–971
Caring demands and delay in seeking care in African American women newly diagnosed with breast cancer: an ethnographic, photographic study. 2001
Kumar S, Burney IA, Zahid KF, Souza PC, Belushi MA, Meki TDM et al (2015) Colorectal cancer patient characteristics, treatment and survival in Oman: a single center study. Asian Pac J Cancer Prev 16:4853–4858
Siegel R, DeSantis C, Jemal A (2014) Colorectal cancer statistics. CA A Cancer Journal for Clinicians 64(2):104–117
O'Connell JB, Maggard MA, Livingston EH, Yo CK (2004) Colorectal cancer in the young. Am J Surg 187(3):343–348
Macleod U, Mitchell ED, Burgess C, MacDonald S, Ramirez AJ. Risk factors for delayed presentation and referral of symptomatic cancer: evidence for common cancers. Br J Cancer 101(S2):S92-S101
Quaife SL, Forbes LJL, Ramirez AJ, Brain KE, Donnelly C, Simon AE et al (2014) Recognition of cancer warning signs and anticipated delay in help-seeking in a population sample of adults in the UK. Br J Cancer 110(1):12–18
McCaffery K, Wardle J, Waller J (2003) Knowledge, attitudes, and behavioral intentions in relation to the early detection of colorectal cancer in the United Kingdom. Prev Med 36(5):525–535
Vernon SW (1997) Participation in colorectal cancer screening. A review 89(19):1406–1422
Lansdorp-Vogelaar I, Knudsen AB, Brenner H (2010) Cost-effectiveness of colorectal cancer screening: an overview. Best Pract Res Clin Gastroenterol 24(4):439–449
Bastani R, Gallardo NV, Maxwell AE (2001) Barriers to colorectal cancer screening among ethnically diverse high-and average-risk individuals. J Psychosoc Oncol 19(3–4):65–84
Qumseya BJ, Tayem YI, Dasa OY, Nahhal KW, Abu Limon IM, Hmidat AM et al (2014) Barriers to colorectal cancer screening in Palestine: a national study in a medically underserved population. Clin Gastroenterol Hepatol 12(3):463–469
Hasnain M, Connell KJ, Menon U, Tranmer PA (2010) Patient-centered care for Muslim women: provider and patient perspectives. J Women's Health 20(1):73–83
McLean M, Al Ahbabi S, Al Ameri M, Al Mansoori M, Al Yahyaei F, Bernsen R (2010) Muslim women and medical students in the clinical encounter. Med Educ 44(3):306–315
Alharbi NS, Almutari R, Jones S, Al-Daghri N, Khunti K, de Lusignan S (2014) Trends in the prevalence of type 2 diabetes mellitus and obesity in the Arabian gulf states: systematic review and meta-analysis. Diabetes Res Clin Pract 106(2):e30–e33
Acknowledgments
The authors would like to thank the participants and the Directorate General of Health Services of Muscat governorate for allowing this study to be conducted in the LHCs.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The study has been approved by the Medical Research and Ethics Committee of the College of Medicine and Health Sciences at Sultan Qaboos University, Muscat, Oman (MREC #1088).
Conflict of Interest Statement
The authors declare that they have no conflict of interest.
Funding
None.
Rights and permissions
About this article
Cite this article
Al-Azri, M., Al-Kindi, J., Al-Harthi, T. et al. Awareness of Stomach and Colorectal Cancer Risk Factors, Symptoms and Time Taken to Seek Medical Help Among Public Attending Primary Care Setting in Muscat Governorate, Oman. J Canc Educ 34, 423–434 (2019). https://doi.org/10.1007/s13187-017-1266-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-017-1266-8