Abstract
Purpose
To compare the 18F-NaF PET/CT studies (18F-NaF) with other imaging methods in the detection of skeletal metastases (SM) in patients with medullary thyroid cancer (MTC).
Methods
We retrospectively analyzed 31 patients with MTC who performed 18F-NaF to assess SM. The results of the 18F-NaF were compared with other imaging methods performed for metastasis detection: 99Tc-MDP bone scan (BS), magnetic resonance imaging (MRI), contrast-enhanced CT (CT), and 68Ga-Dotatate and 18F-FDG PET/CT studies. A qualitative analysis comparing the 18F-NaF findings with the ones of the other methods was performed, and the results were classified as superior (>), equal (=), and inferior (<).
Results
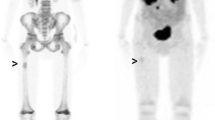
Eleven patients had no bone metastases detected on any of the imaging methods used. Twenty patients presented SM depicted on 18F-NaF. Of these 20 patients, 12 performed bone scan (in 9 18F-NaF > BS and in 3 18F-NaF = BS), 1 performed 18F-FDG (18F-NaF > 18F-FDG), 4 performed 68Ga-Dotatate (in 2 18F-NaF > 68Ga-Dotatate and in 2 18F-NaF = 68Ga-Dotatate), 20 performed CT of at least one body segment (in 15 18F-NaF = CT and in 5 18F-NaF > CT), and 16 performed MRI of at least one body segment, and in all of them, the 18F-NaF was equal to the MRI. Beside this, the 18F-NaF detected SM in body segments not routinely scanned in MRI and CT.
Conclusion
In patients with MTC, the 18F-NaF seems to be equal or superior to other imaging modalities in the detection of SM and allows the analysis of the whole skeletal in a single study.





Similar content being viewed by others
References
Tateishi U, Morita S, Taguri M, Shizukuishi K, Minamimoto R, Kawaguchi M, et al. A meta-analysis of (18)F-fluoride positron emission tomography for assessment of metastatic bone tumor. Ann Nucl Med. 2010;24:523–31.
Iagaru A, Mittra E, Dick DW, Gambhir SS. Prospective evaluation of (99m)Tc MDP scintigraphy, (18)F NaF PET/CT, and (18)F FDG PET/CT for detection of skeletal metastases. Mol Imaging Biol. 2012;14:252–9.
Iagaru A, Young P, Mittra E, Dick DW, Herfkens R, Gambhir SS. Pilot prospective evaluation of 99mTc-MDP scintigraphy, 18F NaF PET/CT, 18F FDG PET/CT and whole-body MRI for detection of skeletal metastases. Clin Nucl Med. 2013;38:e290–6.
Even-Sapir E, Metser U, Mishani E, Lievshitz G, Lerman H, Leibovitch I. The detection of bone metastases in patients with high-risk prostate cancer: 99mTc-MDP Planar bone scintigraphy, single- and multi-field-of-view SPECT, 18F-fluoride PET, and 18F-fluoride PET/CT. J Nucl Med. 2006;47:287–97.
Jambor I, Kuisma A, Ramadan S, Huovinen R, Sandell M, Kajander S, et al. Prospective evaluation of planar bone scintigraphy, SPECT, SPECT/CT, 18F-NaF PET/CT and whole body 1.5T MRI, including DWI, for the detection of bone metastases in high risk breast and prostate cancer patients: SKELETA clinical trial. Acta Oncol. 2016;55:59–67.
Löfgren J, Mortensen J, Rasmussen SH, Madsen C, Loft A, Hansen AE, et al. A prospective study comparing Tc-hydroxyethylene-diphosphonate planar bone scintigraphy and whole-body SPECT/CT with F-fluoride PET/CT and F-fluoride PET/MRI for diagnosing bone metastases. J Nucl Med. 2017;58:1778–85.
Hellwig D, Marienhagen J, Menhart K, Grosse J. Nuclear medicine in Germany. Updated key data and trends from official statistics. Nuklearmedizin. 2017;56:55–68.
Páez D, Orellana P, Gutiérrez C, Ramirez R, Mut F, Torres L. Current status of nuclear medicine practice in Latin America and the Caribbean. J Nucl Med. 2015;56:1629–34.
Van Noorden R. Radioisotopes: the medical testing crisis. Nature. 2013;504:202–4.
Roy M, Chen H, Sippel RS. Current understanding and management of medullary thyroid cancer. Oncologist. 2013;18:1093–100.
Abe K, Adachi I, Miyakawa S, Tanaka M, Yamaguchi K, Tanaka N, et al. Production of calcitonin, adrenocorticotropic hormone, and beta-melanocyte-stimulating hormone in tumors derived from amine precursor uptake and decarboxylation cells. Cancer Res. 1977;37:4190–4.
Mendelsohn G, Wells SA Jr, Baylin SB. Relationship of tissue carcinoembryonic antigen and calcitonin to tumor virulence in medullary thyroid carcinoma. An immunohistochemical study in early, localized, and virulent disseminated stages of disease. Cancer. 1984;54:657–62.
Wells SA Jr, Asa SL, Dralle H, Elisei R, Evans DB, Gagel RF, et al. Revised American Thyroid Association guidelines for the management of medullary thyroid carcinoma. Thyroid. 2015;25:567–610.
Giraudet AL, Vanel D, Leboulleux S, Aupérin A, Dromain C, Chami L, et al. Imaging medullary thyroid carcinoma with persistent elevated calcitonin levels. J Clin Endocrinol Metab. 2007;92:4185–90.
Altehoefer C, Ghanem N, Högerle S, Moser E, Langer M. Comparative detectability of bone metastases and impact on therapy of magnetic resonance imaging and bone scintigraphy in patients with breast cancer. Eur J Radiol. 2001;40:16–23.
Ghanem N, Uhl M, Brink I, Schäfer O, Kelly T, Moser E, et al. Diagnostic value of MRI in comparison to scintigraphy, PET, MS-CT and PET/CT for the detection of metastases of bone. Eur J Radiol. 2005;55:41–55.
Treglia G, Giovanella L. F-Fluoride (F-NaF) PET/CT in medullary thyroid carcinoma: far from evidence, far from guidelines! Eur J Nucl Med Mol Imaging. 2020;47:527–8.
Duarte PS. Letter to the Editor: F-NaF not cited in the EANM practice guideline for PET/CT imaging in medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2020;47:525–6.
Duarte PS, de Castroneves LA, Sado HN, Sapienza MT, de Oliveira Hoff AAF, Buchpiguel CA. Bone and calcified soft tissue metastases of medullary thyroid carcinoma better characterized on F-fluoride PET/CT than on Ga-dotatate PET/CT. Nucl Med Mol Imaging. 2018;52:318–23.
Duarte PS, Marin JFG, Filho GBC, Sapienza MT, Buchpiguel CA. 18F-Fluoride uptake in soft tissue metastases of medullary thyroid carcinoma as a marker of progressive calcification. Clin Nucl Med. 2018;43:848–9.
do Vale RHB, Marin JFG, Duarte PS, Sapienza MT, Buchpiguel CA. Visualization of lymph nodal and hepatic metastases of medullary thyroid carcinoma on 18F-fluoride PET/CT. Clin Nucl Med. 2015;40:895–6.
Ueda CE, Duarte PS, de Castroneves LA, Flávio J, Marin G, Sado HN, et al. Burden of metastatic bone disease measured on 18F-NaF PET/computed tomography studies as a prognostic indicator in patients with medullary thyroid cancer. Nucl Med Commun. 2020;41:469–76.
Choksi P, Papaleontiou M, Guo C, Worden F, Banerjee M, Haymart M. Skeletal complications and mortality in thyroid cancer: a population-based study. J Clin Endocrinol Metab. 2017;102:1254–60.
Vogel T, Wendler J, Frank-Raue K, Kreissl MC, Spitzweg C, Fassnacht M, et al. Bone metastases in medullary thyroid carcinoma: high morbidity and poor prognosis associated with osteolytic morphology. J Clin Endocrinol Metab. 2020;105:2239–46.
Xu JY, Murphy WA Jr, Milton DR, Jimenez C, Rao SN, Habra MA, et al. Bone metastases and skeletal-related events in medullary thyroid carcinoma. J Clin Endocrinol Metab. 2016;101:4871–7.
Giovanella L, Treglia G, Iakovou I, Mihailovic J, Verburg FA, Luster M. EANM practice guideline for PET/CT imaging in medullary thyroid carcinoma. Eur J Nucl Med Mol Imaging. 2020;47:61–77.
Castroneves LA, Coura Filho G, de Freitas RMC, Salles R, Moyses RA, Lopez RVM, et al. Comparison of 68Ga PET/CT to other imaging studies in medullary thyroid cancer: superiority in detecting bone metastases. J Clin Endocrinol Metab. 2018;103:3250–9.
Ota N, Kato K, Iwano S, Ito S, Abe S, Fujita N, et al. Comparison of 18F-fluoride PET/CT, 18F-FDG PET/CT and bone scintigraphy (planar and SPECT) in detection of bone metastases of differentiated thyroid cancer: a pilot study. Br J Radiol. 2014;87:20130444.
Lee S-W, Shim SR, Jeong SY, Kim S-J. Comparison of 5 different PET radiopharmaceuticals for the detection of recurrent medullary thyroid carcinoma: a network meta-analysis. Clin Nucl Med. 2020;45:341–8.
Roberts CC, Daffner RH, Weissman BN, Bancroft L, Bennett DL, Blebea JS, et al. ACR appropriateness criteria on metastatic bone disease. J Am Coll Radiol. 2010;7:400–9.
Haubold-Reuter B, Duewell S, Schilcher B, Marincek B, von Schulthess GK. Fast spin echo MRI and bone scintigraphy in the detection of skeletal metastases. Eur Radiol. 1993;3:316–20.
Frank JA, Ling A, Patronas NJ, Carrasquillo JA, Horvath K, Hickey AM, et al. Detection of malignant bone tumors: MR imaging vs scintigraphy. AJR Am J Roentgenol. 1990;155:1043–8.
Zhou J, Gou Z, Wu R, Yuan Y, Yu G, Zhao Y. Comparison of PSMA-PET/CT, choline-PET/CT, NaF-PET/CT, MRI, and bone scintigraphy in the diagnosis of bone metastases in patients with prostate cancer: a systematic review and meta-analysis. Skelet Radiol. 2019;48:1915–24.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Cristina Emiko Ueda, Paulo Schiavom Duarte, Luciana Audi de Castroneves, George Barbério Coura-Filho, Heitor Naoki Sado, Marcelo Tatit Sapienza, Ana Oliveira Hoff, and Carlos Alberto Buchpiguel declare that they have no conflict of interest.
Ethical Approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed Consent
The institutional review board of our institute approved this study, and the requirement to obtain informed consent was waived.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ueda, C.E., Duarte, P.S., de Castroneves, L.A. et al. Comparison of 18F-NaF PET/CT with Other Imaging Methods in the Detection of Bone Metastases in Patients with Medullary Thyroid Cancer: a Report of a Series of 31 Cases. Nucl Med Mol Imaging 54, 281–291 (2020). https://doi.org/10.1007/s13139-020-00666-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-020-00666-3