Abstract
Introduction
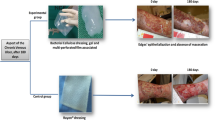
Venous hypertension underlies all clinical manifestations of chronic venous insufficiency (CVI). It is transmitted to the microcirculation and results in capillary changes which lead to edema, skin damage and eventually venous ulceration. The venoactive drugs are believed to have a therapeutic effect in venous disorders. This study evaluated the effect on the healing process of venous leg ulcers of systemic treatment with a semi-synthetic micronized purified flaνοnoid fraction (MPFF).
Material and Method
The study population comprised 60 patients with CVI and venous ulcer of the lower extremities, who were randomised into three groups, each of 20 patients. The patients in group Α, considered as the control group, used only elastic compression stockings. Group Β patients used elastic compression stockings and took MPFF 500mg orally, twice daily, until the complete healing of the ulcer. Group C used elastic compression stockings, and took MPFF 500mg twice daily until the complete healing of the ulcer, plus antibiotics. The ulcer healing rate was measured based on the healing index Η = (D0-Dx/D0) × 100, where D is the day from starting treatment. Venous blood samples were collected from each patient, before, and 20 and 40 days after the beginning of treatment, from the ulceration site and from an upper extremity vein (systemic circulation), for measurement of the white blood cells (WBCs).
Results
Healing time was statistically significantly shorter in groups Β and C than in the control group Α (p = 0.01 and p = 0.001, respectively). The difference between groups Β and C was not significant. Comparison between the initial blood sample and that after 20 days of treatment showed that the WBC trapping rate in the capillaries around the ulcer was reduced by half with the administration of MPFF.
Conclusion
Administration of MPFF has a beneficial effect on capillary permeability and improves the microcirculation, with particular effect on the WBCs trapped in the capillaries around the venous leg ulcer. As a consequence MPFF administration improves the healing rate of the venous ulcers.
Similar content being viewed by others
References
Rabe E, Berboth G, Pannier F. Epidemiology of chronic venous diseases. Wien Med Wochenschr 2016;166:260–3.
Dua A, Desai SS, Heller JA. The impact of race on advanced chronic venous insufficiency. Ann Vasc Surg 2016;34:152–6.
Situm M, Kolić M, Spoljar S. Quality of life and psychological aspects in patients with chronic leg ulcer. Acta Med Croatica 2016;70:61–3.
Nicolaides AN; Cardiovascular Disease Educational and Research Trust; European Society of Vascular Surgery; The International Angiology Scientific Activity Congress Organization; International Union of Angiology; Union Internationale de Phlebologie at the Abbaye des Vaux de Cernay. Investigation of chronic venous insufficiency: A consensus statement (France, March 5-9, 1997). Circulation 2000;102(20):E126–63.
Abbade LP, Lastoria S. Venous ulcer: Epidemiology, physiopathology, diagnosis and treatment. INT J Dermatology 2005;44:449–56.
Fowkers FGR, Evans CJ, Lee AJ. Prevalence and risk factors of chronic venous insufficiency. Angiology 2001;52:S5–S6.
Bergqvist D, Lindholm C, Nelzιn O. Chronic leg ulcers: The impact of venous disease. J Vasc Surg 1999;29:752–5.
Belczak SQ, Sincos IR, Campos W, et al. Veno-active drugs for chronic venous disease: A randomized, double-blind, placebocontrolled parallel-design trial. Phlebology 2014;29:454–60.
Gohel MS, Davies AH. Pharmacological treatment in patients with C4, C5 and C6 venous disease. Phlebology 2010;25(Suppl 1):35–41.
Raffetto JD, Mannello F. Pathophysiology of chronic venous disease. Int Angiol 2014;33:212–21.
Pascarella L, Schonbein GW, Bergan JJ. Microcirculation and venous ulcers: A review. Ann Vasc Surg 2005;19:921–7.
Abbade LP, Lastória S. Venous ulcer: epidemiology, physiopathology, diagnosis and treatment. Review. Int J Dermatol 2005;44:449–56.
Wollina U, Abdel-Naser MB, Mani R. A 2006 review of the microcirculation in skin in patients with chronic venous insufficiency: The problem and the evidence available for therapeutic options. Int J Low Extrem Wounds 2006;5:169–80.
Browse NL, Burnand KG. The cause of venous ulceration. Lancet 1982;2:243–5.
Coleridge Smith P, Thomas P, Scurr JH, et al. Causes of venous ulceration: A new hypothesis. Br Med J 1988;296:1726–7.
Claudy AL, Mirshahi M, Soria C, et al. Detection of undegraded fibrin and tumor necrosis factor alpha in venous leg ulcers. J Am Acad Derm 1991;25:623–7.
Powell CC, Rohrer MJ, Barnard MR, et al. Chronic venous insufficiency is associated with increased platelet and monocyte activation and aggregation. J Vasc Surg 1999;30:844–51.
Wilkinson LS, Bunker D, Edwards JCW, et al. Leukocytes: Their role in the etiopathogenesis of skin damage in venous disease. J Vasc Surg 1993;17:669–75.
Nicolaides AN. Chronic venous disease and the leukocyteendothelium interaction: From symptoms to ulceration. Angiology 2005;56(Suppl 1):11–9.
Duran W, Pappas PJ, Schmid-Schonbein GW. Microcirculatory inflammation in chronic venous insufficiency: Current status and future directions. Microcirculation 2000;7(6 Pt 2):S49–58.
Van Geest AD, Veraart JCJM, Nelemans P, et al. The effect of medical elastic compression stockings with different slope values on edema. Dermatol Surg 2000;26:244–7.
Nelson EA, Harper DR, Prescott RJ, et al. Prevention of recurrence of venous ulceration: randomised controlled trial of cass2 and class 3 elastic compression J Vasc Surg 2006;44:803–8.
Kingsley A. The Wound infection continuum and its application to clinical practice. Ostomy Wound Manage 2003;49(7A Suppl):1–7.
Frank C, Bayoumi I, Westendorp C. Approach to infected skin ulcers. Can Fam Physician 2005;51:1352–9.
Nicolaides AN. From symptoms to leg edema: Efficacy of Daflon 500 mg. Angiology 2003;54(Suppl 1):33–44.
Ramelet AA. Clinical benefits of Daflon 500 mg in the most severe stages of chronic venous insufficiency. Angiology 2001;52(Suppl 1):S49–56.
Katsenis K. Micronized purified flavonoid fraction (MPFF): A review of its pharmacological effects, therapeutic efficacy and benefits in the management of chronic venous insufficiency. Curr Vasc Pharmacol 2005;3:1–9.
Bergan JJ. Chronic venous insufficiency and the therapeutic effects of Daflon 500 mg. Angiology 2005;56(Suppl 1):21–4.
Kranke P, Bennett MH, Martyn-St James M, et al. Hyperbaric oxygen therapy for chronic wounds. Cochrane Database Syst Rev 2012; doi: 10.1002/14651858.
Kavros SJ, Miller JL, Hanna SW. Treatment of ischemic wounds with noncontact, low-frequency ultrasound: The May clinic experience, 2004-2006. Adv Skin Wound Care 2007;20:221–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Katseni, K.K., Bramis, K. & Katsenis, K. Beneficial effect of MPFF administration on the healing process of venous ulcer. Hellenic J Surg 89, 196–202 (2017). https://doi.org/10.1007/s13126-017-0415-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13126-017-0415-1