Abstract
Background
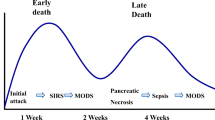
Acute pancreatitis is defined as an acute condition presenting with abdominal pain, and is usually associated with raised pancreatic enzyme levels in the blood or urine, as a result of pancreatic inflammation. Acute pancreatitis may recur, severe episodes, however, may involve a progression to sterile and infected peripancreatic fluid collections, pancreatic necrosis and pancreatic abscess, pancreatic pseudocyst, pancreatic ascites and pancreaticopleural fistulas. These can be divided into acute or delayed, depending on whether such a collection is of less than or more than 4 weeks' duration. Pancreatic Abscess is a circumscribed intra-abdominal collection of pus, usually in proximity to pancreas. Pancreatic abscess is often a late complication of acute necrotizing pancreatitis, occurring more than 4 weeks after the initial attack. The reported mortality rate due to pancreatic abscesses after acute pancreatitis has been 30 to 50%, a statistic that has remained unchanged for decades.
Materials and methods
We report a single case of acute pancreatitis progressing to pancreatic abscess, showing a spectrum phenomenon in evolution of the disease at a tertiary care apex institution of Eastern India.
Similar content being viewed by others
References
Satyajit Bhattacharya. The Pancreas In: Norman S. Williams, Christopher J.K. Bulstrode, P. Ronan O’ Connell. Bailey & Love’s Short Practice of Surgery. 25th Edition. London; Edward Arnold (Publishers) Ltd. 2008;1130–2, 1138-40.
Banks PA, Bollen TL, Dervenis C, et al. Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut 2013;62:102–11.
Warshaw AL, Jin GL. Improved survival in 45 patients with pancreatic abscess. Ann Surg 1985;202:408–17.
Khanna AK, Satyendra K. Tiwary and Puneet Kumar. Pancreatic pseudocyst: Therapeutic dilemma. International Journal of Inflammation 2012; Article ID 279476, 7 pages.
Gukovsky I, Pandol SJ, Mareninova OA, et al. Impaired autophagy and organellar dysfunction in pancreatitis. J Gastroenterol Hepatol 2012;27(Suppl 2):27–32.
Katsohis CD, Jardinoglou E, Basdanis G, et al. Pancreatic abscess following acute pancreatitis. Am Surg 1989;557:427–34.
Pitchumoni CS, Agarwal N. Pancreatic pseudocysts: when and how should drainage be performed? Gastroenterology Clinics of North America 1999;28:615–39.
Siegelman SS, Copeland BE, Saba GP. CT of fluid collections associated with pancreatitis. American Journal of Roentgenology 1980;134:1121–32.
Morgan DE, Baron TH, Smith JK, et al. Pancreatic fluid collections prior to intervention: evaluation with MR imaging compared with CT and US. Radiology 1997;203:773–8.
Brugge WR, Lewandrowski K, Lee-Lewandrowski E et al. Diagnosis of pancreatic cystic neoplasms: a report of the cooperative pancreatic cyst study. Gastroenterology 2004;126:1330–6.
Gumaste VV, Pitchumoni CS. Pancreatic pseudocyst. Gastroenterologist 1996;4:33–43.
Criado E, de Stefano AA, Weiner TM, et al. Long term results of percutaneous catheter drainage of pancreatic pseudocysts. Surgery Gynecology and Obstetrics 1992;175:293–8.
Heider R, Meyer AA, Galanko JA, et al. Percutaneous drainage of pancreatic pseudocysts is associated with a higher failure rate than surgical treatment in unselected patients. Annals of Surgery 1999;229:781–9.
Adams DB, Anderson MC. Percutaneous catheter drainage compared with internal drainage in the management of pancreatic pseudocyst. Annals of Surgery 1992;215:571–8.
Mithöfer K, Mueller PR, Warshaw AL. Interventional and surgical treatment of pancreatic abscess. World Journal of Surgery 1997;21:162–8.
John Jae Park, Sun Suk Kim, Yang Seoh KOO, et al. Definitive treatment of pancreatic abscess by endoscopic transmural drainage. Gie Journal 2002;55:256–62.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pandey, P., Sen, S. Spectrum of acute pancreatitis in a patient- progression of complications. Hellenic J Surg 88, 426–429 (2016). https://doi.org/10.1007/s13126-016-0365-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13126-016-0365-z