Abstract
Background
In severe acute pancreatitis (AP), intravenous glutamine has been shown to reduce the rate of complications, hospital stay, and mortality. In the present randomized trial, we aimed to evaluate the effect of enteral glutamine supplementation on clinical outcomes, gut permeability, systemic inflammation, oxidative stress, and plasma glutamine levels in patients with severe and predicted severe AP.
Methods
Patients with AP admitted within 72 h of onset of symptoms were included. The primary outcome measure was development of infected pancreatic and peri-pancreatic necrosis and in-hospital mortality. High-sensitivity C-reactive protein (HS-CRP) and interleukin-6 (IL-6) were evaluated as markers of inflammation; plasma thiobarbituric acid reactive substances (TBARS) and activities of serum superoxide dismutase and glutathione peroxidase were determined to evaluate oxidative stress; serum polyethylene glycol (PEG) was tested for intestinal permeability; subjective global assessment (SGA) was used for nutritional assessment, and an improvement in organ function was measured by the Modified Marshall score. Intention-to-treat analysis was used. A p-value of < 0.05 was considered statistically significant.
Results
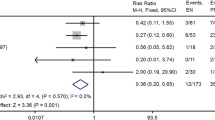
After power calculation, we enrolled 18 patients in the glutamine and 22 in the control arm. There was no significant improvement in the development of infected necrosis and in-hospital mortality between the groups. Improvement in Modified Marshall score was observed in a higher proportion of patients receiving glutamine (15 [83.3%] vs. 12 [54.5%]; p = 0.05). Plasma glutamine levels improved more in glutamine-treated group (432.72 ± 307.83 vs. 618.06 ± 543.29 μM/L; p = 0.004), while it was lower in controls (576.90 ± 477.97 vs. 528.20 ± 410.45 μM/L; p = 0.003). PEG level was lower after glutamine supplementation (39.91 ± 11.97 vs. 32.30 ± 7.39 ng/mL; p = 0.02). Statistically significant reduction in IL-6 concentration was observed in the glutamine group at the end of treatment (87.44 ± 7.1 vs. 63.42 ± 33.7 μM/L; p = 0.02).
Conclusions
Despite absence of improvement in infected necrosis and in-hospital mortality, enteral glutamine supplementation showed improvement in gut permeability, oxidative stress, and a trend towards improvement in organ function as depicted by improvement in the Modified Marshall score.
Trial registration: NCT01503320

Access this article
We’re sorry, something doesn't seem to be working properly.
Please try refreshing the page. If that doesn't work, please contact support so we can address the problem.

Similar content being viewed by others
References
Latifi R, McIntosh JK, Dudrick SJ. Nutritional management of acute and chronic pancreatitis. Surg Clin North Am. 1991;71:579–95.
Gough DB, Boyle B, Joyce W, et al. Free radical inhibition and serial chemiluminescence in evolving experimental pancreatitis. Br J Surg. 1990;77:1256–9.
Chardavoyne R, Asher A, Bank S, Stein TA, Wise L. Role of reactive oxygen metabolites in early cardiopulmonary changes of acute hemorrhagic pancreatitis. Dig Dis Sci. 1989;34:1581–4.
Leser HG, Gross V, Scheibenbogr C, et al. Elevation of serum interleukin-6 concentration precedes acute-phase response and reflects severity in acute pancreatitis. Gastroenterology. 1991;101:782–5.
Norman J. The role of cytokines in the pathogenesis of acute pancreatitis. Am J Surg. 1998;175:76–83.
Banks PA, Freeman ML. Practice guidelines in acute pancreatitis. Am J Gastroenterol. 2006;101:2379–400.
Petrov MS, Shanbhag S, Chakraborty M, Phillips AR, Windsor JA. Organ failure and infection of pancreatic necrosis as determinants of mortality in patients with acute pancreatitis. Gastroenterology. 2010;139:813–20.
Ryan CM, Yarmush ML, Burkee JF, Tompkins RG. Increased gut permeability early afterburns correlates with extent of injury. Crit Care Med. 1992;20:1508–12.
Ryan MC, Schmidt J, Lewandrowski K, et al. Gut macromolecular permeability in pancreatitis correlates with severity of disease in rats. Gastroenterology. 1993;104:890–5.
Novak F, Heyland DK, Avenell A, Drover JW, Su X. Glutamine supplementation in serious illness: a systematic review of the evidence. Crit Care Med. 2002;30:2022–9.
Oudemans-van Straaten HM, Bosman RJ, Treskes M, van der Spoel HJ, Zandstra DF. Plasma glutamine depletion and patient outcome in acute ICU admissions. Intensive Care Med. 2001;27:84–90.
Lin MT, Kung SP, Yeh SL, Liaw KY, Wang MY, Kuo ML, et al. Glutamine-supplemented total parenteral nutrition attenuates plasma interleukin-6 in surgical patients with lower disease severity. World J Gastroenterol. 2005;11:6197–201.
Yao GX, Xue XB, Jiang ZM, Yang NF, Wilmore DW. Effects of perioperative parenteral glutamine-dipeptide supplementation on plasma endotoxin level, plasma endotoxin inactivation capacity and clinical outcome. Clin Nutr. 2005;24:510–5.
Luo M, Bazargan N, Griffith DP, et al. Metabolic effects of enteral versus parenteral alanyl-glutamine dipeptide administration in critically ill patients receiving enteral feeding: a pilot study. Clin Nutr. 2008;27:297–306.
Jo S, Choi SH, Heo JS, et al. Missing effect of glutamine supplementation on the surgical outcome after pancreaticoduodenectomy for periampullary tumors: a prospective, randomized, double-blind, controlled clinical trial. World J Surg. 2006;30:1974–82.
van Stin MF, Ligthart-Melis GC, Boelens PG, et al. Antioxidant enriched enteral nutrition and oxidative stress after major gastrointestinal tract surgery. World J Gastroenterol. 2008;14:6960–9.
Xian-Li H, Qing-Jiu M, Jian-Guo L, Yan-Ku C, Xi-Lin D. Effect of total parenteral nutrition (TPN) with and without glutamine dipeptide supplementation on outcome in severe acute pancreatitis (SAP). Clin Nutr Suppl. 2004;1:43–7.
Xue P, Deng LH, Xia Q, et al. Impact of alanyl-glutamine dipeptide on severe acute pancreatitis in early stage. World J Gastroenterol. 2008;14:474–8.
Filipovic B, Kovcevic N, Randjelovic T, Kostic S, Filipovic B. Nutritional status in hospitalized patients in the Department of Gastroenterohepatology. Hepatogastroenterology. 2011;58:1129–34.
Tinju J, Reshmi S, Rajesh G, Balakrishnan V. Anthropometric, biochemical, clinical, and dietary assessment for malnutrition in south Indian patients with chronic pancreatitis. Trop Gastroenterol. 2010;31:285–90.
Schnelldorfer T, Adams DB. The effect of malnutrition on morbidity after surgery for chronic pancreatitis. Am Surg. 2005;71:466–72.
Dickerson R, Vehe K, Mullen J, Feurer I. Resting energy expenditure in patients with pancreatitis. Crit Care Med. 1991;19:484–90.
Havala T, Shronts E, Cerra F. Nutritional support in acute pancreatitis. Gastroenterol Clin N Am. 1989;18:525–42.
Shaw JHF, Wolfe RR. Glucose, fatty acid, and urea kinetics in patients with severe pancreatitis. The response to substrate infusion and total parenteral nutrition. Ann Surg. 1986;204:665–72.
Helton WS, Jacobs DO, Bonner-Weir S, Bueno R, Smith RJ, Wilmore DW. Effects of glutamine-enriched parenteral nutrition on the exocrine pancreas. JPEN J Parenter Enteral Nutr. 1990;14:344–52.
Singleton KD, Wischmeyer PE. Glutamine’s protection against sepsis and lung injury is dependent on heat shock protein 70 expression. Am J Physiol Regul Integr Comp Physiol. 2007;292:R1839–45.
Doruk N, Buyukakilli B, Atici S, et al. The effect of preventive use of alanyl-glutamine on diaphragm muscle function in cecal ligation and puncture-induced sepsis model. JPEN J Parenter Enteral Nutr. 2005;29:36–43.
Yeh CL, Hsu CS, Yeh SL, Chen WJ. Dietary glutamine supplementation modulates Th1/Th2 cytokine and interleukin-6 expressions in septic mice. Cytokine. 2005;31:329–34.
Oba M, Baldwin RL 4th, Bequette BJ. Oxidation of glucose, glutamate, and glutamine by isolated ovine enterocytes in vitro is decreased by the presence of other metabolic fuels. J Anim Sci. 2004;82:479–86.
Yong L, Lu Q-P, Liu S-H, Hu F. Efficacy of glutamine-enriched nutrition support for patients with severe acute pancreatitis: a meta-analysis. JPEN J Parenter Enteral Nutr. 2016;40:83–94.
Acknowledgments
Dr. M. Sasikala and late Dr. C. Subramanyam for guiding with biochemical evaluation and providing valuable advice; Ms. Merlin Annie Raj for clinical monitoring of patients; Mr. Balakumar Reddy, Mr. Venu, and Mr. Sadik for assisting in laboratory work.
Author information
Authors and Affiliations
Contributions
• Madhulika Arutla recruited and monitored patients, collected data, conducted nutritional and biochemical evaluations, and drafted the manuscript.
• M. Raghunath provided intellectual inputs and mentoring.
• Deepika G supervised biochemical assays.
• Aparna Jakkampudi performed FACS for cytokine assay.
• H.V.V. Murthy performed statistical analyses.
• G. V. Rao recruited patients and provided intellectual inputs.
• D. Nageshwar Reddy recruited patients and provided intellectual inputs.
Corresponding author
Ethics declarations
Conflict of interest
MA, MR, CD, AJ, HVVM, GVR, DNR, and RT declare that they have no conflict of interest.
Ethics statement
The authors declare that the study was performed in a manner conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Prior approval was obtained from the Institutional Review Board (IRBno. AIG/GI/2011/05) of the Asian Institute of Gastroenterology, Hyderabad. Written informed consent was obtained from all the patients before being enrolled in the study.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arutla, M., Raghunath, M., Deepika, G. et al. Efficacy of enteral glutamine supplementation in patients with severe and predicted severe acute pancreatitis— A randomized controlled trial. Indian J Gastroenterol 38, 338–347 (2019). https://doi.org/10.1007/s12664-019-00962-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-019-00962-7