Abstract
Aim
The aim of this study was to assess the stress distribution of the zygomatic implants in maxillectomy cases and to understand the long-term prognosis of this rehabilitation option using finite element analysis.
Materials and Methods
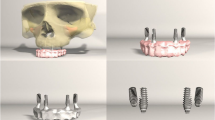
A three-dimensional finite element model was designed using computed tomography of a patient who underwent maxillectomy post-mucormycosis. Zygomatic implants and abutments were designed based on the manufacturer’s design. Quad zygomatic implants were placed in the canine and premolar region into the zygomatic bone bilaterally. A prosthesis with an entire complement of teeth extending from the first molar teeth bilaterally was designed and attached to the multiunit abutments and zygomatic implants. Forces were applied to the zygomatic implants at six different locations bilaterally on the prosthesis which included occlusal and laterally directed forces on the central incisor region, canine region, and molar region using von Mises criteria. A three-dimensional finite element analysis was run, and maximum stress distribution was recorded at various loads. Statistical Package for Social Sciences for Windows version 22.0 Released 2013. Armonk, NY: IBM Corp., was used to perform statistical analyses. Kruskal–Wallis test was used to compare the mean stress values. Multiple comparisons of mean difference in stress values between force applications in implant were done using Dunn’s post hoc test.
Results
The maximum stress was observed at the distal head of the implant in the models. Minimum stress was observed at the apex of the implant in the models. The mean stress values based on force application in the bone and fixed prosthesis showed less significance when compared to the zygomatic implants which was statistically significant at p = 0.03.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Mucormycosis is a devastating oro-facial fungal infection that causes widespread necrosis of bone [1, 2]. It is usually seen in immunocompromised patients [3]. Although its occurrence is rare [0.14% of cases per 1000 population in India] [4], during the second wave of the COVID-19 pandemic, an aggressive presentation of rhino-cerebral mucormycosis was encountered [5]. This resulted in many individuals of different age groups requiring oro-facial rehabilitation [6]. This can be a challenging task owing to the loss of the maxilla which compromises various options for rehabilitation. Various procedures such as basal implants, patient-specific implants, and zygomatic implants [7] which alleviate the need for grafting procedures in the edentulous maxilla [8,9,10] are being used to restore dentition in these patients. However, in these patients, owing to the entire or partial loss of maxilla and/or palatal bone, the role of the support from these structures was called into question while placing zygomatic implants for rehabilitation.
Finite element analysis (FEA) is a powerful tool to evaluate not only stress distribution on implants and abutments on loading with masticatory forces but also helps to evaluate the stress distribution on the bone supporting these implants [11,12,13,14,15]. It is an effective computational tool that has been adapted from the engineering arena to dental implant biomechanics to assess stress [16,17,18,19,20]. This study was done to assess the stress distribution of the zygomatic implants in maxillectomy cases and to understand the long-term prognosis of this rehabilitation option using finite element analysis.
Materials and Methods
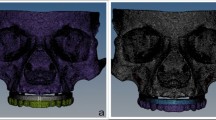
The CT data of an individual patient who underwent maxillectomy [Brown’s Class II] [21] post-mucormycosis were obtained and used for three-dimensional models. The models were exported as STL (stereo lithographic) files which were later imported to blue sky bio software® to optimize polygonal surfaces and generate non-uniform rational B-spline (NURBS) surfaces. The NURBS model was imported to solid models which were used for the finite element analysis.
The rehabilitation of the atrophic maxilla is quite challenging because of the limited bone volume, the complications associated with bone-grafting procedures, patients' morbidity, and cost implications. The minimum number of conventional implants to support a fixed prosthesis in the upper arch is 4 implants; however, in the severely atrophic maxilla, this procedure is not possible without a major bone grafting or sinus augmentation. Since zygomatic implants were introduced as an alternative to bone augmentation, it was considered in our study [22]. Based on the manufacturer’s diagrams, the solid models of zygomatic implants and abutments were designed. Quad zygomatic implants were placed in the canine and premolar region into the zygomatic bone bilaterally. A prosthesis with an entire complement of teeth extending from the first molar teeth bilaterally was also designed and attached to the multiunit abutments. The zygomatic implants along with the dental prosthesis were fabricated together to represent a fixed prosthesis supported by zygomatic implants.
All materials involved in the models were assumed to be isotropic, homogenous, linearly elastic, and static.
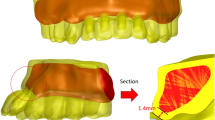
Solid models were made using Creo parametric 3.0 to create a mesh which was generated by Hypermesh 11. Forces stimulating masticatory loads were applied to the zygomatic implants at six different locations on the right and left sides of the prosthesis which included occlusal and laterally directed forces on the central incisor region, canine region, and molar region using von Mises criteria. A magnitude of 50–600 N of forces were analyzed. A 3D FEA was run, and stress distribution was recorded at various loads.
Statistical Package for Social Sciences [SPSS] for Windows version 22.0 Released 2013. Armonk, NY: IBM Corp., was used to perform statistical analyses. Descriptive analysis included the expression of the stress values in terms of mean and standard deviation for each force application. Kruskal–Wallis test was used to compare the mean stress values based on different force applications in implant, bone, and fixed prosthesis and also between implant, bone, and fixed prosthesis based on different force applications. The level of significance was set at p < 0.05. Multiple comparisons of mean difference in stress values between force applications in implant was done using Dunn’s post hoc test.
Results
The mean stress values for the implant at a force of 50 N were 237.180 ± 153.490, for 100 N force was 442.646 ± 163.730, for 300 N force was 842.152 ± 350.208 and at 600 N force was 1770.603 ± 654.908. This difference in the mean stress values for implant at different force application was statistically significant at p = 0.03. (Table 1).
Multiple comparisons of mean difference in the stress values between force applications in implant revealed that 50 N and 150 N force applications showed significantly lesser mean stress values as compared to 300 N and 600 N force, and the mean differences were statistically significant at p = 0.04, respectively. However, no significant difference was observed between 50 and 150 N force and also between 300 and 600 N (Table 2).
The mean stress values for bone at a force of 50 N were 58.560 ± 14.494, for 100 N force was 143.914 ± 108.653, for 300 N force was 287.827 ± 179.748 and at 600 N force was 575.655 ± 359.497. However, this difference in the mean stress values for bone at different force applications was showing a borderline significance at p = 0.08 (Table 1).
The mean stress values for fixed prosthesis at a force of 50 N was 224.102 ± 216.113, for 100 N force was 873.996 ± 616.170, for 300 N force was 1747.992 ± 1232.343 and at 600 N force was 2689.227 ± 2593.364. However, this difference in the mean stress values for fixed prosthesis at different force applications was not statistically significant [p = 0.13] (Table 1).
The maximum stress was observed at the distal head of the implant in the models. Minimum stress was observed at the apex of the implant in the models (Fig. 1). The stress distribution on the bone and fixed prosthesis were low when compared to the stress distribution on the zygomatic implants (Fig. 2).
Considering the force generated during routine mastication of food to be 70 N –150 N, the effect of varying the angle of a 150 N load for the model relative to the occlusal plane is shown in Table 3 (Fig. 3). The stress distribution was observed to be more in the occlusal directed forces rather than the laterally directed forces.
The mean stress values for bone at different force applications [50 N–600 N] showed relatively lesser stress values as compared to implant and fixed prosthesis, which was further followed next by implant showing relatively lesser stress values as compared to fixed prosthesis. However, the mean stress values for different force applications between implant, bone and fixed prosthesis were not statistically significant (Table 4).
Discussion
By understanding the basic theory, method, application, and limitations of FEA in implant dentistry, the clinician will be better equipped to interpret the results of FEA studies and universalize these results to clinical situations [16]. However, to obtain more accurate stress predictions, advanced digital imaging techniques can be applied to model the geometry more realistically; the anisotropic and non-homogenous nature of the material must be considered and the boundary conditions must be carefully treated with the use of computational modeling techniques [16]. This study was done using FEA to assess the stress distribution on the zygomatic implants and surrounding bone in maxillectomy cases. FEA has become a powerful technique in dental implant biomechanics because of its versatility in the calculation of stress distributions within complex structures [23, 24].
The magnitude of forces ranging from 50 N to 600 N was used in this study. While the physiological bite forces have not been measured for zygomatic implants, forces of 450 N were observed in conventional implant-supported bridges [25]. The forces up to 600 N were studied to outdo the forces recorded in vivo. Ujigawa et al. [26] used an FEA model with normal anatomy to investigate the distribution of forces along the zygomatic implants. They simulated a 150 N occlusal force and a 50 N lateral force. Their model incorporated a force of 300 N which was applied to the zygomatic bone and arch to simulate the masseteric action. A large von Mises stress was observed in the zygomatic bone which suggested that most of the occlusal force was transmitted to this area. It is quite difficult to know what proportion of the observed stress in the zygomatic bone was derived from the occlusal force rather than the masseteric force. Therefore our study focused solely on the occlusal forces acting on the implants and masseteric forces were not included in the analysis.
Freedman M. et al. conducted a study to investigate the influence of presence of maxillary alveolar bone on the stress distribution of zygomatic implants with a force ranging from 50 to 600 N. A 3D FEA model was used with and without an alveolar bone to analyze the stress distribution. The differences in stress distribution demonstrated between the two models showed that the model with alveolar bone support was more effective at distributing the applied forces than the model without alveolar support [27]. Miyamoto et al. [25] conducted a study to analyze the stress distributions in craniofacial structures around implant-supported maxillary prostheses. A CT scan of the post-hemimaxillectomy case was used to create a 3D model using DICOM data. Maxillary prostheses were designed with 2 implants in the zygoma on the affected side and 2–3 implants in the maxillary alveolar bone on the unaffected side, without using a cantilever. They concluded that models with alveolar bone support were more effective in distributing the stress to the craniofacial area than those without alveolar bone support. This information was useful for designing maxillary prostheses.In our study also, it was observed that on loading the zygomatic implants, the stress increased within the implants when compared to the bone. This is possibly because of the absence of the maxillary bone which helps in the distribution of forces to the craniofacial skeleton and minimizes the stress distribution on the implant itself.
For patient-specific implants, larger support structures would be required which is the possible drawback and reason for not using it in our study [28]. Thus selecting a zygomatic implant was comparatively more affordable and functional and also was comparably easy to process.
This concludes that the alveolar bone of the maxilla is an essential component for the stress to be distributed along the bone uniformly and not to be internalized by the implant. This could be explained by the fact that the alveolar bone is in close proximity to the masticatory force that is applied. Considering this observation, and the limitations of FEA-related studies, the long-term effect on these implants still needs to be studied in clinical cases.
References
Aswal GS, Rawat R, Dwivedi D, Prabhakar N, Kumar KV (2022) Diagnosis and management of mucormycosis in the dental clinic: a guide for oral health professionals in India. J Fam Med Prim Care 11(8):4293–4298
Samaranayake LP, Fakhruddin KS, Ngo HC, Bandara HM, Leung YY (2022) Orofacial mycoses in coronavirus disease-2019 (COVID-19): a systematic review. Int Dent J 72:S0020-6539
Sridhara SR, Paragache G, Panda NK, Chakrabarti A (2005) Mucormycosis in immunocompetent individuals: an increasing trend. J Otolaryngol 34(6):402
Skiada A, Pavleas I, Drogari-Apiranthitou M (2020) Epidemiology and diagnosis of mucormycosis: an update. J Fungi 6(4):265
Aranjani JM, Manuel A, Abdul Razack HI, Mathew ST (2021) COVID-19—associated mucormycosis: evidence-based critical review of an emerging infection burden during the pandemic’s second wave in India. PLoS Negl Trop Dis 15(11):e0009921
Dos Santos RL, Viveiros SK, De Sousa SC, Sugaya NN, Dias RB, Coto NP, Paula CR (2020) Rhinocerebral mucormycosis: diagnosis, treatment, and buccomaxillofacial rehabilitation. Oral Surg Oral Med Oral Pathol Oral Radiol 130(3):e116–e117
Romeed SA, Hays RN, Malik R, Dunne SM (2015) Extrasinus zygomatic implant placement in the rehabilitation of the atrophic maxilla: three-dimensional finite element stress analysis. J Oral Implantol 41(2):e1-6
Kaman S, Atil F, Tekin U, Ozgul O, Önder ME, Yilmaz S, Gungor H, Kocyigit ID (2017) Stress analysis of zygomatic implants on the augmented maxillary sinus: is it necessary to graft? Implant Dent 26(6):860–867
Ferrara ED, Stella JP (2004) Restoration of the edentulous maxilla: the case for the zygomatic implants. J Oral Maxillofac Surg 62(11):1418–1422
Brånemark PI, Gröndahl K, Öhrnell LO, Nilsson P, Petruson B, Svensson B, Engstrand P, Nannmark U (2004) Zygoma fixture in the management of advanced atrophy of the maxilla: technique and long-term results. Scand J Plast Reconstr Surg Hand Surg 38(2):70–85
Chopade SR, Madhav VN, Palaskar J (2014) Finite element analysis: New dimension in prosthodontic research. J Dent Allied Sci 3(2):85
Boccaccio A, Ballini A, Pappalettere C, Tullo D, Cantore S, Desiate A (2011) Finite element method (FEM), mechanobiology and biomimetic scaffolds in bone tissue engineering. Int J Biol Sci 7(1):112–132
Jianping G, Yan W, Wei Y (2008) Application of finite element analysis in implant dentistry. Springer, China, pp 81–82
Poiate IA, Vasconcellos AB, Santana RB, Poiate E Jr (2009) Three-dimensional stress distribution in the human periodontal ligament in masticatory, parafunctional, and trauma loads: finite element analysis. J Periodontol 80:1859–1867
Morneburg TR, Pröschel PA (2002) Measurement of masticatory forces and implant loads: a methodologic clinical study. Int J Prosthodont 15(1):20–7
Corvello PC, Montagner A, Batista FC, Smidt R, Shinkai RS (2011) Length of the drilling holes of zygomatic implants inserted with the standard technique or a revised method: a comparative study in dry skulls. J Cranio-Maxillofac Surg 39(2):119–123
Geng JP, Tan KB, Liu GR (2001) Application of finite element analysis in implant dentistry: a review of the literature. J Prosthet Dent 85(6):585–598
Wang M, Qu X, Cao M, Wang D, Zhang C (2013) Biomechanical three-dimensional finite element analysis of prostheses retained with/without zygoma implants in maxillectomy patients. J Biomech 46(6):1155–1161
Neena AF Three dimensional finite element analysis to evaluate stress distribution around implant retained mandibular overdenture using two different attachment systems. Doctoral dissertation, Alexandria University
Joshi S, Kumar S, Jain S, Aggarwal R, Choudhary S, Reddy NK (2019) 3D finite element analysis to assess the stress distribution pattern in mandibular implant-supported overdenture with different bar heights. J Contemp Dent Pract 20(7):794–800
Brown JS, Rogers SN, McNally DN, Boyle M (2000) A modified classification for the maxillectomy defect. Head Neck J Sci Spec Head Neck 22(1):17–26
Stiévenart M, Malevez C (2010) Rehabilitation of totally atrophied maxilla by means of four zygomatic implants and fixed prosthesis: a 6–40-month follow-up. Int J Oral Maxillofac Surg 39(4):358–363
Merdji A, Bouiadjra BB, Chikh BO, Mootanah R, Aminallah L, Serier B, Muslih IM (2012) Stress distribution in dental prosthesis under an occlusal combined dynamic loading. Mater Des 36:705–13
Reddy MS, Sundram R, Abdemagyd HA (2019) Application of finite element model in implant dentistry: a systematic review. J Pharm Bioallied Sci 11(Suppl 2):S85
Miyamoto S, Ujigawa K, Kizu Y, Tonogi M, Yamane GY (2010) Biomechanical three-dimensional finite-element analysis of maxillary prostheses with implants. Design of number and position of implants for maxillary prostheses after hemimaxillectomy. Int J Oral Maxillofac Surg 39(11):1120–1126
Ujigawa K, Kato Y, Kizu Y, Tonogi M, Yamane GY (2007) Three-dimensional finite elemental analysis of zygomatic implants in craniofacial structures. Int J Oral Maxillofac Surg 36(7):620–625
Freedman M, Ring M, Stassen LF (2013) Effect of alveolar bone support on zygomatic implants: a finite element analysis study. Int J Oral Maxillofac Surg 42(5):671–676
Shaikh MQ, Nath SD, Akilan AA, Khanjar S, Balla VK, Grant GT, Atre SV (2021) Investigation of patient-specific maxillofacial implant prototype development by metal fused filament fabrication (MF3) of Ti–6Al–4V. Dent J 9(10):109
Funding
No funds, grants, or any other support was received. Authors declare they have no financial interests.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical Approval
Approval was obtained from the Ethics Committee of Navodaya Dental College and Hospital. The procedures used in this study adheres to the tenets of the Declarartion of Helsinki.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rathod, D.K., Chakravarthy, C., Suryadevara, S.S. et al. Stress Distribution of the Zygomatic Implants in Post-mucormycosis Case: A Finite Element Analysis. J. Maxillofac. Oral Surg. 22, 695–701 (2023). https://doi.org/10.1007/s12663-023-01914-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-023-01914-7