Abstract
Purpose
Intralipid® (ILE), a clinically used lipid emulsion, reduces ischemia-reperfusion (IR) injury in healthy and infarct-remodelled rat hearts. We tested whether ILE is also cardioprotective in large porcine hearts in the context of the donation after circulatory death (DCD) model, where human hearts are procured for transplantation after cardiac arrest and thus are exposed to significant IR injury.
Methods
After induction of anesthesia, surgical preparation, termination of ventilator support, and cardiac arrest, hearts of female pigs were procured following a 15 min standoff period, with an optimized normokalemic crystalloid adenosine-lidocaine cardioplegia. Hearts were then randomly allocated to ex vivo reperfusion (38°C) in the absence (control) or presence of 1% ILE. All hearts were perfused with blood and Krebs-Henseleit solution (1:1) for 30 min in Langendorff mode and for an additional 30 min in working mode to assess mechanical function. Left ventricular (LV) biopsies were obtained after five minutes of reperfusion and LV tissue was preserved at the end of reperfusion for biochemical analyses and immunohistochemistry.
Results
Intralipid® postconditioning reduced cell membrane damage as assessed by the mean (standard deviation) leakage of myocardial glutathione disulfide (39 (9) nmol·mg−1 protein vs 19 (7) nmol·mg−1 protein; P = 0.006), protected LV tissue from protein carbonylation (3.4 [0.6] nmol·mg−1 protein vs 5.3 [0.9] nmol·mg−1 protein; P = 0.006), decreased myeloperoxidase activity (35 [8] nmol·min−1·mg−1 protein vs 75 [11] nmol·min−1·mg−1 protein; P < 0.001), and increased inotropy (maximum rate of rise of LV pressure 2001 [345] mmHg·sec−1vs 1584 [192] mmHg·sec−1; P = 0.044). Intralipid® postconditioning triggered reactive oxygen species signalling at early reperfusion and activated protection signalling (Akt, signal transducer and activator of transcription 3, and glycogen synthase kinase 3β) in LV tissue, recapitulating all features of ILE-mediated protection reported in small rodent hearts.
Conclusions
Our data show that ILE postconditioning elicits protection signalling in large mammalian hearts while mimicking clinical conditions, and is capable of enhancing protection of DCD hearts.
Résumé
Objectif
Intralipid® (ILE), une émulsion lipidique utilisée en clinique, réduit les lésions d’ischémie-reperfusion (IR) dans des modèles de cœurs de rats sains et remodelés par infarctus. Nous avons testé l’ILE afin de déterminer si cet agent conservait ses propriétés cardioprotectrices dans de plus gros cœurs porcins dans le contexte d’un modèle de don après décès cardiocirculatoire (DDC), situation au cours de laquelle un cœur humain est prélevé pour être transplanté après un arrêt cardiaque et, par conséquent, exposé à une importante lésion d’IR.
Méthode
Après l’induction de l’anesthésie, la préparation chirurgicale, l’interruption de la ventilation mécanique et l’arrêt cardiaque, des cœurs de truies ont été prélevés après une période latente de 15 minutes, avec la perfusion d’une solution optimisée de cardioplégie à base de cristalloïde normokaliémique avec de l’adénosine et lidocaïne. Les cœurs ont ensuite été aléatoirement alloués à une reperfusion ex vivo (38°C) en l’absence (témoin) ou en présence de 1 % ILE. Tous les cœurs ont été perfusés avec une solution de sang et de Krebs-Henseleit à un ratio 1:1 pendant 30 minutes dans un montage de Langendorff et durant 30 min supplémentaires afin d’évaluer la fonction mécanique. Des biopsies du ventricule gauche (VG) ont été réalisées après cinq minutes de reperfusion, et le tissu VG a été conservé à la fin de la reperfusion à des fins d’analyses biochimiques et d’immunocytochimie.
Résultats
Le post-conditionnement avec Intralipid® a eu les effets suivants : réduction des lésions aux membranes cellulaires, tel qu’évaluées par la fuite moyenne (écart type) de disulfide de glutathion myocardique (39 (9) nmol·mg−1 protéine vs 19 (7) nmol·mg−1 protéine; P = 0,006); protection du tissu VG de la carbonylation protéique (3,4 [0,6] nmol·mg−1 protéine vs 5,3 [0,9] nmol·mg−1 protéine; P = 0,006); réduction de l’activité de la peroxydase leucocytaire (35 [8] nmol·min−1·mg−1 protéine vs 75 [11] nmol·min−1·mg−1 protéine; P < 0,001); et augmentation de l’inotropie (taux maximal d’augmentation de la pression VG 2001 [345] mmHg·sec−1vs 1584 [192] mmHg·sec−1; P = 0,044). Le post-conditionnement avec Intralipid® a provoqué la signalisation de dérivés réactifs de l’oxygène au début de la reperfusion et activé une signalisation de protection (Akt, transducteur de signal et activateur de transcription 3, et glycogène synthase kinase 3β) dans le tissu du VG, reproduisant toutes les caractéristiques de la protection procurée par l’ILE rapportées dans les cœurs de petits rongeurs.
Conclusion
Nos données montrent que le post-conditionnement avec ILE élicite des signaux de protection dans les cœurs de gros mammifères tout en imitant les conditions cliniques, et peut améliorer la protection des cœurs de DDC.
Similar content being viewed by others
Heart transplantation remains the gold standard therapy for end-stage cardiac failure. Unfortunately, the demand for donor hearts for transplantation is far higher than the supply and many patients die while waiting for a suitable donor heart. Donation after circulatory death (DCD) could markedly expand the pool of donor hearts and likely satisfy the ever-increasing organ demand. In fact, there is a growing contribution of DCD organ donations (e.g., kidney and liver) to transplant rates in Canada.1 Nevertheless, in other jurisdictions such as Australia, New Zealand, and the United Kingdom, DCD heart transplantation is only beginning to be used clinically.2
Ischemia-reperfusion (IR) injury is a major problem in cardiac transplantation,3 specifically in the DCD context,4 where interventions to reduce IR injury can only be initiated at the time of organ procurement (and after cardiac arrest). Ex vivo heart perfusion (EVHP) has emerged as an alternative technique to cold storage as it preserves the donated heart in a perfused, semi-physiologic state and allows a thorough assessment of donor heart viability. Additionally, it might be used to further improve organ preservation for longer periods.5
We have previously shown that controlled initial reperfusion of the DCD heart can result in optimization of functional recovery compared with standard recovery techniques.6,7 These studies focused on the initial reperfusion period of the donor heart, without subsequent further intervention during EVHP. Nevertheless, pharmacologic postconditioning, which is known to enhance innate endogenous protective cellular mechanisms within the myocardium resulting in improved recovery after IR injury, has not been well explored in the DCD context. Only one study using a cocktail of erythropoietin, glycerol trinitrate, and zoniporide (a Na+/H+ exchange inhibitor) reported improved cardioprotection when added to the cardioplegia given at the time of procurement in the donor.8 Further intervention during EVHP was not explored in those studies.
We and others have previously reported the protective effects of postconditioning with clinically used lipid emulsions such as Intralipid® (ILE) in healthy and diseased rodent hearts.9,10,11,12 Our studies deciphered the upstream mechanisms of protection by demonstrating that the fatty acid intermediate, palmitoylcarnitine (a metabolite released from ILE) inhibits mitochondrial complex IV, thus releasing reactive oxygen species (ROS) from the electron transport chain at the onset of reperfusion and activating the reperfusion injury salvage kinase pathway.11 Hence, redox mechanisms are essential for cardioprotection and small amounts of ROS released at the onset of reperfusion initiate protection signalling13,14,15,16,17 as opposed to the sustained detrimental ROS production during reperfusion, which causes cell death.18 Our experiments also provided evidence that no cardiotonic action, arising from acceleration of acetyl CoA production due to supplementation of fatty acids, is involved in the protection by ILE postconditioning.12
Here, we explored the cardioprotective potential of ILE postconditioning during ex vivo perfusion in a porcine model of DCD heart donation. Our endeavor is one of the first steps in the ongoing process of bench-to-bedside research translation in the field of cardioprotection. A previously optimized initial reperfusion protocol with normokalemic adenosine-lidocaine cardioplegic solution and avoidance of hypothermia during initial reperfusion was used as a control/standard treatment.6,7 We hypothesized that ILE postconditioning would enhance mechanical function of DCD hearts and reduce oxidative and cellular damage even with a previously optimized procurement and preservation protocol. We further hypothesized that ILE postconditioning would elicit all protective signalling features in this large animal model—mimicking conditions closer to the human heart—that we previously reported in small rodent hearts.
Methods
This investigation conforms to the Canadian Council on Animal Care Guidelines and has received approval from the University of Alberta Animal Care and Use Committee (original approval date: July 31, 2015) and adheres to the ARRIVE guidelines (https://www.nc3rs.org.uk/arrive-guidelines) in its reporting as far as possible. All chemicals were from Millipore-Sigma Canada Ltd. (Oakville, ON, Canada), unless otherwise stated. Please see Table 1 for the abbreviation definitions.
Donation after circulatory death heart procurement and cardioplegia
Sexually immature female (14-16 weeks of age) Yorkshire pigs with a mean (SD) weight of 50 (5) kg were sedated with an intramuscular injection of ketamine (20 mg·kg−1). Orotracheal intubation was enabled with additional xylazine (0.9 mg·kg−1) via the ear vein and inhalational isoflurane as needed. Anesthesia was maintained with isoflurane (2-3%). A median sternotomy was performed and the pericardium opened. Sheath cannulae (5-6 F) were placed into the internal jugular vein and common carotid artery to monitor central venous and aortic pressures, respectively. After normovolemic hemodilution with 1,000 mL of Ringer’s solution and heparinization (1,000 U·kg−1), 750 mL of blood was collected, mixed with 750 mL of modified Krebs-Henseleit solution (containing KCl (4.6 mmol·L−1), NaCl (85 mmol·L−1), NaHCO3 (25 mmol·L−1), NaH2PO4 (1.2 mmol·L−1), MgCl2 (1.2 mmol·L−1), CaCl2 (1.25 mmol·L−1), glucose (10 mmol·L−1), Na-pyruvate (5 mmol·L−1), and 8% bovine serum albumin) and used for priming of the EVHP circuit (mean [SD] hemoglobin of 6 [0.5] g·dL−1). Isoflurane was briefly increased to 5%, inspired oxygen was reduced to 21%, mechanical ventilation was discontinued, and the pigs were extubated to induce asphyxiation resulting in hypoxic cardiac arrest. Circulatory death was defined when the central venous pressure equaled the mean arterial blood pressure or when there was loss of pulsatility on the arterial pressure recording. After a warm ischemic 15-min standoff period, the ascending aorta was cross-clamped and normokalemic adenosine-lidocaine cardioplegic solution (containing NaCl (111.8 mM), KCl (5.9 mM), CaCl2 (0.22 mM) MgCl2 (2.6 mM), NaHCO3 (32 mM), NaH2PO4 (1.2 mM), glucose (10 mM), mannitol (120 mM), pyruvate (1 mM), adenosine (400 µM), lidocaine (500 µM), and insulin (10 IU·L−1)7 was delivered antegrade into the aortic root.
Ex vivo heart perfusion and assessment of myocardial function
Hearts were perfused using a previously described circuit consisting of a venous reservoir, oxygenator, and two centrifugal pumps.5 Hearts were stimulated with a continuous infusion of insulin (2 units·hr−1) and epinephrine (0.04 µg·min−1) added to the perfusate. Computer-controlled pumps with automated feedback loops were used to precisely control diastolic aortic pressure (40 mmHg) and left atrial pressures. Hearts were perfused in the Langendorff mode for 30 min using an aortic root pressure of 40 mmHg and then were transitioned to perfusion in working mode (left atrial pressure of 6 mmHg and aortic root pressure of 40 mmHg) for an additional 30 min. Oxygen and gas flow were titrated to maintain a pH between 7.25-7.35, partial pressure of oxygen between 100-200 mmHg, and PaCO2 between 35-45 mmHg. The coronary sinus blood flow and left atrial flow were measured with a flow module and clamp-on flow probes (Transonic Systems Inc., Ithaca, NY, USA). After a working mode was established, a fluid-filled ventricular 5F pigtail catheter (Cordis, Milpitas, CA, USA) was placed in the left ventricle via the aortic valve. Hearts were randomly assigned to postconditioning with Intralipid® (20% added to the perfusate to achieve a final concentration of 1%, n = 5) or no treatment (control/standard, n = 5). After completion of a five-minute initial reperfusion period in the non-working mode, a left apical ventricular biopsy was collected and immediately processed to measure ROS production, and remnant tissue was snap-frozen in liquid nitrogen for immunoblotting. Aortic root pressure was subsequently increased to 60 mmHg and hearts were gradually rewarmed to 38°C during a 30-min period. A working heart mode was established after 30 min of reperfusion by increasing the left atrial pressure to 6 mmHg. Steady-state functional parameters were obtained from the pigtail catheter inserted into the LV through the aortic valve 60 min after reperfusion.
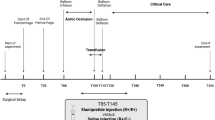
An in-house custom-made data acquisition platform was used to collect functional data. Preload recruitable stroke work was assessed by a gradual reduction in preload pressure/flow and plotting LV stroke work against left atrial pressure. Left ventricular tissue was snap-frozen in liquid nitrogen at the end of reperfusion and stored for biochemical analysis. Additional LV tissue samples were collected in optimal cutting temperature compound and used for histochemical analysis. Left ventricular tissue from four non-ischemic, non-perfused porcine hearts served as aerobic controls (for immunoblot and biochemical analyses). Figure 1 provides an overview of the study protocol.
Study protocol of Intralipid® (ILE) postconditioning in the porcine donation after circulatory death (DCD) model. Donation after circulatory death hearts were rendered ischemic after termination of ventilator support. An additional standoff period of 15 min after confirmation of circulatory arrest was established, after which hearts were procured with optimized cardioplegia containing adenosine and lidocaine. Hearts were reperfused ex vivo, either with perfusate alone (IR) or perfusate supplemented with 1% Intralipid® (IR/ILE) for one hour. A left ventricular (LV) biopsy was collected after five minutes of reperfusion for the measurements of reactive oxygen species (ROS) production and biochemical analyses. Assessments of mechanical function were performed in the working heart mode at the end of the protocol. Left ventricular tissue samples were collected at the end of the protocol for biochemical analyses and histology
Amplex Red assay for the determination of mitochondrial hydrogen peroxide (H2O2) release in permeabilized LV fibres
Cardiac biopsies from the LV apex (collected at five minutes of reperfusion) were prepared for the Amplex Red assay (Invitrogen, Carlsbad, CA, USA) as previously described.11,12 The online electronic supplementary material (eTable) provides additional technical details (page 1).
Protein carbonylation
Protein carbonylation, an indicator of protein oxidation, was measured in LV tissue using an ELISA kit (Protein Carbonyl Content Assay Kit, Cat# ab126287; Abcam Inc, Cambridge, MA, USA). This assay has a detection limit of 0.15 nmol carbonyl per mg protein.
Glutathione tissue content
Total glutathione content, a sensitive marker of cellular damage indicating leakage through the cell membrane, was measured in LV tissue using a fluorometric assay kit (cat# K264-100; BioVision, Inc., Milpitas, CA, USA).
Myeloperoxidase (MPO) tissue content and activity
Frozen LV tissue samples were rinsed in 50 mM phosphate buffer twice to remove excess blood and then homogenized. The supernatant was collected after centrifuging at 5,000 g for five minutes and immediately used for these assays. Page 2 of the online electronic supplementary material (eTable) provides further technical details.
Immunoblotting
Left ventricular total tissue lysates were prepared from samples collected at five minutes of reperfusion and at end of the perfusion protocol. Subcellular fractionations of mitochondria were prepared by differential centrifugation as previously described (eTable, page 3).19
Histochemistry
Hematoxylin/eosin and Oil Red staining were performed according to standard protocols (eTable, page 3)
Statistical analysis
All results were tested for normality (Shapiro-Wilk test) and summarized as mean (SD) for the indicated number (n) of independent observations and presented as dot blots. The significance of differences between two normally distributed treatment groups was determined using a two-tailed t test. Differences were considered significant if the P < 0.05. SigmaPlot (version 13.0; Systat Software, Inc, Chicago, IL, USA) was used for the analyses. Based on previous studies in the DCD context6,7 and the initial report that ILE postconditioning specifically improved the maximal rate of increase in LV pressure (dP/dtmax),9 we used dP/dtmax as the primary endpoint of post-ischemic functional recovery in the current study. A sample size of n = 4 per group was calculated a priori with a power of 80% and a two-sided 5% type I error rate by assuming a mean functional recovery of dP/dtmax of 1,600 in untreated controls and of 2,000 mmHg·sec−1 in ILE-treated hearts (20% improved function) with an SD of 300 mmHg·sec−1 based on previously reported study results.5 The sample size was increased to n = 5 per group to account for potential dropouts. All other outcomes were considered secondary endpoints and no multiplicity adjustments were applied.
Results
Intralipid® postconditioning improves post-ischemic LV function and attenuates cellular damage in porcine DCD hearts
Intralipid® postconditioning improved the mean (SD) dP/dtmax from 1584 (192) to 2001 (345) mmHg·sec−1 (mean difference, − 417 mmHg·sec−1; 95% confidence interval [CI], − 820 mmHg·sec−1 to − 15 mmHg·sec−1; P = 0.04), corresponding to an increase in inotropy of 25% on average after 60 min of reperfusion (Table 2). Developed pressure was also higher in ILE-treated hearts (mean difference, − 17 mmHg·sec−1; 95% CI, − 32 mmHg·sec−1 to − 1 mmHg·sec−1; P = 0.04), but other parameters such as preload recruitable stroke work, cardiac output (measured from left atrial flow rates in the working mode), and coronary flow (measured from pulmonary artery flow rates in the working mode) only showed small improvements, which did not reach statistical significance (Table 2). Glutathione tissue content (mean difference, − 25 nmol·mg−1 protein; 95% CI, − 43 nmol·mg−1 protein to − 7 nmol·mg−1 protein; P = 0.01) and the amount of glutathione disulfide (mean difference, − 20 nmol·mg−1 protein; 95% CI, − 31 nmol·mg−1 protein to − 8 nmol·mg−1 protein; P = 0.006) were significantly higher in hearts protected with ILE postconditioning (Fig. 2A), indicating less leakage from the myocardium in response to IR injury and hence less cell damage.
Cardioprotection by Intralipid® (ILE) postconditioning in porcine donation after circulatory death (DCD) hearts. Panel A) Total glutathione content and glutathione disulfide (GSSG) content of cardiac tissue determined in control (IR) and ILE postconditioned hearts (IR/ILE). Panel B) Protein carbonylation as measured in total tissue extract of control (IR) and ILE postconditioned hearts (IR/ILE). Panel C) Myeloperoxidase (MPO) activity in control (IR) and ILE postconditioned hearts (IR/ILE). Panel D) Myeloperoxidase content in control (IR) and ILE postconditioned hearts (IR/ILE). Data are mean (SD) and dots represent individual experiments. n = 5 for each group
Intralipid® postconditioning reduces oxidative damage in the LV of porcine DCD hearts
To determine whether ILE postconditioning attenuates oxidative damage, we measured protein carbonylation in LV tissue. Intralipid® postconditioning markedly decreased tissue carbonylation on average by 35% (mean difference, 1.9 nmol·mg−1 protein; 95% CI, 0.7 nmol·mg−1 protein to 3.1 nmol·mg−1 protein; P = 0.006) compared with control hearts (Fig. 2B). The carbonylation tissue level in ILE-treated hearts was not different from the average level measured in the four aerobic porcine hearts not subjected to IR (ILE postconditioning [n = 5]: 3.4 (0.6) vs aerobic samples [n = 4]: 3.3 (1) nmol·mg−1 protein, P = 0.98).
Intralipid® postconditioning reduces activation of MPO in porcine DCD hearts during reperfusion
Since previous studies emphasized the importance of preventing leukocyte activation during reperfusion,20,21 we tested whether ILE postconditioning would alter MPO activity and content, which are markers of leukocyte activation and tissue infiltration. Intralipid® postconditioning markedly reduced MPO activity compared with control hearts (mean difference, 41 nmol·min−1·mg−1 protein; 95% CI, 27 nmol·min−1·mg−1 protein to 54 nmol·min−1·mg−1 protein; P < 0.001) (Fig. 2C), and the observed levels were similar to those measured in aerobic control hearts not subjected to IR injury (ILE postconditioning [n = 5]: 35 (8) vs aerobic samples [n = 4]: 27 (2) nmol·min−1·mg−1, P = 0.33). Myeloperoxidase content was not increased (Fig. 2D), consistent with the absence of leukocyte tissue infiltration at earlier stages of reperfusion. To confirm that mononuclear cells did not accumulate in the vessels or LV tissue, immunohistochemical staining of CD11 (a marker of leukocytes) and CD31 (a marker of the endothelium) was performed. The staining confirmed the absence of leukocyte accumulation in the LV tissue and the vasculature (Figs 3A-H).
Histochemical evaluation of left ventricular (LV) tissue collected after 60 min of reperfusion in control (IR) and ILE (Intralipid®) treated (IR/ILE) porcine hearts. Panel A) Hematoxylin/eosin staining (magnification 10x) showing no difference between treatment groups. Oil Red O (ORO) staining showing no accumulation of fat droplets in cardiac tissue of ILE-treated hearts (IR/ILE) but occasional staining of intravasal blood cells (black arrows). Panel B) CD11R3 staining (magnification 10x) reveals similar amounts of mononuclear cells (leukocytes) predominantly in small vessels (black arrows) in control (IR) and ILE-treated hearts (IR/ILE) without accumulation of leukocytes within cardiac tissue. Porcine spleen served as a positive control. Panel C) The endothelial marker CD31 was equally expressed in control (IR) and ILE-treated hearts (IR/ILE) (magnification 10x). There is no visible accumulation of mononuclear cells within the vessels. Porcine spleen served as a positive control. Bar = 200 µm in all panels
Intralipid® postconditioning elicits signalling ROS at the onset of reperfusion, which is accompanied by phosphorylation of glycogen synthase kinase (GSK)3β in porcine DCD hearts
In an attempt to replicate our previous findings with regard to protection signalling in small rodent hearts exposed to IR and treated with ILE postconditioning,11,12 and to determine if these signalling events also occur in large mammalian hearts, we measured ROS formation in LV cardiac fibres collected five minutes after the initiation of reperfusion in control and ILE-treated porcine hearts and also determined concomitant phosphorylation of Akt and its downstream target GSK3β. Hydrogen peroxide emission rate was increased in ILE-treated hearts (P = 0.011) (Figs 4A and 4B). Akt showed a trend (P = 0.08) to increased phosphorylation by ILE postconditioning (Fig. 4C), and its downstream target GSK3β was clearly phosphorylated (Fig. 4C) (P = 0.037). Extracellular signal-regulated kinase (ERK)1/2 and signal transducer and activator of transcription 3 (STAT3) were not activated (not phosphorylated) at this time point (data not shown).
Early signalling events in left ventricular biopsies collected five minutes after the onset of reperfusion in control (IR) and ILE (Intralipid®) treated (IR/ILE) porcine hearts. Panel A) Hydrogen peroxide (H2O2) emission rate in non-energized (without added substrates) and energized (with added substrates) cardiac fibres as measured by Amplex Red assay. The connected dots track the H2O2 rates in fibres from individual experimental samples before and after energization with substrates. IR (five minutes/basal), non-energized cardiac fibres of control hearts exposed to IR collected after the onset of reperfusion; IR (five minutes /+ substrate), respective energized fibres; IR/ILE (5 min/basal), non-energized cardiac fibres of ILE-treated hearts exposed to IR collected at five minutes of reperfusion; IR (5 min/+substrate), respective energized fibres. Panel B) Summary of mitochondrial H2O2 emission rate (computed as the difference between the rates from energized and non-energized fibres from panel A between control (IR) and ILE-treated (IR/ILE) hearts at five minutes after reperfusion. Mean (SD) values are depicted next to dots representing individual measurements. Panel C) Immunoblots showing phosphorylation of Akt (pS473) and glycogen synthase kinase (GSK)3β (pS9) from total tissue lysates. First two lanes show two representative aerobic control hearts (AER-1, AER-2) not exposed to IR. Subsequent lanes show pairs of control and ILE-treated hearts (IR-1 and IR/ILE-1, IR-2 and IR/ILE-2, IR-3 and IR/ILE-3, IR-4 and IR/ILE-4, IR-5 and IR/ILE-5). Vinculin was used as a loading control. Mean (SD) values are depicted next to dots representing individual measurements. n = 5 per group
Intralipid® postconditioning elicits sustained Akt activation and further activates STAT3 in mitochondria during later stages of reperfusion in porcine DCD hearts
To determine whether protection signalling is maintained during ILE postconditioning, we also measured phosphorylation of Akt, ERK1/2, and STAT3 in LV total tissue and phosphorylation of STAT3 in mitochondrial fractions after 60 min of reperfusion. While P-Akt (total tissue, P = 0.044) and p-STAT3 (mitochondrial fraction, P = 0.033) were clearly increased in porcine hearts treated with ILE postconditioning, there was no increased activation of ERK1/2 (Fig. 5).
Late signalling events in left ventricular tissue collected after 60 min of reperfusion in control (IR) and ILE (Intralipid®) treated (IR/ILE) porcine hearts. Panel A) Immunoblots showing phosphorylation of Akt (pS473), extracellular signal-regulated kinase (ERK)1/2 (pT202/pY204), and signal transducer and activator of transcription 3 (STAT3) (pY705) from total tissue lysates. First two lanes show two representative aerobic control hearts (AER-1, AER-2) not exposed to IR. Subsequent lanes show pairs of control and ILE-treated hearts (IR-1 and IR/ILE-1, IR-2 and IR/ILE-2, IR-3 and IR/ILE-3, IR-4 and IR/ILE-4, IR-5 and IR/ILE-5). Panel B) Immunoblots showing phosphorylation of STAT3 (pY705) from mitochondrial fractions. Lanes show pairs of control and ILE-treated hearts (IR-1 and IR/ILE-1, IR-2 and IR/ILE-2, IR-3 and IR/ILE-3, IR-4 and IR/ILE-4, IR-5 and IR/ILE-5). Vinculin (for total tissue lysates in panel A) and voltage-dependent anion-selective channel 1 (VDAC, for mitochondrial fractions in panel B) were used as loading controls. Mean (SD) values are depicted next to dots representing individual measurements. n = 5 per group
Discussion
We investigated the cardioprotective potential of ILE postconditioning as a novel pharmacologic therapy to enhance protection against IR injury in porcine DCD hearts. Although our study shows only a modest post-ischemic functional improvement in the primary endpoint (dP/dtmax) of hearts treated with ILE postconditioning, the additional protection we observed in biochemical analyses with ILE postconditioning is remarkable since hearts were procured using a previously optimized protocol with warm cardioplegia containing lidocaine and adenosine to protect against IR injury.6,7 Moreover, the hearts were exposed to isoflurane, a protective inhalational anesthetic,22 as part of the experimental background anesthetic, while avoiding propofol, an anesthetic that inhibits ILE postconditioning.23 We have recently shown in rat hearts that inhalational anesthetics together with ILE postconditioning provide additive protection,23 and we have now confirmed this observation in a large mammal (porcine) model. Our study further provides evidence to suggest that ILE postconditioning confers protection to these hearts by eliciting the same cell signalling pathways previously reported in small rodent hearts, involving the upstream release of signalling ROS at the onset of reperfusion and downstream inhibition of GSK3β.9,10,11,12
In the DCD transplant context, the donor heart suffers from damage due to: 1) prolonged warm ischemia during the period of donor decompensation, death, and procurement mimicked in our model by the withdrawal of mechanical ventilation (with consecutive asphyxiation) and the standoff period after declaration of circulatory death, and 2) subsequent ex vivo reperfusion with oxygenated Ca2+-containing perfusate. We observed less glutathione leakage from the myocardium in protected ILE postconditioned hearts. This low molecular weight peptide (308 Dalton) is a sensitive marker of cell damage in IR injury, which is particularly suited to measure membrane damage as previously shown in preconditioning experiments.24 Moreover, hearts treated with ILE postconditioning contained less oxidized carbonylated proteins. Carbonylation represents an irreversible form of protein modification due to oxidation with a clearance rate of days as opposed to lipid peroxidation products, which are removed within minutes.
In our study, we observed only a small improvement in cardiac function in ILE-treated hearts. Nevertheless, this may be because heart procurement was optimized to ensure cellular protection from IR injury.6,7 Also, the hearts were only reperfused for 60 min and longer periods of reperfusion may be needed to clearly reveal more pronounced differences in functional recovery between protected and unprotected hearts.7 In our previous studies with rat hearts, we showed that ILE improved recovery of post-ischemic mechanical function by mechanisms independent of a direct metabolic (“cardiotonic”) effect, i.e., by the provision of supplemental energy substrates such as fatty acids.12 Instead, protection is the result of early ROS-mediated activation of protection signalling, consistent with the concept of postconditioning.11,12 Accordingly, ILE during reperfusion is only required for the first few minutes at the onset of reperfusion to trigger protection. A direct positive inotropic effect of ILE has been reported in recent studies using guinea pig papillary muscles25 and in vivo rat experiments,26 but these effects were transient and short-lived, and occurred mainly at ILE concentrations of 2.8% and higher. Interestingly, these changes in inotropy are, again, not the result of metabolic or “cardiotonic” effects as they are not affected by oxfenicine, an inhibitor of carnitine palmitoyltransferase I. It is possible that the same signalling events that also trigger cardioprotection, such as Akt activation, interfere with Ca2+ handling27 and thus increase contractility, contributing at least in part to the improved mechanical function in ILE postconditioned hearts.
Our previous data from rat hearts suggest that Akt and ERK1/2, but not STAT3, are activated at early reperfusion, and that STAT3 is phosphorylated only at later stages of reperfusion,12 possibly transactivated by Akt.28 Our current data from porcine hearts show no activation of ERK1/2 and STAT3 at early reperfusion in LV biopsies, while Akt showed a trend to activation, and GSK3β, its downstream target, was phosphorylated, indicative of inhibition. GSK3β plays a key role in the convergence of protection signalling to inhibit or delay mitochondrial permeability transition.29 We speculate that the non-significant Akt phosphorylation is likely due to the timing of sample collection; thus, Akt may be still an important trigger kinase in ILE-induced postconditioning in the porcine heart.30 A mechanistic role of STAT3 in ILE cardioprotection is also possible since STAT3 signalling was proposed as the main protection pathway in a porcine model using ischemic (but not pharmacologic) postconditioning.31 Our data suggest that STAT3 may have an important mediator role at later stages of reperfusion since we found increased STAT3 phosphorylation in LV mitochondria 60 min after reperfusion. A small pool of STAT3 resides in mitochondria and has been linked to the control of the electron transport chain, modulation of ROS generation, and the regulation of the mitochondrial permeability transition pore.32 Regardless of the exact mechanism involved, our experiments clearly show protection signalling and indicate reduced ischemic damage in ILE-treated porcine hearts. This confirms the effectiveness of this cardioprotective strategy, even in the presence of other cardioprotective agents (lidocaine, adenosine, isoflurane) and using previously optimized reperfusion conditions.5,6,7
Our analyses also show that ILE postconditioning markedly attenuates MPO activation during IR. Myeloperoxidase, predominantly stored in the azurophilic granules of leukocytes, is a key inflammatory mediator responsible for endothelial dysfunction, apoptosis, and plaque vulnerability.20 Upon leukocyte activation, MPO is released into the tissue and forms the toxic hypochlorous acid.33 Myeloperoxidase is a major risk factor for coronary artery disease, but also enhances cardiomyocyte damage during IR. Not surprisingly, individuals expressing reduced MPO are protected against coronary artery disease and myocardial infarction,34,35 and MPO knockout mice exhibit reduced leukocyte infiltration and LV dilation and remodeling after permanent coronary artery ligation.36 Interestingly, a recent study also showed positive MPO immunostaining not only in the vascular and perivascular space, but also inside cardiomyocytes.37 This is consistent with findings from our study, namely the lack of leukocyte accumulation in early reperfused cardiac tissue as measured by MPO content and immunohistochemistry. Intracardiomyocyte MPO activity exhibits strong positive correction with caspase-3 activity and its inhibition reduces myocardial infarct size.37 It is likely that the increased baseline H2O2 production, as measured by Amplex Red assay in non-energized control cardiac fibres at early reperfusion, may reflect increased activation of prooxidant intracardiomyocyte enzymes, including MPO.
Limitations and future research
We have used only female pigs to enable direct comparison to our previous studies. Because the animals were sexually immature, sex hormone effects on ILE cardioprotection were considered negligible. Nevertheless, cellular and functional differences between male and female porcine hearts may exist. Even in the most recent practice guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection, it appears unclear “whether sex influences the effect of cardioprotection in larger mammals”.38 We have used dP/dtmax as a primary outcome of post-ischemic functional recovery, but other parameters such as ejection fraction may have been more reliable, specifically when limiting the post-ischemic perfusion time. Glutathione tissue content rather than troponin release into the perfusate was thought to be more reliable in reflecting myocardial injury in the presence of transmural biopsies. Since the purpose of this study was to test: 1) whether ILE postconditioning is capable of protecting DCD hearts, and 2) whether protection signalling is similar in large and small animal hearts, we did not use ROS blockers to prove causal involvement of ROS in the ILE postconditioning as we did in our previous studies.11,12 Donation after circulatory death hearts were exposed to isoflurane prior to and during asphyxiation, which induces preconditioning and may present an unrealistic condition, which may not be found in a clinical scenario. Nonetheless, although potential organ donors in the DCD context may only occasionally be exposed to isoflurane shortly before death and cardiac arrest, many patients are treated with preconditioning-inducing drugs such as morphine, statins, and potentially others that exert pharmacologic conditioning similar to isoflurane. Future research within the realm of newly available guidelines for translational research39 should explore the possible role of other protection mechanisms involved in ILE postconditioning. This will help to address the biologic and more so the clinical significance of these findings.
In summary, we show that DCD hearts can be protected by Intralipid® administered at the onset of reperfusion. Intralipid® postconditioning increased inotropy, reduced cell membrane damage, protected LV tissue from protein carbonylation, and decreased myeloperoxidase activity in reperfused hearts. The present results from porcine hearts are highly encouraging and confirm previous results from small rodent hearts. Our findings support the use of ILE postconditioning in DCD human heart procurement.
References
Rao V, Dhanani S, MacLean J, et al. Effect of organ donation after circulatory determination of death on number of organ transplants from donors with neurologic determination of death. CMAJ 2017; 189: E1206-11.
Dhital KK, Iyer A, Connellan M, et al. Adult heart transplantation with distant procurement and ex-vivo preservation of donor hearts after circulatory death: a case series. Lancet 2015; 385: 2585-91.
Hausenloy DJ, Yellon DM. Myocardial ischemia-reperfusion injury: a neglected therapeutic target. J Clin Invest 2013; 123: 92-100.
White CW, Messer SJ, Large SR, et al. Transplantation of hearts donated after circulatory death. Front Cardiovasc Med 2018; 5: 8.
White CW, Ambrose E, Muller A, et al. Assessment of donor heart viability during ex vivo heart perfusion. Can J Physiol Pharmacol 2015; 93: 893-901.
White C, Ambrose E, Muller A, et al. Impact of reperfusion calcium and pH on the resuscitation of hearts donated after circulatory death. Ann Thorac Surg 2017; 103: 122-30.
White CW, Ambrose E, Muller A, et al. Avoidance of profound hypothermia during initial reperfusion improves the functional recovery of hearts donated after circulatory death. Am J Transplant 2016; 16: 773-82.
Iyer A, Gao L, Doyle A, et al. Increasing the tolerance of DCD hearts to warm ischemia by pharmacological postconditioning. Am J Transplant 2014; 14: 1744-52.
Rahman S, Li J, Bopassa JC, et al. Phosphorylation of GSK-3beta mediates intralipid-induced cardioprotection against ischemia/reperfusion injury. Anesthesiology 2011; 115: 242-53.
Li J, Iorga A, Sharma S, et al. Intralipid, a clinically safe compound, protects the heart against ischemia-reperfusion injury more efficiently than cyclosporine-A. Anesthesiology 2012; 117: 836-46.
Lou PH, Lucchinetti E, Zhang L, et al. The mechanism of Intralipid(R)-mediated cardioprotection complex IV inhibition by the active metabolite, palmitoylcarnitine, generates reactive oxygen species and activates reperfusion injury salvage kinases. PLoS One 2014; 9: e87205.
Zaugg M, Lou PH, Lucchinetti E, Gandhi M, Clanachan AS. Postconditioning with Intralipid emulsion protects against reperfusion injury in post-infarct remodeled rat hearts by activation of ROS-Akt/Erk signaling. Transl Res 2017; 186(36-51): e2.
Brand MD. Mitochondrial generation of superoxide and hydrogen peroxide as the source of mitochondrial redox signaling. Free Radic Biol Med 2016; 100: 14-31.
Brennan JP, Southworth R, Medina RA, Davidson SM, Duchen MR, Shattock MJ. Mitochondrial uncoupling, with low concentration FCCP, induces ROS-dependent cardioprotection independent of KATP channel activation. Cardiovasc Res 2006; 72: 313-21.
Chen W, Gabel S, Steenbergen C, Murphy E. A redox-based mechanism for cardioprotection induced by ischemic preconditioning in perfused rat heart. Circ Res 1995; 77: 424-9.
Hamanaka RB, Chandel NS. Mitochondrial reactive oxygen species regulate cellular signaling and dictate biological outcomes. Trends Biochem Sci 2010; 35: 505-13.
Vanden Hoek TL, Becker LB, Shao Z, Li C, Schumacker PT. Reactive oxygen species released from mitochondria during brief hypoxia induce preconditioning in cardiomyocytes. J Biol Chem 1998; 273: 18092-8.
Kilgore KS, Lucchesi BR. Reperfusion injury after myocardial infarction: the role of free radicals and the inflammatory response. Clin Biochem 1993; 26: 359-70.
Cox B, Emili A. Tissue subcellular fractionation and protein extraction for use in mass-spectrometry-based proteomics. Nat Protoc 2006; 1: 1872-8.
Nicholls SJ, Hazen SL. Myeloperoxidase and cardiovascular disease. Arterioscler Thromb Vasc Biol 2005; 25: 1102-11.
Wang XS, Kim HB, Szuchman-Sapir A, McMahon A, Dennis JM, Witting PK. Neutrophils recruited to the myocardium after acute experimental myocardial infarct generate hypochlorous acid that oxidizes cardiac myoglobin. Arch Biochem Biophys 2016; 612: 103-14.
Zaugg M, Lucchinetti E, Spahn DR, Pasch T, Schaub MC. Volatile anesthetics mimic cardiac preconditioning by priming the activation of mitochondrial K(ATP) channels via multiple signaling pathways. Anesthesiology 2002; 97: 4-14.
Lucchinetti E, Lou PH, Gandhi M, Clanachan AS, Zaugg M. Differential effects of anesthetics and opioid receptor activation on cardioprotection elicited by reactive oxygen species-mediated postconditioning in Sprague-Dawley rat hearts. Anesth Analg 2018; 126: 1739-46.
Verbunt RJ, Van der Laarse A. Glutathione metabolism in non-ischemic and postischemic rat hearts in response to an exogenous prooxidant. Mol Cell Biochem 1997; 167: 127-34.
Park WK, Kim HS, Kim SH, Jung JR, Lynch C 3rd, Min NH. Intralipid restoration of myocardial contractions following bupivacaine-induced asystole: concentration- and time-dependence in vitro. Anesth Analg 2017; 125: 91-100.
Fettiplace MR, Ripper R, Lis K, et al. Rapid cardiotonic effects of lipid emulsion infusion. Crit Care Med 2013; 41: e156-62.
Song G, Ouyang G, Bao S. The activation of Akt/PKB signaling pathway and cell survival. J Cell Mol Med 2005; 9: 59-71.
Zhang X, Shan P, Alam J, Fu XY, Lee PJ. Carbon monoxide differentially modulates STAT1 and STAT3 and inhibits apoptosis via a phosphatidylinositol 3-kinase/Akt and p38 kinase-dependent STAT3 pathway during anoxia-reoxygenation injury. J Clin Invest 2005; 280: 8714-21.
Juhaszova M, Zorov DB, Kim SH, et al. Glycogen synthase kinase-3beta mediates convergence of protection signaling to inhibit the mitochondrial permeability transition pore. J Clin Invest 2004; 113: 1535-49.
Hausenloy DJ, Yellon DM. Reperfusion injury salvage kinase signalling: taking a RISK for cardioprotection. Heart Fail Rev 2007; 12: 217-34.
Heusch G, Musiolik J, Gedik N, Skyschally A. Mitochondrial STAT3 activation and cardioprotection by ischemic postconditioning in pigs with regional myocardial ischemia/reperfusion. Circ Res 2011; 109: 1302-8.
Szczepanek K, Chen Q, Larner AC, Lesnefsky EJ. Cytoprotection by the modulation of mitochondrial electron transport chain: the emerging role of mitochondrial STAT3. Mitochondrion 2012; 12: 180-9.
Podrez EA, Abu-Soud HM, Hazen SL. Myeloperoxidase-generated oxidants and atherosclerosis. Free Radic Biol Med 2000; 28: 1717-25.
Asselbergs FW, Tervaert JW, Tio RA. Prognostic value of myeloperoxidase in patients with chest pain. N Engl J Med 2004; 350: 516-8.
Nikpoor B, Turecki G, Fournier C, Theroux P, Rouleau GA. A functional myeloperoxidase polymorphic variant is associated with coronary artery disease in French-Canadians. Am Heart J 2001; 142: 336-9.
Askari AT, Brennan ML, Zhou X, et al. Myeloperoxidase and plasminogen activator inhibitor 1 play a central role in ventricular remodeling after myocardial infarction. J Exp Med 2003; 197: 615-24.
Liu HR, Tao L, Gao E, et al. Rosiglitazone inhibits hypercholesterolaemia-induced myeloperoxidase upregulation–a novel mechanism for the cardioprotective effects of PPAR agonists. Cardiovasc Res 2009; 81: 344-52.
Botker HE, Hausenloy D, Andreadou I, et al. Practical guidelines for rigor and reproducibility in preclinical and clinical studies on cardioprotection. Basic Res Cardiol 2018; 113: 39.
Hausenloy DJ, Garcia-Dorado D, Botker HE, et al. Novel targets and future strategies for acute cardioprotection: position paper of the European Society of Cardiology Working Group on Cellular Biology of the Heart. Cardiovasc Res 2017; 113: 564-85.
Acknowledgements
We would like to thank Dr. Gregory Korbutt, Scientific Director of the Alberta Cell Therapy Manufacturing Facility and Director of the Alberta Diabetes Institute Histology Core for performing the immunohistochemistry. This study was supported by grants from the University Hospital Foundation, University of Alberta Hospital (Edmonton, Canada), the Heart and Stroke Foundation of Canada, and the Canadian National Transplant Research Program.
Conflicts of interest
None declared.
Editorial responsibility
This submission was handled by Dr. Hilary P. Grocott, Editor-in-Chief, Canadian Journal of Anesthesia.
Author contributions
Eliana Lucchinetti contributed substantially to all aspects of this manuscript, including study design, data acquisition, analysis and interpretation, and drafting the article. Phing-How Lou contributed substantially to data acquisition and analysis as well as drafting the article. Sanaz Hatami and Xiao Qi assisted with the surgeries and supervised the ex vivo perfusions including functional data acquisition. Alexander S. Clanachan contributed to data interpretation and to critical revision of the manuscript. Darren H. Freed performed all surgeries, supervised the ex vivo perfusions, and contributed to manuscript drafting. Michael Zaugg contributed substantially to all aspects of this manuscript, including study design, data analysis and interpretation, and manuscript drafting.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lucchinetti, E., Lou, PH., Hatami, S. et al. Enhanced myocardial protection in cardiac donation after circulatory death using Intralipid® postconditioning in a porcine model. Can J Anesth/J Can Anesth 66, 672–685 (2019). https://doi.org/10.1007/s12630-019-01322-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-019-01322-x