Abstract
Introduction
The purpose of this survey was to determine the equipment that anesthesiologists prefer in difficult tracheal intubation and “cannot intubate, cannot ventilate” (CICV) situations.
Methods
A questionnaire was e-mailed to members of the Canadian Anesthesiologists’ Society to ascertain their preferences, experience, and comfort level with regard to their use of airway equipment in difficult intubation and CICV situations in adult patients. A Chi square test was used to analyse the data. All reported P values are two-sided.
Results
Nine hundred ninety-seven of 2,532 questionnaires (39%) were returned. In an unanticipated difficult direct laryngoscopic intubation situation, 893 of 997 (90%) respondents chose a video laryngoscope as the first-choice rescue technique, while 41 (4%) and 21 (2%) of respondents chose a flexible bronchoscope and an intubating laryngeal mask airway device, respectively. The majority of anesthesiologists had experience and were comfortable with using a flexible bronchoscope or a video laryngoscope. Regarding CICV, 294 of 955 (31%) respondents stated that they had never encountered it. Wire-guided cricothyroidotomy was chosen as the first-choice surgical airway by 375 of 955 (39%) respondents, while intravenous catheter cricothyroidotomy and “defer to tracheostomy by surgeon” were selected by 266 (28%) and 215 (23%) respondents, respectively. Seven hundred eighty-five of 997 (78%) respondents were familiar with the exact steps of the American Society of Anesthesiologists’ difficult airway algorithm, while 448 (47%) had attended an airway workshop within the past five years.
Conclusions
In a difficult intubation situation, the most frequently selected first-choice airway device was a video laryngoscope, followed by a flexible bronchoscope. In a CICV situation, the most frequently selected first-choice surgical airway technique was a wire-guided cricothyroidotomy, followed by an intravenous catheter cricothyroidotomy.
Résumé
Introduction
L’objectif de cette enquête était de déterminer quel équipement les anesthésiologistes préfèrent en cas d’intubation trachéale difficile et dans les situations « impossible d’intuber, impossible de ventiler » (IIIV).
Méthodes
Un questionnaire a été adressé par courriel au membre de la Société canadienne des anesthésiologistes pour connaître leurs préférences, leur expérience et leur niveau de confort concernant l’utilisation du matériel d’intubation dans les cas d’intubation difficile et dans les situations IIIV chez des patients adultes. Un test du Chi2 a été utilisé pour analyser les données. Toutes les valeurs de P fournies sont bilatérales.
Résultats
Neuf cent quatre-vingt-dix-sept questionnaires ont été retournés sur 2 532 (39 %). Confrontés à une situation inattendue d’intubation laryngoscopique directe difficile, 893 des 997 (90 %) répondants ont choisi un vidéolaryngoscope comme premier choix de technique de secours, tandis que 41 (4 %) et 21 (2 %) des répondants ont préféré un bronchoscope flexible et un dispositif de masque laryngé d’intubation, respectivement. La majorité des anesthésiologistes avaient l’expérience des bronchoscopes flexibles et d’un vidéolaryngoscope et se sentaient à l’aise pour les utiliser. Concernant les situations IIIV, 294 des 955 répondants (31 %) ont indiqué qu’ils n’en avaient jamais rencontré. La cricothyroïdotomie sur guide d’acier a été retenue comme premier choix chirurgical d’ouverture des voies aériennes par 375 des 955 répondants (39 %), tandis que la cricothyroïdotomie avec cathéter intraveineux et le « transfert au chirurgien pour trachéotomie » ont été choisis par, respectivement, 266 (28 %) et 215 (23 %) des répondants. Sept cent quatre-vingt-cinq répondant sur 997 (78 %) connaissaient les étapes exactes de l’algorithme pour intubation difficile de l’American Society of Anesthesiologists tandis que 448 répondants (47 %) avaient assisté à un atelier sur les voies aériennes au cours des cinq dernières années.
Conclusions
Dans les situations d’intubation difficile, le premier choix de dispositif, le plus souvent sélectionné, et un vidéolaryngoscope, suivi par le bronchoscope flexible. Devant une situation IIIV, la technique chirurgicale de premier choix la plus souvent sélectionnée est la cricothyroïdotomie sur guide d’acier, suivie par la cricothyroïdotomie par cathéter intraveineux.
Similar content being viewed by others
Since the last Canadian anesthesiologists’ survey1 on “cannot intubate, cannot ventilate” (CICV) situations conducted in 2003 and published in 2005, there have been many advances in equipment available to anesthesiologists, including video laryngoscopes (e.g., GlideScope® 2 and C-MAC®) and optical stylets for difficult intubations. Nevertheless, since video laryngoscopy became available, there are limited data available on equipment preferences in an unanticipated difficult intubation scenario.
“Cannot intubate, cannot ventilate” is defined as a situation wherein tracheal intubation fails and oxygenation by bag-mask or supraglottic airway ventilation is unsuccessful.3 The American Society of Anesthesiologists (ASA) and the Difficult Airway Society have provided guidelines4,5 on management of this situation in which performing an infraglottic surgical airway is considered the last resort. As CICV situations are infrequent, many anesthesiologists are unfamiliar with how to perform a “surgical” airway6 in either patients or mannequins.
Many different methods can be used to perform a “surgical” airway, including a narrow-bore intravenous catheter cricothyroidotomy, a wire-guided cricothyroidotomy, and the conventional open surgical technique.7 In an earlier Canadian survey,1 the majority of anesthesiologists chose a narrow-bore catheter cricothyroidotomy as their first-choice surgical airway in a CICV situation. Despite this, evidence shows that a narrow-bore catheter cricothyroidotomy has a poor success rate and is associated with numerous complications.8,9
Given these new advances in equipment and evidence of the efficacy of surgical airway9 in the last decade, we planned to re-distribute the 2003 airway questionnaire, with some modifications, to current members of the Canadian Anesthesiologists’ Society. The purpose of this survey was to determine anesthesiologists’ current preferences, experience, and comfort level using airway equipment in unanticipated difficult intubation and CICV situations.
Methods
The University Health Network Research Ethics Board approved the online questionnaire (Appendix, REB #12-5486-BE, approved Jan 13, 2013) powered by SurveyMonkey® (www.surveymonkey.com/).
Following approval by the Canadian Anesthesiologists’ Society (CAS), a cover e-mail containing a link to the questionnaire was sent to members of the CAS during February 2013. Two reminder e-mails were sent at approximately three-week intervals to those who had not completed the questionnaire. Exclusion criteria were non-anesthesiologists and inactive CAS members. It stated in the e-mail that completion of the Web-based questionnaire indicated consent to participate in the research study.
The following modifications were made to the 2003 questionnaire: flexible bronchoscope was used instead of fibreoptic bronchoscope, lighted stylet was removed as a choice for intubating equipment, and scalpel-bougie was added as a choice for cricothyroidotomy. The questionnaire used in the current study consists of three general sections (Appendix). The first section describes an unanticipated difficult intubation and failed direct laryngoscopy situation and poses three questions. First, recipients are asked to select their first and second choices for alternative airway devices to manage the situation. Second, they are asked whether they have used any of the listed devices on mannequins or patients. Third, they are asked to indicate on a four-point Likert scale their level of comfort in using the selected alternative intubating equipment and retrograde intubation.
The second section pertains to a CICV situation. Recipients are asked how many times they encountered a CICV situation in the last five years, or ever, and in what circumstances they encountered the situations. Recipients of the questionnaire are given a CICV situation and asked three questions. They are asked their first and second choices of “surgical” airway, if they had personally used any of the specified devices, and their comfort level in using them.
In the last section, recipients are asked if they are familiar with the exact steps of the ASA 2003 difficult airway algorithm and the Difficult Airway Society 2004 algorithm and if they had personally attended a difficult airway workshop in the last five years. Finally, demographic questions include age group, sex, years in practice, type of hospital, and province of practice.
Statistical analyses were performed using SPSS® 15.0 (SPSS Inc. Chicago, IL, USA). For statistical analyses, comfort level with the use of alternative airway devices and with performing a surgical airway were categorized into binary variables. “Very comfortable” and “somewhat comfortable” were collapsed into “comfortable”, while “somewhat uncomfortable” and “not consider using” were collapsed into “uncomfortable”. A Chi square test was used to compare categorical variables. All reported P values are two-sided.
Results
There were 2,532 survey invitations e-mailed, and 997 (39%) members responded by filling out the Web-based questionnaire. The cumulative numbers of respondents at initial request and after the first and second reminders were 394, 512, and 997 respondents, respectively. Of those who responded, 955 answered all questions completely, and 42 did not provide complete answers. Blank responses to questions were coded as missing data. Demographic data, including age range, sex, practice status, type of hospital, and location of practice are summarized in Table 1.
For the difficult intubation situation (Table 2), a video laryngoscope was the first-choice alternative technique chosen by 893 of 997 (90%) respondents in an unanticipated difficult direct laryngoscopic intubation situation, while a flexible bronchoscope was chosen by 41 (4%) respondents, intubating laryngeal mask airway by 21 (2%) respondents, and optical stylet by 17 (2%) respondents. In the 2003 survey,1 lighted stylet was the alternative technique chosen by 432 of 971 respondents (45%), flexible bronchoscope by 251 (26%) respondents, and intubating laryngeal mask airway by 197 (20%) respondents.
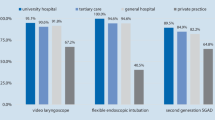
Virtually all anesthesiologists (Table 3) had performed awake flexible bronchoscopic intubation (98%) and asleep flexible bronchoscopic intubation (91%) and used video laryngoscopes (99%). A lesser percentage had used an intubating laryngeal mask airway (80%) and the retrograde wire technique (14%) in patients. Most anesthesiologists were comfortable with using the flexible bronchoscope and the video laryngoscope, while less than 50% were comfortable with the optical stylet and retrograde wire technique (Table 3).
Thirty-one percent of respondents stated that they had not encountered CICV. Fifty-two percent of the respondents had encountered a CICV situation either once or twice, and 17% had encountered a CICV situation at least three times. A CICV situation was encountered mostly in elective surgery (49%), followed by emergency surgery (38%).
In a CICV situation (Table 4), a wire-guided cricothyroidotomy was chosen as the first-choice surgical airway by 375 of 955 (39%) respondents, while an intravenous catheter cricothyroidotomy and “defer to tracheostomy by surgeon” were selected by 266 (28%) and 215 (23%) respondents, respectively. In the 2003 survey,1 an intravenous catheter cricothyroidotomy was the surgical airway chosen by 490 of 971 (51%) respondents, wire-guided cricothyroidotomy by 276 (28%) respondents, and “defer to tracheostomy by surgeon” by 136 (14%) respondents. The use of surgical airways on mannequins and patients and the proportion of respondents comfortable in using surgical airways are shown in Table 5. A wire-guided cricothyroidotomy had been performed on mannequins and on patients by approximately 70% and 12% of respondents, respectively. A cricothyroidotomy via intravenous catheter had been performed on mannequins and on patients by 61% and 13% of respondents, respectively. Most respondents were not comfortable performing an open surgical cricothyroidotomy, scalpel-bougie cricothyroidotomy, or tracheostomy.
Seventy-eight percent of anesthesiologists were familiar with the 2003 ASA difficult airway guidelines, while 66% were familiar with the 2004 Difficult Airway Society guidelines. Approximately half of the respondents had attended a difficult airway workshop within the last five years.
Discussion
Difficult intubation
Through this survey, we found that the majority of respondents preferred to use a video laryngoscope followed by a flexible bronchoscope in an unanticipated difficult intubation situation with failed direct laryngoscopy (Table 2). These results differ from an earlier Canadian survey1 in which a lighted stylet and flexible bronchoscope were the preferred choices. In our view, this reflects a major shift in anesthesiologists’ preferences for airway equipment. The use of “older” equipment, e.g., lighted stylet and the retrograde wire set,10 in difficult intubation situations has been replaced with newer devices such as video laryngoscopes. Previous studies from 1998-200411-13 showed that the flexible bronchoscope and intubating laryngeal mask airway were the most popular devices selected when encountering a difficult intubation. Since then, however, technology has advanced notably with the introduction of video laryngoscopes. There are numerous articles showing improved laryngoscopic views and success14 with video laryngoscopes, and this may account for the increasing use seen10 in difficult intubation situations. The Trachlight™, the most commonly used type of lighted stylet, is no longer produced commercially and was not offered as a choice in this survey.
Most respondents stated that they were experienced with flexible bronchoscopes (91-98%). Ezri et al.13 and Rosenblatt et al.12 showed that 59% and 78% of respondents, respectively, were familiar with flexible bronchoscopes. Our results show an increase in familiarity compared with these two studies. Probable reasons for this positive change may include an increase in airway training during North American anesthesia residency10 and an increase in simulator and mannequin training.10 Our study shows that 34% of respondents have performed flexible bronchoscopy on mannequins (Table 3), similar to the findings of Ezri et al.13 and Goldmann et al.15 Over 90% of anesthesiologists have used video laryngoscopes and flexible bronchoscopes in patients. Most have not used optical stylets or the retrograde wire set on patients, with only 40% and 14% reported usage, respectively. This is considerably less than in the older studies13,15 in which 25-40% of respondents reported use of the retrograde wire. We can infer that most anesthesiologists experience success using video laryngoscopes and flexible bronchoscopes; therefore, alternative techniques are being taught8 and resorted to less frequently. Choices of particular equipment will also depend on the experience of the anesthesiologist11 and availability of the equipment in a particular department.
There is little information in the literature pertaining to comfort in using various difficult airway devices. Our survey results show that most respondents appear comfortable using flexible bronchoscopes and video laryngoscopes (Table 3) and less so in using older techniques such as the retrograde wire set. This corresponds with the low usage of these older techniques, both on mannequins and patients.
Cannot intubate cannot ventilate
The current survey shows that 69% of respondents had encountered CICV, 52% either once or twice and 17% at least three times. In 2005, Wong et al. 1 found that 57% had encountered CICV.
When encountering a CICV situation, there is also limited literature pertaining to choice of surgical airway. Various guidelines emphasize the insertion of a supraglottic airway and administration of muscle relaxant3 in a CICV situation prior to performing a surgical airway. The intent of the survey was not to query the clinical management of CICV but to assess the preferred cricothyroidotomy technique. We show (Table 4) that respondents chose wide-bore wire-guided cricothyroidotomy (39%) and narrow-bore intravenous catheter cricothyroidotomy (28%). A quarter of respondents would still defer to the surgeon rather than undertake a surgical airway themselves. In 2005, Wong et al. 1 showed that the first-choice surgical airway in a CICV situation was cricothyroidotomy via intravenous catheter (51%), and the second choice was wire-guided cricothyroidotomy (28%). The National Audit Project 49 highlighted problems and a high failure rate while using a narrow-bore or wide-bore percutaneous cricothyroidotomy and recommended the open surgical cricothyroidotomy in a CICV situation. We showed a trend away from the once popular1 intravenous catheter cricothyroidotomy; however, only 8% of respondents chose the open surgical method. The “scalpel-bougie” technique as mentioned by Heard et al.7 and widely taught in Australia is rarely chosen in our survey (3% first choice); however, it remains a feasible option when encountering a CICV situation.
Only 10-13% of our respondents have performed a wire-guided cricothyroidotomy, intravenous catheter cricothyroidotomy, or tracheostomy on patients in a CICV situation. Only 5% have performed the scalpel-bougie method, and only 2% have performed the open surgical method. The rare performance on patients is consistent with literature findings,16 i.e., a lower frequency of CICV situations in recent years,17 and 80% of respondents in our survey had less than two CICV encounters in their practice. We show that approximately 60-70% of respondents have performed a cricothyroidotomy on a mannequin. Wire-guided cricothyroidotomy was the most commonly used technique. The high failure rate of cricothyroidotomy in the National Audit Project 4 and a suboptimal exposure to mannequin training based on this survey suggest that additional exposure to surgical airway should be implemented through residency training and continuing medical education.
Fifty-two percent of respondents in our survey feel comfortable with wire-guided cricothyroidotomy, 43% with intravenous catheter cricothyroidotomy, and much fewer with the scalpel-bougie and open surgical methods. Given the increase in the use of mannequins and simulators in anesthesia training10,18 and improved performance and comfort levels19 with cricothyroidotomy through repetition using these methods, increased simulator training in surgical airway techniques may improve the comfort level of anesthesiologists in performing a surgical airway in a future CICV encounter.
Limitations of the survey include the approximate 40% response rate despite repeated reminders. This response rate is similar to that of two previous surveys.1,13 Second, a French version of the questionnaire was not available, potentially limiting our response rate in certain provinces, e.g., Quebec. Third, the questionnaire was distributed only via e-mail and not hard copy. The above limitations can lead to selection biases and limit the implications of our results.
In conclusion, our survey shows that a video laryngoscope is preferred in a difficult intubation situation; flexible bronchoscopy is the second choice, while the intubating laryngeal mask airway and optical stylet are rarely chosen. In a CICV situation, wire-guided cricothyroidotomy is the preferred method for a surgical airway, with intravenous catheter cricothyroidotomy being the second choice. Simulation training in surgical airway may be important in addressing a lack of comfort and clinical experience with this technique.
References
Wong DT, Lai K, Chung FF, Ho RY. Cannot intubate–cannot ventilate and difficult intubation strategies: results of a Canadian national survey. Anesth Analg 2005; 100: 1439-46.
Cooper RM, Pacey JA, Bishop MJ, McCluskey SA. Early clinical experience with a new videolaryngoscope (GlideScope) in 728 patients. Can J Anesth 2005; 52: 191-8.
Law JA, Broemling N, Cooper RM, et al. The difficult airway with recommendations for management – Part 1 – Difficult tracheal intubation encountered in an unconscious/induced patient. Can J Anesth 2013; 60: 1089-118.
Apfelbaum JL, Hagberg CA, Caplan RA, et al. Practice guidelines for the management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology 2013; 118: 251-70.
Henderson JJ, Popat MT, Latto IP, Pearce AC, Difficult Airway Society. Difficult Airway Society guidelines for management of the unanticipated difficult intubation. Anaesthesia 2004; 59: 675-94.
Eisenburger P, Laczika K, List M, et al. Comparison of conventional surgical versus Seldinger technique emergency cricothyroidotomy performance by inexperienced clinicians. Anesthesiology 2000; 92: 687-90.
Heard AM, Green RJ, Eakins P. The Formulation and introduction of a ‘can’t intubate, can’t ventilate’ algorithm into clinical practice. Anaesthesia 2009; 64: 601-8.
Green L. Can’t intubate, can’t ventilate! A survey of knowledge and skills in a large teaching hospital. Eur J Anaesthesiol 2009; 26: 480-3.
Cook TM, Woodall N, Frerk C, Fourth National Audit Project. Major complications of airway management in the UK: results of the Fourth National Audit Project of Royal College of Anaesthetists and the Difficult Airway Society. Part 1: anaesthesia. Br J Anaesth 2011; 106: 617-31.
Pott LM, Randel GI, Straker T, Becker KD, Cooper RM. A survey of airway training among U.S. and Canadian Anesthesiology residency programs. J Clin Anesth 2011; 23: 15-26.
Bokhari A, Benham SW, Popat MT. Management of unanticipated difficult intubation: a survey of current practice in the Oxford region. Eur J Anaesthesiol 2004; 2: 123-7.
Rosenblatt WH, Wagner PJ, Ovassapian A, Kain ZN. Practice patterns in managing the difficult airway by anesthesiologists in the United States. Anesth Analg 1998; 87: 153-7.
Ezri T, Szmuk P, Warters RD, Katz J, Hagberg CA. Difficult airway management practice patterns among anesthesiologists practicing in the United States: have we made any progress? J Clin Anesth 2003; 15: 418-22.
Aziz MF, Dillman D, Fu R, Brambrink AM. Comparative effectiveness of the C-MAC video laryngoscope versus direct laryngoscopy in the setting of the predicted difficult airway. Anesthesiology 2012; 116: 629-36.
Goldmann K, Braun U. Airway management practices at German university and university-affiliated teaching hospitals – equipment, techniques and training: results of a nationwide survey. Acta Anaesthesiol Scand 2006; 50: 298-305.
McNarry AF, Dovell T, Dancey FM, Pead ME. Perception of training needs and opportunities in advanced airway skills: a survey of British and Irish trainees. Eur J Anaesthesiol 2007; 24: 498-504.
Hamaekers AE, Henderson JJ. Equipment and strategies for emergency tracheal access in the adult patient. Anaesthesia 2011; 66(Suppl 2): 65-80.
Hagberg CA, Greger J, Chelly JE, Saad-Eddin HE. Instruction of airway management skills during anesthesiology residency training. J Clin Anesth 2003; 15: 149-53.
Wong DT, Prabhu AJ, Coloma M, Imasogie N, Chung FF. What is the minimum training required for successful cricothyroidotomy?: a study in mannequins. Anesthesiology 2003; 98: 349-53.
Funding sources
Supported in part by the Department of Anesthesia, University of Toronto, Canada.
Conflicts of interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Author contributions
David T. Wong was responsible for conception of the survey and writing the manuscript. Arpan Mehta and Brian Yau contributed to the design of the questionnaire. Arpan Mehta and Jean Wong contributed to the data analysis. Arpan Mehta, Amanda D. Tam, and Jean Wong contributed to writing the manuscript. Amanda D. Tam contributed to the statistical analysis. Brian Yau contributed to programming the questionnaire on SurveyMonkey®.
Appendix
Appendix



Rights and permissions
About this article
Cite this article
Wong, D.T., Mehta, A., Tam, A.D. et al. A survey of Canadian anesthesiologists’ preferences in difficult intubation and “cannot intubate, cannot ventilate” situations. Can J Anesth/J Can Anesth 61, 717–726 (2014). https://doi.org/10.1007/s12630-014-0183-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12630-014-0183-0