Abstract
Background
Polypharmacy, frailty and malnutrition are known predictors of adverse outcomes in dialysis patients. Little has reported about their interaction and composite prognostic values. We aimed to describe the interaction between polypharmacy, frailty, nutrition, hospitalization, and survival in peritoneal dialysis patients.
Methods
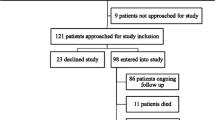
In this prospective cohort study, we recruited 573 peritoneal dialysis patients. Drug burden was measured by medication number and daily pill load. Frailty and nutrition were assessed by the validated Frailty Score (FQ) and Subjective Global Assessment (SGA) respectively. All patients were followed for two years. Primary outcome was all-cause mortality. Secondary outcomes were fall and fracture episodes, hospitalization, change in FQ and SGA.
Results
At baseline, each patient took 7.5 ± 2.6 medications with 15.5 ± 8.5 tablets per day. Medication number, but not daily pill load predicted baseline FQ (p = 0.004) and SGA (p = 0.03). Over 2 years, there were 69 fall and 1,606 hospitalization episodes. In addition, 148 (25.8%) patients died, while FQ and SGA changed by 0.73 ± 4.23 and −0.07 ± 1.06 respectively in survivors. Medication number (hospitalization: p = 0.02, survival: p = 0.005), FQ (hospitalization: p < 0.001; survival: p = 0.01) predicted hospitalization and survival. Medication number also predicted fall episodes (p = 0.02) and frailty progression (p = 0.002). Daily pill load did not predict any of these outcomes.
Conclusions
Drug burden is high in peritoneal dialysis patients, and it carries important prognostic implication. Medication number but not pill load significantly predicted onset and progression of frailty, malnutrition, fall, hospitalization, and mortality.



Similar content being viewed by others
Data availability statement: Data available on request due to privacy/ethical restrictions.
References
Collaboration GBDCKD. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395(10225):709–33.
Ballew SH, Chen Y, Daya NR, Godino JG, Windham BG, McAdams-DeMarco M, et al. Frailty, Kidney Function, and Polypharmacy: The Atherosclerosis Risk in Communities (ARIC) Study. Am J Kidney Dis. 2017;69(2):228–36.
Battistella M, Ng P. Addressing Polypharmacy in Outpatient Dialysis Units. Clin J Am Soc Nephrol. 2020;16(1):144–6.
Pantuzza LL, Ceccato M, Silveira MR, Junqueira LMR, Reis AMM. Association between medication regimen complexity and pharmacotherapy adherence: a systematic review. Eur J Clin Pharmacol. 2017;73(11):1475–89.
Sommer J, Seeling A, Rupprecht H. Adverse Drug Events in Patients with Chronic Kidney Disease Associated with Multiple Drug Interactions and Polypharmacy. Drugs Aging. 2020;37(5):359–72.
Chang TI, Park H, Kim DW, Jeon EK, Rhee CM, Kalantar-Zadeh K, et al. Polypharmacy, hospitalization, and mortality risk: a nationwide cohort study. Sci Rep. 2020;10(1):18964.
van Oosten MJM, Logtenberg SJJ, Hemmelder MH, Leegte MJH, Bilo HJG, Jager KJ, et al. Polypharmacy and medication use in patients with chronic kidney disease with and without kidney replacement therapy compared to matched controls. Clin Kidney J. 2021;14(12):2497–523.
Szeto CC, Chan GC, Ng JK, Chow KM, Kwan BC, Cheng PM, et al. Depression and Physical Frailty Have Additive Effect on the Nutritional Status and Clinical Outcome of Chinese Peritoneal Dialysis. Kidney Blood Press Res. 2018;43(3):914–23.
Wu PY, Chao CT, Chan DC, Huang JW, Hung KY. Contributors, risk associates, and complications of frailty in patients with chronic kidney disease: a scoping review. Ther Adv Chronic Dis. 2019;10:2040622319880382.
Chan GC, N GJ, Chow KM, Kwong VW, Pang WF, Cheng PM, et al. Interaction between central obesity and frailty on the clinical outcome of peritoneal dialysis patients. PLoS One. 2020;15(10):e0241242.
Chan GC, Ng JK, Chow KM, Kwong VW, Pang WF, Cheng PM, et al. Progression in Physical Frailty in Peritoneal Dialysis Patients. Kidney Blood Press Res. 2021;46(3):342–51.
Chen JB, Lam KK, Su YJ, Lee WC, Cheng BC, Kuo CC, et al. Relationship between Kt/V urea-based dialysis adequacy and nutritional status and their effect on the components of the quality of life in incident peritoneal dialysis patients. BMC Nephrol. 2012;13:39.
Chan GC, Ng JK, Chow KM, Kwan BC, Kwong VW, Pang WF, et al. Depression does not predict clinical outcome of Chinese peritoneal Dialysis patients after adjusting for the degree of frailty. BMC Nephrol. 2020;21(1):329.
Mei F, Gao Q, Chen F, Zhao L, Shang Y, Hu K, et al. Frailty as a Predictor of Negative Health Outcomes in Chronic Kidney Disease: A Systematic Review and Meta-Analysis. J Am Med Dir Assoc. 2021;22(3):535–43 e7.
Lo WK, Bargman JM, Burkart J, Krediet RT, Pollock C, Kawanishi H, et al. Guideline on targets for solute and fluid removal in adult patients on chronic peritoneal dialysis. Perit Dial Int. 2006;26(5):520–2.
Peritoneal Dialysis Adequacy Work G. Clinical practice guidelines for peritoneal dialysis adequacy. Am J Kidney Dis. 2006;48 Suppl 1:S98–129.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17(1):230.
Chan GC-K, Ng JK-C, Chow K-M, Kwong VW-K, Pang W-F, Cheng PM-S, et al. Impact of frailty and its inter-relationship with lean tissue wasting and malnutrition on kidney transplant waitlist candidacy and delisting. Clinical Nutrition. 2021.
Enia G, Sicuso C, Alati G, Zoccali C. Subjective global assessment of nutrition in dialysis patients. Nephrol Dial Transplant. 1993;8(10):1094–8.
Ikizler TA, Burrowes JD, Byham-Gray LD, Campbell KL, Carrero JJ, Chan W, et al. KDOQI Clinical Practice Guideline for Nutrition in CKD: 2020 Update. Am J Kidney Dis. 2020;76(3 Suppl 1):S1–S107.
Chu NM, Deng A, Ying H, Haugen CE, Garonzik Wang JM, Segev DL, et al. Dynamic Frailty Before Kidney Transplantation: Time of Measurement Matters. Transplantation. 2019;103(8):1700–4.
Johansen KL, Dalrymple LS, Delgado C, Chertow GM, Segal MR, Chiang J, et al. Factors Associated with Frailty and Its Trajectory among Patients on Hemodialysis. Clin J Am Soc Nephrol. 2017;12(7):1100–8.
Battistella M, Jandoc R, Ng JY, McArthur E, Garg AX. A Province-wide, Cross-sectional Study of Demographics and Medication Use of Patients in Hemodialysis Units Across Ontario. Can J Kidney Health Dis. 2018;5:2054358118760832.
Schmidt IM, Hubner S, Nadal J, Titze S, Schmid M, Barthlein B, et al. Patterns of medication use and the burden of polypharmacy in patients with chronic kidney disease: the German Chronic Kidney Disease study. Clin Kidney J. 2019;12(5):663–72.
Szeto CC, Chow KM, Kwan BC, Leung CB, Chung KY, Law MC, et al. Relation between number of prescribed medication and outcome in peritoneal dialysis patients. Clin Nephrol. 2006;66(4):256–62.
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in Prescription Drug Use Among Adults in the United States From 1999–2012. JAMA. 2015;314(17):1818–31.
Giroux M, Bouchard N, Henderson A, Lam L, Tran VAS, Projean D, et al. Pharmacokinetics of Tobramycin Administered at the Beginning of Intermittent Hemodialysis Session (ESRD Study). Can J Kidney Health Dis. 2021;8:2054358120987061.
Szeto CC, Wong TY, Chow KM, Leung CB, Law MC, Wang AY, et al. Impact of dialysis adequacy on the mortality and morbidity of anuric Chinese patients receiving continuous ambulatory peritoneal dialysis. J Am Soc Nephrol. 2001;12(2):355–60.
Chen YC, Hung KY, Kao TW, Tsai TJ, Chen WY. Relationship between dialysis adequacy and quality of life in long-term peritoneal dialysis patients. Perit Dial Int. 2000;20(5):534–40.
Gaweda AE, Goldsmith LJ, Brier ME, Aronoff GR. Iron, inflammation, dialysis adequacy, nutritional status, and hyperparathyroidism modify erythropoietic response. Clin J Am Soc Nephrol. 2010;5(4):576–81.
Ng JK, Kwan BC, Chan GC, Chow KM, Pang WF, Cheng PM, et al. Predictors and prognostic significance of persistent fluid overload: A longitudinal study in Chinese peritoneal dialysis patients. Perit Dial Int. 2022:8968608221110491.
Vaios V, Georgianos PI, Liakopoulos V, Agarwal R. Assessment and Management of Hypertension among Patients on Peritoneal Dialysis. Clin J Am Soc Nephrol. 2019;14(2):297–305.
Ryta A, Chmielewski M, Debska-Slizien A, Jagodzinski P, Sikorska-Wisniewska M, Lichodziejewska-Niemierko M. Impact of gender and dialysis adequacy on anaemia in peritoneal dialysis. Int Urol Nephrol. 2017;49(5):903–8.
Debowska M, Gomez R, Pinto J, Waniewski J, Lindholm B. Phosphate clearance in peritoneal dialysis. Sci Rep. 2020;10(1):17504.
Griva K, Lai AY, Lim HA, Yu Z, Foo MW, Newman SP. Non-adherence in patients on peritoneal dialysis: a systematic review. PLoS One. 2014;9(2):e89001.
Ghimire S, Castelino RL, Lioufas NM, Peterson GM, Zaidi ST. Nonadherence to Medication Therapy in Haemodialysis Patients: A Systematic Review. PLoS One. 2015;10(12):e0144119.
Laville SM, Gras-Champel V, Moragny J, Metzger M, Jacquelinet C, Combe C, et al. Adverse Drug Reactions in Patients with CKD. Clin J Am Soc Nephrol. 2020;15(8):1090–102.
Chan L, Saha A, Poojary P, Chauhan K, Naik N, Coca S, et al. National Trends in Emergency Room Visits of Dialysis Patients for Adverse Drug Reactions. Am J Nephrol. 2018;47(6):441–9.
Zha Y, Qian Q. Protein Nutrition and Malnutrition in CKD and ESRD. Nutrients. 2017;9(3).
Gafter-Gvili A, Schechter A, Rozen-Zvi B. Iron Deficiency Anemia in Chronic Kidney Disease. Acta Haematol. 2019;142(1):44–50.
Liu WS, Chu DC, Chan HL, Li SY, Liu CK, Yang CY, et al. Fixed dose of long-acting erythropoietic stimulating agents at higher frequency improves appetite, reduces inflammation and corrects anaemia in patients on haemodialysis. Clin Exp Pharmacol Physiol. 2016;43(10):875–82.
Inoue A, Ishikawa E, Shirai Y, Murata T, Miki C, Hamada Y. Effects of Protein-Energy Wasting (PEW) and hyperphosphatemia on the prognosis in Japanese maintenance hemodialysis patients: A five-year follow-up observational study. Clin Nutr ESPEN. 2020;36:134–8.
Vich Vila A, Collij V, Sanna S, Sinha T, Imhann F, Bourgonje AR, et al. Impact of commonly used drugs on the composition and metabolic function of the gut microbiota. Nat Commun. 2020;11(1):362.
Valuck RJ, Ruscin JM. A case-control study on adverse effects: H2 blocker or proton pump inhibitor use and risk of vitamin B12 deficiency in older adults. J Clin Epidemiol. 2004;57(4):422–8.
Leonard J, Marshall JK, Moayyedi P. Systematic review of the risk of enteric infection in patients taking acid suppression. Am J Gastroenterol. 2007;102(9):2047–56; quiz 57.
Lau AN, Tomizza M, Wong-Pack M, Papaioannou A, Adachi JD. The relationship between long-term proton pump inhibitor therapy and skeletal frailty. Endocrine. 2015;49(3):606–10.
Strid H, Simren M, Bjornsson ES. Overuse of acid suppressant drugs in patients with chronic renal failure. Nephrol Dial Transplant. 2003;18(3):570–5.
Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol. 2009;4(6):1089–96.
Parker K, Nikam M, Jayanti A, Mitra S. Medication burden in CKD-5D: impact of dialysis modality and setting. Clin Kidney J. 2014;7(6):557–61.
Kiebalo T, Holotka J, Habura I, Pawlaczyk K. Nutritional Status in Peritoneal Dialysis: Nutritional Guidelines, Adequacy and the Management of Malnutrition. Nutrients. 2020;12(6).
Leung CB, Cheung WL, Li PK. Renal registry in Hong Kong-the first 20 years. Kidney Int Suppl (2011). 2015;5(1):33–8.
Acknowledgements
This study was supported by the Richard Yu Chinese University of Hong Kong (CUHK) PD Research Fund, and CUHK research accounts 6905134 and 7105912.
Funding
Funding sources: This study was supported by the Richard Yu Chinese University of Hong Kong (CUHK) PD Research Fund, and CUHK research accounts 6905134 and 7105912. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Author contributions: Gordon Chun-Kau CHAN: Conceptualization, Methodology, Data curation, Formal analysis, Writing — Original Draft, Project administration. Jack Kit-Chung NG: Investigation, Data curation, Writing — Review & Editing. Kai-Ming CHOW: Investigation. Phyllis Mei-Shan CHENG: Investigation. Man-Ching LAW: Investigation. Chi-Bon LEUNG: Investigation. Philip Kam-Tao LI: Supervision. Cheuk-Chun SZETO: Conceptualization, Methodology, Data curation, Writing — Review & Editing, Supervision.
Corresponding author
Ethics declarations
Conflict of interest statement: Dr. CC Szeto receives research grant and consultancy from Baxter Healthcare. The authors declare no other conflict of interest. The results presented in this paper have not been published previously in whole or part, except in abstract format.
Ethical standards: The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Institutional Review Board of Joint Chinese University of Hong Kong — New Territories East Cluster Clinical Research Ethics Committee (Approval number: CRE-2012.311).
Additional information
Informed consent statement: Informed consent was obtained from all subjects involved in the study.
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Chan, G.CK., Ng, J.KC., Chow, KM. et al. Polypharmacy Predicts Onset and Transition of Frailty, Malnutrition, and Adverse Outcomes in Peritoneal Dialysis Patients. J Nutr Health Aging 26, 1054–1060 (2022). https://doi.org/10.1007/s12603-022-1859-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12603-022-1859-8