Abstract
Purpose
This study aimed to analyze the use of electronic medical records (EMRs) to improve patient engagement with health information. The study examined two distinct behaviors: continued use of EMRs and not using EMRs (non-adoptive behavior).
Methods
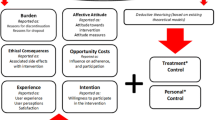
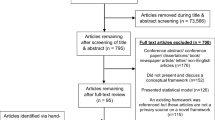
Secondary analysis of a cross-sectional national survey was conducted. The data were interpreted within the Unified Theory of Acceptance and Use of Technology (UTAUT) model to assess the factors that influenced patients’ use of EMRs. Logistic regression analyses were also carried out to identify the significant predictors of non-adoptive behavior.
Results
The results of the study showed that the degree to which participants perceived the technology as easy to use, prior experience in accessing health data through technology, frequency of provider visits, and perceived poor health were indicators of continued use of EMRs. Logistic regression analyses revealed that gender, age, race/ethnicity, education, and type of insurance coverage were significant predictors of some of the barriers/preferences of non-adoptive behavior.
Conclusions
The study concluded that the UTAUT model can be effectively applied in healthcare settings to better understand patients’ use of EMRs and improve health information exchange between healthcare providers and patients. Further exploration is needed to differentiate between various behaviors to better meet the needs of patients and improve health outcomes. Overall, the findings highlight the importance of considering patient factors when implementing EMR systems in healthcare settings.
Similar content being viewed by others
References
Guttmacher S, Tiersten D. Digital health records: a viewpoint on impact on medical practice and potential implications for both communication and future research. J Healthc Commun. 2014. https://doi.org/10.1179/1753806814Z.00000000062.
Michas F. Impact of electronic health records on U.S. physicians’ practices 2018. 2020. In: Statista – The Statistics Portal. https://www.statista.com/statistics/614068/us-physicans-electronic-health-record-practice-impact/#statisticContainer. Accessed 2 Feb 2023.
Saeed SA, Masters RM. Disparities in Health Care and the Digital divide. Curr Psychiatry Rep. 2021. https://doi.org/10.1007/s11920-021-01274-4.
Centers for Medicare and Medicaid Services. In: E-Health Records. 2021. https://www.cms.gov/Medicare/E-Health/EHealthRecords. Accessed 15 Nov 2023.
Steward C. Type of medical information patients would want access via EHRs in the U.S 2020. In: Statista – The Statistics Portal. 2022. https://www.statista.com/statistics/1335858/information-patients-would-want-to-access-in-ehrs-in-the-us/. Accessed 2 Feb 2023.
Ant Ozok A, Huijuan W, Garrido M, Pronovost PJ, Gurses AP. Usability and perceived usefulness of personal health records for preventive health care: a case study focusing on patients’ and primary care providers’ perspectives. Appl Ergon. 2014. https://doi.org/10.1016/j.apergo.2013.09.005.
Dhanireddy S, Walker J, Reisch L, Oster N, Delbanco T, Elmore JG. The urban underserved: attitudes towards gaining full access to electronic medical records. Health Expect. 2014. https://doi.org/10.1111/j.1369-7625.2012.00799.
Greiver M. 2015. Do electronic medical records improve quality of care?: No. Canadian Family Physician. 2015; 61:847–849.
Rexhepi H, Åhlfeldt RM, Cajander Ã, Huvila I. Cancer patients’ attitudes and experiences of online access to their electronic medical records: a qualitative study. Health Inf J. 2018. https://doi.org/10.1177/1460458216658778.
Ralston JD, Revere D, Robins LS, Goldberg HI. Patients’ experience with a diabetes support programme based on an interactive electronic medical record: qualitative study. BMJ. 2004. https://doi.org/10.1136/bmj.328.7449.1159.
Manca DP. Do electronic medical records improve quality of care? Yes. Can Fam Physician. 2015;61:846–7.
Ancker JS, Nosal S, Hauser D, Way C, Calman N. Access policy and the digital divide in patient access to medical records. Health Policy Technol. 2017. https://doi.org/10.1016/j.hlpt.2016.11.004.
Sadoughi F, Khodaveisi T, Ahmadi H. The used theories for the adoption of electronic health record: a systematic literature review. Health Technol. 2019. https://doi.org/10.1007/s12553-018-0277-8.
Mukhopadhyay S, Basak R, Carpenter D, Reithel BJ. Patient use of online medical records: an application of technology acceptance framework. Inf Comput Secur. 2019. https://doi.org/10.1108/ICS-07-2019-0076.
Mishra A, Baker-Eveleth L, Gala P, Stachofsky J. Factors influencing actual usage of fitness tracking devices: empirical evidence from the UTAUT model. Health Mark Q. 2022. https://doi.org/10.1080/07359683.2021.1994170.
Wang H, Tao D, Yu N, Qu X. Understanding consumer acceptance of healthcare wearable devices: an integrated model of UTAUT and TTF. Int J Med Inform. 2020. https://doi.org/10.1016/j.ijmedinf.2020.104156.
Cellucci LW, Cellucci T, Stanton M, Kerrigan D, Madrake M. Current status and future directions of EMR use in psychology clinics. Health Policy Technol. 2015. https://doi.org/10.1016/j.hlpt.2015.02.005.
Enaizan O, Zaidan AA, Alwi NHM, Zaidan BB, Alsalem MA, Albahri OS, Albahri AS. Electronic medical record systems: decision support examination framework for individual, security and privacy concerns using multi-perspective analysis. Health Technol. 2020. https://doi.org/10.1007/s12553-018-0278-7.
Kijsanayotin B, Pannarunothai S, Speedie SM. Factors influencing health information technology adoption in Thailand’s community health centers: applying the UTAUT model. Int J Med Inform. 2008. https://doi.org/10.1016/j.ijmedinf.2008.12.005.
Shiferaw KB, Mehari EA. Modeling predictors of acceptance and use of electronic medical record system in a resource limited setting: using modified UTAUT model. Inf Med Unlocked. 2019. https://doi.org/10.1016/j.imu.2019.100182.
Venkatesh V, Zhang X, Sykes TA. Doctors do too little technology: a longitudinal field study of an Electronic Healthcare System implementation. Inf Syst Res. 2011. https://doi.org/10.1287/isre.1110.0383.
Venkatesh V, Bala H. Technology Acceptance Model 3 and a Research Agenda on Interventions. Decis Sci. 2008. https://doi.org/10.1111/j.1540-5915.2008.00192.x.
Ojinnaka CO, Adepoju OE. Racial and ethnic disparities in Health Information Technology Use and Associated Trends among individuals living with chronic Diseases. Popul Health Manag. 2021. https://doi.org/10.1089/pop.2021.0055.
Venkatesh V, Morris MG, Davis GB, Davis FD. User Acceptance of Information Technology: toward a unified view. MIS Q. 2003. https://doi.org/10.2307/30036540.
Tan PJB. Applying the UTAUT to understand factors affecting the Use of English E-Learning websites in Taiwan. SAGE Open. 2013. https://doi.org/10.1177/2158244013503837.
Venkatesh V, Thong J, Xu X. Unified theory of Acceptance and Use of Technology: a synthesis and the Road ahead. J Assoc Inf Sci Technol. 2016. https://doi.org/10.17705/1jais.00428.
Fishbein M, Ajzen I. Belief, attitude, intention, and behavior: an introduction to theory and research. Reading: MA:Addison-Wesley; 1975.
Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice- Hall; 2002.
Venkatesh V, Davis FD. A theoretical extension of the Technology Acceptance Model: four Longitudinal Field Studies. Manage Sci. 2000. https://doi.org/10.1287/mnsc.46.2.186.11926. (Management Science).
Fishbein M. A reasoned Action Approach to Health Promotion. Med Decis Making. 2008. https://doi.org/10.1177/0272989X08326092.
Davis FD, Perceived, Usefulness. Perceived ease of Use, and user Acceptance of Information Technology. MIS Q. 1989. https://doi.org/10.2307/249008.
Charness N, Boot WR, Technology. Gaming, and Social networking. In: Schaie KW, Willis SL, editors. Handbook of the psychology of aging. Academic Press; 2016. pp. 389–407.
Holden RJ, Karsh BT. The Technology Acceptance Model: its past and its future in health care. J Biomed Inform. 2010. https://doi.org/10.1016/j.jbi.2009.07.002.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991. https://doi.org/10.1016/0749-5978(91)90020-T.
Yu C. Factors affecting individuals to adopt mobile banking: empirical evidence from the UTAUT model. J Electron Commer Res. 2012;13:2–104.
Dwivedi YK, Rana NP, Jeyaraj A, Clement M, Williams MD. Re-examining the Unified Theory of Acceptance and Use of Technology (UTAUT): towards a revised theoretical model. Inf Syst Front. 2019. https://doi.org/10.1007/s10796-017-9774-y.
Dwivedi YK, Rana NP, Tamilmani K, Raman R. A meta-analysis based modified unified theory of acceptance and use of technology (meta-UTAUT): a review of emerging literature. Curr Opin Psychol. 2020. https://doi.org/10.1016/j.copsyc.2020.03.008.
Jewer J. Patients’ intention to use online postings of ED wait times: a modified UTAUT model. Int J Med Inform. 2018. https://doi.org/10.1016/j.ijmedinf.2018.01.008.
Westat. (2020). Health Information National Trends Survey 5 (HINTS 5). In: National Cancer Institute. https://hints.cancer.gov/docs/methodologyreports/HINTS5_Cycle4_MethodologyReport.pdf. Accessed 13 Oct 2022.
Kaazan P, Li T, Seow W, Bednarz J, Pipicella JL, Krishnaprasad K, Ng W, Williams A-J, Connor SJ, Andrews JM. Assessing effectiveness and patient perceptions of a novel electronic medical record for the management of inflammatory bowel disease. JGH Open. 2021. https://doi.org/10.1002/jgh3.12631.
Winkelman WJ, Lenord, Patient-Perceived Usefulness of Online Electronic Medical Records. Employing grounded theory in the development of information and Communication Technologies for Use by Patients living with chronic illness. J Am Med Inform Assoc. 2005. https://doi.org/10.1197/jamia.M1712.
Alhasan A, Audah L, Ibrahim I, Al-Sharaa A, Al-Ogaili AS, Jabiry MM. A case-study to examine doctors’ intentions to use of IT healthcare devices in Iraq during COVID-19 pandemic. Int J Pervasive Comput. 2022. https://doi.org/10.1108/IJPCC-10-2020-0175.
Scheper H, Derogee R, Mahdad R, van der Wal RJP, Nelissen RGHH, Visser LG, de Boer MGJ. A mobile app for postoperative wound care after arthroplasty: ease of use and perceived usefulness. Int J Med Inform. 2019. https://doi.org/10.1016/j.ijmedinf.2019.05.010.
Langford AT, Orellana K, Buderer N. Use of Online Medical Records to support medical decision making: a cross-sectional study of US adults. J Health Commun. 2021. https://doi.org/10.1080/10810730.2021.1983893.
Koch-Weser S, Bradshaw YS, Gualtieri L, Gallagher SS. The internet as a Health Information source: findings from the 2007 Health Information National Trends Survey and Implications for Health Communication. J Health Commun. 2010. https://doi.org/10.1080/10810730.2010.522700.
Funding
The author declares that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
The author confirms sole responsibility for the study conception, data analysis, interpretation of results, and writing of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval and participant consent was not necessary as this study involved the use of a de-identified publicly available dataset.
Consent for publication
Not applicable.
Competing Interests
The author reports there are no competing interests to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Altinay, Z. Electronic medical records and patient engagement: examining post-adoptive and non-adoptive behavior. Health Technol. 13, 799–810 (2023). https://doi.org/10.1007/s12553-023-00778-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12553-023-00778-8