Abstract
Purpose
The purpose of this research was to study the stress distribution at the bone–implant contact in the pick-up implant impression technique. The mechanical properties and the curing dynamics of Pattern Resin LS were previously investigated.
Materials and methods
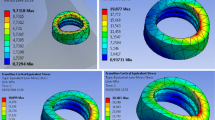
Measurements of the elastic modules of Pattern Resin LS were carried out after complete curing by standard stress–strain tests and a three-point bending technique. A specific laboratory set-up was implemented to monitor the curing dynamics and the linear contraction by using optical imaging methods. A finite element model (FEM) was created and a complete assembly was made with 33 solid bodies representing the main components of the system including the external portion of cortical bone, the internal portion of trabecular bone, six implants, six copings, one bridging structure (modular individual tray), six modules, and six pattern resin layers to fill up the interstitial spaces. Isotropic characteristics for cortical and trabecular bone were incorporated. The stress distribution was measured at the total body of the bone–implant interface, at the external cortical bone surface, at the coping–implant connection area, and at the tray–coping junction. Parametric analysis was also done to study the behavior of two types of internal connection in the impression phase: type A consisting of a 0.4 mm tube-in-tube connection with a triangular head by three cams (Cam-Log Biotechnologies, Germany); type B consisting of a 0.5-mm internal hexagonal connection (Biomet 3i, USA).
Results
The measured values of Young’s modulus and the flexural modulus of the resin were 1.58 ± 0.12 GPa and 2.07 ± 0.24 GPa, respectively. The final volume contraction was found to be strongly dependent on the powder/liquid ratio; specifically, the tests suggested that the highest value of the powder/liquid ratio (2:1) was the most favorable one. In all cases, however, the Pattern Resin behavior was within the linear elastic range, without any permanent deformation or detachment. At individual tray–Pattern Resin interfaces, a stress of about 20.0 MPa was produced for each component; FEM analysis showed that the stress level at the implant–transfer copings connection was higher than that at the bone–implant interface. The trabecular and cortical bone showed the lowest level of stress concentration. B-type transfer showed a higher stress at the transfer coping–implant connection; A-type transfer coping allowed for a higher deformation area, increasing the risk of detachment.
Conclusions
The mechanical properties of Pattern Resin LS seem to be appropriate for use in the pick-up impression technique thanks to the low-volume contraction, the capabilities to dampen misfits, and permanent deformation effects. The shape of the copings affects the values of the stress both in the transfer coping–implant connection zones and at resin–transfer coping interfaces. A thicker clearance of the module–tray connection helps in reducing the mechanical stress. The FEM analysis showed that the removal procedure of the pick-up implant impression tray does not produce any irreversible damage on the cortical and trabecular bone structure. Since the yield threshold was high, the stress distribution at the bone–implant–coping configurations was largely within the safety range for the multiple internal-connection implants, in combination with a modular individual impression tray.









Similar content being viewed by others
References
Vigolo P, Millstein PL. Evaluation of master cast technique for multiple abutment implant prostheses. Int J Oral Maxillofac Implant. 1993;8:439–45.
Barrett MG, de Rijk WG, Burges JO. The accuracy of six impression techniques for osseointegrate implants. J Prosthodont. 1993;2:75–82.
Hussaini S, Wung T. One clinical visit for a multiple implant restoration master cast fabrication. J Prosthet Dent. 1997;78:550–3.
Matsushita Y, Kihara M. A modified implant impression technique. J Prosthet Dent. 2002;87:343–4.
Carr AB. Comparison of impression techniques for a five-implants mandibular model. Int J Oral Maxillofac Implants. 1991;6:448–55.
Kim S, Nicoholls JI, Han CH, Lee KW. Displacement of implant component from impression to definitive cast. Int J Maxillofac Implants. 2006;21:747–55.
Simeone P, Valentini PP, Pizzoferrato R, Scudieri F. Dimensional accuracy of pick-up implant impression: an in vitro comparison of modular versus standard custom trays. Int J Oral Maxillofac Implants. 2011;26:538–46.
Takahashi J, Kitahara K, Teraoka F, Kubo F. Resin pattern material with low polymerization shrinkage. Int J Prosthodont. 1999;12(4):325–9.
McDonnell T, Houston F, Byrne D, Gorman C, Claffey N. The effect of time lapse on the accuracy of two acrylic resins used to assemble an implant framework for soldering. J Prosthet Dent. 2004;91(6):538–40.
Sato Y, Teixeira ER, Tsuga K, Shindoi N. The effectiveness of a new algorithm on a three-dimensional finite element model construction of bone trabeculae in implant biomechanics. J Oral Rehabil. 1999;26:640–3.
O’Mahony AM, Williams JL, Katz JO, Spencer P. Anisotropic elastic properties of cancellous bone from a human edentulous mandible. Clin Oral Implants Res. 2000;11:415–21.
Al-Sukhum J, Kelleway J, Helenius M. Devolopment of a three-dimensional finite element model of a human mandible containing endosseous dental implants. I. Mathematical validation and experimental verification. J Biomed Mater Res A. 2007;80:234–46.
O’Mahony AM, Williams JL, Spencer P. Anisotropic elasticity of cortical and cancellous bone in the posterior mandible increases per-implant stress and strain under oblique loading. Clin Oral Implants Res. 2001;12:648–57.
Schwartz-Dabney CL, Dechow PC. Edentulation alters material properties of cortical bone in the human mandible. J Dent Res. 2002;81:613–7.
Himmlová L, Dostálová T, Kácovský A, Konvicˇková S. Influence of implant length and diameter on stress distribution: a finite element analysis. J Prosthet Dent. 2004;91(1):20–5.
Ekici B. Numerical analysis of a dental implant system in three-dimensions. Adv Eng Softw. 2002;33:109–13.
Meng RT, Jr., Latta MA. Physical properties of four acrylic denture based resins. J Contemp Dent Pract. 2005;6:1–15.
Barbosa DB, Freitas de Souza R, Pero AC, Marra J, Compagnoni MA. Flexural strength of acrylic resins polymerized by different cycles. J Appl Oral Sci. 2007;15:424–8.
Vallittu PK. Flexural properties of acrylic resin polymers reinforced with unidirectional and woven glass fibers. J Prosthet Dent. 1999;81:318–26.
GC. GC Pattern Resin LS low shrinkage modelling resin tips and tricks: technique and handling of GC Pattern Resin. 2009. p. 1–12. http://www.gcamerica.com/lab/products/PATTERN_RESIN_LS/pattern_resin_tech_guide.pdf. Accessed 22 Oct. 2014.
Kwon T-Y, Han J-Y, Chun J-N, Son JS, Kyo-Han Kim K-H. Effects of prepolymerized particle size and polymerization kinetics on volumetric shrinkage of dental modeling resins. BioMed Res Int. 2014;2014:914739.
Gibbs SB, Versluis V, Tantbirojn D, Ahuja S. Comparison of polymerization shrinkage of Pattern Resins. J Prosthet Dent. 2014;112(2):293–8.
Rajagopal P, Chitre V, Aras MA. A comparison of the accuracy of patterns processed from an inlay casting wax, an auto-polymerized resin and a light-cured resin pattern material. Indian J Dent Res. 2012;23:152–6.
Cerqueira NM, Ozcan M, Gonçalves M, da Rocha DM, Vasconcellos DK, Bottino MA, Yener-Salihog˘lu E. A strain gauge analysis of microstrain induced by various splinting methods and acrylic resin types for implant impressions. Int J Oral Maxillofac Implants. 2012;27(2):341–5.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
P. Simeone, P.P. Valentini, R. Pizzoferrato, and M. Marinelli state that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Simeone, P., Valentini, P., Pizzoferrato, R. et al. Stress distribution and bone–implant interface behavior in pick-up implant impression. J. Stomat. Occ. Med. 7, 97–104 (2014). https://doi.org/10.1007/s12548-014-0114-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12548-014-0114-2