Abstract
Objectives
Occlusal stabilization splints are commonly used for temporomandibular disorders (TMD) related to muscular origins. The aim of the study was to assess the vertical thickness of occlusal stabilization splints under the aspect of maximal therapeutic effectiveness. An attempt was made to establish optimal jaw separation for vertical thickness of occlusal stabilization splints based on bite force (BF) and facial skeletal morphology.
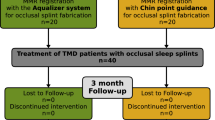
Methods
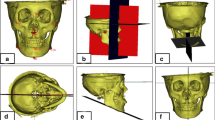
A total of 28 patients diagnosed as having myofascial pain (MFP) were eligible for this study and 3 acrylic occlusal stabilization splints of different vertical thickness were fabricated for each patient. Clinical and subjective examinations were carried out to assess the treatment effectiveness of the splints. Using in-house methods the BF was measured in different vertical jaw separations (VJS). The lateral cephalograms of selected factors were assessed. The relationship between splint thickness, BF and facial skeletal morphology was evaluated.
Results
There was statistically significant correlation between vertical thickness of the splint and treatment effectiveness as well as between the VJS at which the first minimum BF generated in patients was measured and the VJS for the vertical thickness of the splint with maximum therapeutic effectiveness.
Conclusions
The VJS for vertical thickness of occlusal stabilization splints should be established individually for each patient. The VJS at the first minimum BF is essential for establishing the vertical thickness of occlusal stabilization splints to obtain the maximum treatment effectiveness.
Clinical Significance
It is possible to establish the VJS for vertical thickness of occlusal stabilization splints individually for each patient using a formula generated from BF measurements and lateral cephalometric analyses.

Similar content being viewed by others
References
Dworkin SF, LeResche L. Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomand Disord Facial Oral Pain. 1992;6(4):301–55.
Greene CS. Managing patients with temporomandibular disorders: a new “standard of care”. Am J Orthod Dentofacial Orthop. 2010;138:3–4.
Raphael KG, Marbach JJ, Klausner J. Myofascial face pain. Clinical characteristics of those with regional vs, widespread pain. J Am Dent Assoc. 2000;131:161–71.
Svensson P, Graven-Nielsen T. Craniofacial muscle pain: review of mechanisms and clinical manifestations. J Orofac Pain. 2001;15(2):117–45.
McNeill C. Management of temporomandibular disorders: concepts and controversies. J Prosthet Dent. 1997;77:510–22.
Westesson PL, Bronstein SL, Liedberg J. Internal derangement of the temporomandibular joint: morphologic description with correlation to joint function. Oral Surg Oral Med Oral Pathol. 1985;59:323–31.
Greene CS. Managing TMD patients: initial therapy is the key. J Am Dent Assoc. 1992;123(6):43–5.
List T, Axelsson S. Management of TMD: evidence from systematic reviews and meta-analyses. Review article. J Oral Rehabil. 2010;37:430–51.
Ash M, Ramfjord P. Occlusion. 4th ed. Philadelphia: Saunders; 1995.
Raphael KG, Marbach JJ. Widespread pain and the effectiveness of oral splints in myofascial face pain. J Am Dent Assoc. 2001;132:305–16.
DuPont JS, Brown CE. Occlusal splints from the beginning to the present. J Craniomand Prac. 2006;24(2):141–5.
Ré JP, Perez C, Darmouni L, Carlier JF, Orthlieb J-D. The occlusal splint therapy. Int J Stomat Occ Med. 2009;2:82–6.
Türp JC, Komine F, Hugger A. Efficacy of stabilization splints for the management of patients with masticatory muscle pain: a qualitative systematic review. Clin Oral Invest. 2004;8:179–95.
Al-Ani Z, Gray RJ, Davies SJ, Sloan P, Path FRC, Glenny A-M. Stabilization splint therapy for the treatment of temporomandibular myofascial pain: a systematic review. J Dent Educ. 2005;69(11):1242–50.
Davies SJ, Gray RJ. The pattern of splint usage in the management of two common temporomandibular disorders. Part II: The stabilisation splint in the treatment of pain dysfunction syndrome. Br Dent J. 1997;183:247–51.
Clark T. A critical evaluation of orthopedic interocclusal appliance therapy: effectiveness for specific symptoms. J Am Dent Assoc. 1984;108:364–68.
Alvarez-Arenal A, Junquera LM, Fernandez JP. Effect of occlusal splint and transcutaneous electric nerve stimulation on the signs and symptoms of temporomandibular disorders in patients with bruxism. J Oral Rehabil. 2001;29:858–63.
Dao TT, Lavigne GJ, Charbonneau A, Feine JS, Lund JP. The efficacy of oral splints in the treatment of myofascial pain of the jaw muscles: a controlled clinical trial. Pain. 1994;56:85–94.
Lundh H, Westesson P-L, Eriksson L, Brooks SL. Temporomandibular joint disk displacement without reduction. Treatment with flat occlusal splint versus no treatment. Oral Surg Oral Med Oral Pathol. 1992;73:655–8.
Sheikholeslam A, Holmgren K, Riise C. Therapeutic effects of the plane occlusal splint on signs and symptoms of craniomandibular disorders in patients with nocturnal bruxism. J Oral Rehabil. 1993;20:473–82.
Kurita H, Kurashima K, Ohtsuka A, Katani A. Change of position of the temporomandibular joint disk with insertion of a disk—repositioning appliance. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1988;85:142–5.
Donovan TE, Anderson M, Becker W, Cagna DR, Hilton TJ, Rouse J. Annual review of selected scientific literature: report of the committee on scientific investigation of the American Academy of Restorative Dentistry. J Prosthet Dent. 2011;106:224–65.
Kawazoe Y, Kotani H, Hamada T, Yamada S. Effect of occlusal splints on the electromyographic activities of masseter muscles during maximum clenching in patients with myofascial pain—dysfunction syndrome. J Prosthet Dent. 1980;43:578–80.
Attanasio R. Intraoral orthotic therapy. Dent Clin North Am. 1997;41:309–24.
Carlsson GE, Ingervall B, Kocak G. Effect of increasing vertical dimension on the masticatory system in subjects with natural teeth. J Prosthet Dent. 1979;41:284–9.
Drago CJ, Rugh JD, Barghi N. Nightguard vertical thickness effects on nocturnal bruxism. J Dent Res. 1979;58:A901.
Manns A, Mirrales R, Cumsile F. Influence of vertical dimension on masseter muscle electromyographic activity in patients with mandibular dysfunction. J Prosthet Dent. 1985;53:243–7.
Suvinen TI, Reade PC, Kononen M, Kemppainen P. Vertical jaw separation and masseter muscle electromyographic activity: a comparative study between asymptomatic controls and patients with temporomandibular pain and dysfunction. J Oral Rehabil. 2003;30:765–72.
Ferrario VF, Sforza C, Tartaglia GM, Dellavia C. Immediate effect of a stabilization splint on masticatory muscle activity in temporomandibular disorders patients. J Oral Rehabil. 2001;29:810–15.
Humsi ANK, Naeije M, Hipp JA, Hansson TL. The immediate effects of a stabilization splint on the muscular symmetry in the masseter and anterior temporal muscles of patients with craniomandibular disorders. J Prosthet Dent. 1989;62:339–43.
Look JO, Schiffman EL, Truelove EL, Ahmad M. Reliability and validity of Axis I of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/TMD) with proposed revisions. J Oral Rehabil. 2010;37:744–59.
Rakosi T. An atlas and manual of cephalometric radiography. 2nd ed. Philadelphia: Lea & Febiger; 1992.
Jarabak JR, Fizzel JA. Light wire edgewise appliance. St. Louis: Mosby; 1972.
Proffit WR, Fields HW, Nixon WL. Occlusal forces in normal- and long-face adults. J Dent Res. 1983;62(5):566–71.
Greene CS. The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain. 2001;15(2):93–105.
Dworkin SF, Massoth DL. Temporomandibular disorders and chronic pain: disease or illness? J Prosthet Dent. 1994;72:29–38.
Cairns BE. Pathophysiology of TMD pain—basic mechanisms and their implications for pharmacotherapy. Review article. J Oral Rehabil. 2010;37:391–410.
Michelotti A, Iodice G. The role of orthodontics in temporomandibular disorders. J Oral Rehabil. 2010;7:411–29.
Wanyura H, Wagner T, Samolczyk-Wanyura D. Borrelia burgdorferi—a potentially aetiological factor in TMJ disorders? Preliminary report. J Craniomaxillofac Surg. 2008;36(1):28–33.
Ohrbach R. Disability assessment in temporomandibular disorders and masticatory system rehabilitation. J Oral Rehabil. 2010;37:452–80.
Ekberg EC, Vallon D, Nilner M. The efficacy of appliance therapy in patients with temporomandibular disorders of mainly myogenous origin. A randomized controlled, short-term trial. J Orofac Pain. 2003;17(2):133–39.
Fricton J. Current evidence providing clarity in management of temporomandibular disorders: summary of a systematic review of randomized clinical trials for intra-oral appliances and occlusal therapies. J Evid Base Dent Pract. 2006;6:48–52.
Murray GM, Peck CC. Orofacial pain and jaw muscle activity: a new model. J Orofac Pain. 2007;21:263–78.
Lobbezoo F, Lavigne GJ. Do bruxism and temporomandibular disorders have cause-and-effect relationship? J Orofac Pain. 1997;11(1):15–23.
Raphael KG, Marbach JJ, Klausner JJ, Teaford MF, Fischoff DK. Is bruxism severity a predictor of oral splint efficacy in patients with myofascial face pain? J Oral Rehabil. 2003;30:17–29.
Lavigne GJ, Khoury S, Abe S, Kamaguchi T, Raphael K. Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil. 2008;35:476–94.
Lobbezoo F, Naeije M. Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil. 2001;28:1085–91.
Klasser GD, Greene CS, Lavigne GJ. Oral appliances and the management of sleep bruxism in adults: a century of clinical applications and search for mechanisms. Int J Prosthodont. 2010;23:453–62.
Manns A, Miralles R, Palazzi C. EMG, bite force, and elongation of the masseter muscle under isometric voluntary contractions and variations of vertical dimension. J Prosthet Dent. 1979;42:674–82.
Manns A, Miralles R, Cumsille F. Influence of vertical dimension on masseter muscle electromyographic activity in patients with mandibular dysfunction. J Prosthet Dent. 1988;59:73–7.
Plesh O, McCall WD Jr, Gross A. The effect of prior jaw motion in the plot of electromyographic amplitude versus jaw position. J Prosthet Dent. 1988;60:369–73.
Manns A, Miralles R, Guerrero F. The changes in electrical activity of the postural muscles of the mandible upon varying the vertical dimension. J Prosthet Dent. 1981;45(4):438–45.
Miles TS, Nordstrom MA, Türker KS. Length-related changes in activation threshold and wave form of motor units in human masseter muscle. J Physiol. 1986;370:457–65.
Fields HW, Proffit WR, Case JC, Vig KW. Variables affecting measurements of vertical occlusal force. J Dent Res. 1986;65(2):135–8.
Tortopidis D, Lyons MF, Baxendale RH, Gilmour WH. The variability of the bite force measurement between sessions, in different positions within dental arch. J Oral Rehabil. 1998;25:681–6.
Lindaur SJ, Gay T, Rendell J. Effect of jaw opening on masticatory muscle EMG—force characteristics. J Dent Res. 1993;72:51–5.
Mackenna BR, Turker KS. Jaw separation and maximum incising force. J Prosthet Dent. 1983;49:726–30.
Miyaura K, Matsuka Y, Morita M, Yamashita A, Watanabe T. Comparison of biting forces in different age and sex groups: a study of biting efficiency with mobile and non-mobile teeth. J Oral Rehabil. 1999;26:223–7.
Kohoyama K, Hatakeyama E, Sasaki T, Azuma T, Karita K. Effect of sample thickness on bite force studied with a multiple-point sheet sensor. J Oral Rehabil. 2001;31:327–34.
Van Der Bilt A, Abbink JH, Fontijn-Tekamp FA, Bosman F. Maximal bite force and EMG during bilateral and unilateral clenching. J Oral Rehabil. 2002;29:878–9.
Ringqvist M. Isometric force and its relation to dimensions of the facial skeleton. Acta Odont Scand.1973;31:35–42.
Glaros AG, Owais Z, Lausten L. Reduction in parafunctional activity: a potential mechanism for the effectiveness of splint therapy. J Oral Rehabil. 2007;34:97–104.
Conflict of Interest
The authors declare that there is no current or potential conflict of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kostrzewa-Janicka, J., Mierzwińska-Nastalska, E., Jarzębski, G. et al. Vertical jaw separation for vertical thickness of occlusal stabilization splint. J. Stomat. Occ. Med. 5, 20–27 (2012). https://doi.org/10.1007/s12548-012-0034-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12548-012-0034-y