Abstract
Background
Admission to a neurological intensive care unit (Neuro-ICU) can increase risk for depressive and anxiety symptoms for both patients and caregivers. To better understand the long-term mental health impact of a Neuro-ICU admission, we examined the dyadic interdependence between depression and anxiety at Neuro-ICU admission with 3-month quality of life (QoL) for patients and caregivers in a longitudinal, observational cohort study.
Method
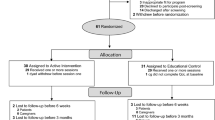
We assessed depressive and anxiety symptoms (Hospital Anxiety and Depression Scale; HADS) reported by neurologically intact patients (n = 72) and their caregivers (n = 72) within 2 weeks of Neuro-ICU admission (baseline) and 3-months post-discharge (follow-up). We examined the longitudinal association between dyadic depression and anxiety at Neuro-ICU admission and 3-month QoL (World Health Organization; QOL-BREF) across four domains (Physical, Psychological, Social relationships, and Environmental QoL) in separate actor-partner interdependence models (APIM) for patients and caregivers.
Results
In the overall models, patients’ own baseline depression levels were negatively associated with their own 3-month QoL in all domains (β = − 0.53 to − 0.64, p < 0.001), and for caregivers, only in the psychological (β = − 0.73, p < .001) and social relationships (β = − 0.56, p < .001) domains. No actor effects were found for one’s own baseline anxiety impacting one’s own 3-month QoL. Partner effects for one’s own depression were significant for caregivers on patients’ 3-month psychological (β = − 0.26, p < .02) and environmental (β = − 0.29, p < .03) QoL, as well as for patients on caregiver’s 3-month psychological QoL (β = 0.25, p < .02). No partner effects were significant in association with baseline anxiety and 3-month QoL in both patients and caregivers.
Conclusion
Neuro-ICU patients’ and caregivers’ baseline depression has significant negative impacts on their own long-term QoL. Caregivers demonstrate significant negative impacts on patient long-term QoL in domains related to emotional distress and caregiver burden. Early identification of mental health symptoms, especially depression, during Neuro-ICU admission may provide an intervention opportunity to improve QoL post-discharge for both dyad members.





Similar content being viewed by others
Data Availability
The data that support the findings of this study are available from the corresponding author, Dr. Ana-Maria Vranceanu, upon reasonable request.
References
Shaffer K, Riklin E, Jacobs J, Rosand J, Vranceanu A. Mindfulness and coping are inversely related to psychiatric symptoms in patients and informal caregivers in the neuroscience ICU: implications for clinical care. Crit Care Med. 2016;44(11):2028–36.
Meyers E, Presciutti A, Shaffer K, Gates M, Lin A, Rosand J, Vranceanu A. The impact of resilience factors and anxiety during hospital admission on longitudinal anxiety among dyads of neurocritical care patients without major cognitive impairment and their family caregivers. Neurocrit Care. 2020;33(2):468–78.
Yousefzadeh-Chabok S, Khodadadi-Hassankiadeh N, Saberi A, Khanghah A, Zarrabi H, Yeganeh M, Hamideh H, Moghadam A. Anxiety, depression, and their related factors in patients admitted to intensive care units. Caspian Journal of Neurological Sciences. 2018;4(4):159–68.
Denno M, Gillard P, Graham G, DiBonaventura M, Goren A, Sepi F, Zorowitz R. Anxiety and depression associated with caregiver burden in caregivers of stroke survivors with spasticity. Arch Phys Med Rehabil. 2013;94(9):1731–6.
Meyers E, Lin A, Lester E, Shaffer K, Rosand J, Vranceanu AM. Baseline resilience and depression symptoms predict trajectory of depression in dyads of patients and their informal caregivers following discharge from the Neuro-ICU. Gen Hosp Psychiatry. 2020;62:87–92.
Rabiee A, Nikayin S, Hashem M, Huang M, Dinglas V, Bienvenu O, Turnbull A, Needham D. Depressive symptoms after critical illness: a systematic review and meta-analysis. Crit Care Med. 2016;44(9):1744–53.
Davydow D, Gifford J, Desai S, Bienvenu O, Needham D. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009;35(5):796–809.
Hwang D, Yagoda D, Perrey H, Currier P, Tehan T, Guanci M, Ananian L, Cobb J, Rosand J. Anxiety and depression symptoms among families of adult intensive care unit survivors immediately following brief length of stay. J Crit Care. 2014;29(2):278–82.
Robinson R, Jorge R. Post-stroke depression: a review. Am J Psychiatry. 2016;173(3):221–31.
Broomfield N, Quinn T, Abdul-Rahim A, Walters M, Evans J. Depression and anxiety symptoms post-stroke/TIA: prevalence and associations in cross-sectional data from a regional stroke registry. BMC Neurol. 2014;14(1):198.
Kapoor A, Si K, Herrmann N, Lanctôt K, Murray B, Swartz R. Abstract TMP42: Younger age and depressive symptoms predict post-stroke generalized anxiety disorder. Stroke (1970), 50(Suppl_1), Stroke (1970), 2019–02, Vol.50 (Suppl_1).
Kreiter K, Rosengart A, Claassen J, Fitzsimmons B, Peery S, Du Y, Connolly E, Mayer S. Depressed mood and quality of life after subarachnoid hemorrhage. J Neurol Sci. 2013;335(1–2):64–71.
Ramirez C, Christophe V, Dassonneville C, Grynberg D. Caregivers’ quality of life and psychological health in response to functional, cognitive, neuropsychiatric and social deficits of patients with brain tumour: protocol for a cross-sectional study. BMJ Open. 2017;7(10):E016308.
Shaffer K, Jacobs J, Coleman J, Greer J, Vranceanu A. Anxiety and depressive symptoms among two seriously medically ill populations and their family caregivers: a comparison and clinical implications. Neurocrit Care. 2017;27(2):180–6.
Zale E, Heinhuis T, Tehan T, Salgueiro D, Rosand J, Vranceanu A. Resiliency is independently associated with greater quality of life among informal caregivers to neuroscience intensive care unit patients. Gen Hosp Psychiatry. 2018;52:27–33.
Oliveira S, Carvalho H, Esteves F. Toward an understanding of the quality of life construct: validity and reliability of the WHOQOL- Bref in a psychiatric sample. Psychiatry Res. 2016;244:37–44.
Skevington S, Lotfy M, O’Connell K. The World Health Organization’s WHOQOL-BREF quality of life assessment: psychometric properties and results of the international field trial. A report from the WHOQOL Group. Qual. Life Res. 2004;13(2):299–310.
Nelson M, Smith M, Martinson B, Kind A, Luepker R. Declining patient functioning and caregiver burden/health: the Minnesota stroke survey–quality of life after stroke study. Gerontologist. 2008;48(5):573–83.
Carod-Artal F, Egido J. Quality of life after stroke: the importance of a good recovery. Cerebrovascular Diseases (Basel, Switzerland). 2009;27(1):204–14.
Shaffer K, Riklin E, Jacobs J, Rosand J, Vranceanu A. Psychosocial resiliency is associated with lower emotional distress among dyads of patients and their informal caregivers in the neuroscience intensive care unit. J Crit Care. 2016;36:154–9.
Presciutti A, Meyers E, Reichman M, Vranceanu A. Associations between baseline total PTSD symptom severity, specific PTSD symptoms, and 3-month quality of life in neurologically intact neurocritical care patients and informal caregivers. Neurocritical Care. 2020-04-30.
Choi K, Shaffer K, Zale E, Funes C, Koenen K, Tehan T, Rosand J, Vranceanu A. Early risk and resiliency factors predict chronic posttraumatic stress disorder in caregivers of patients admitted to a neuroscience ICU. Crit Care Med. 2018;46(5):713–9.
Meyers E, Shaffer K, Gates M, Lin A, Rosand J, Vranceanu A. Baseline resilience and posttraumatic symptoms in dyads of neurocritical patients and their informal caregivers: a prospective dyadic analysis. Psychosomatics (Washington, D.C.). 2020;61(2):135–144.
Stas L, Kenny DA, Mayer A, Loeys T. (In press). Giving dyadic data analysis away: a user-friendly app for actor-partner interdependence models. Personal Relationships.
Kenny DA, Kashy DA, Cook WL. Dyadic data analysis. The Guildford Press. 2006.
Savini S, Buck H, Dickson V, Simeone S, Pucciarelli G, Fida R, Matarese M, Alvaro R, Vellone, E. Quality of life in stroke survivor-caregiver dyads: a new conceptual framework and longitudinal study protocol. Journal of Advanced Nursing Protocol. 2014.
Regan TW, Lambert SD, Kelly B, Falconier M, Kissane D, Levesque JV. Couples coping with cancer: exploration of theoretical frameworks from dyadic studies. Psycho-Oncology. 2015.
Bannon SM, Cornelius T, Gates M, Lester E, Mace R, Popok P, Macklin E, Rosand J, Vranceanu AM. Emotional distress in Neuro-ICU survivor-caregiver dyads: the recovering together randomized clinical trial. Health Psychology. 2021.
Lester EG, Grunberg VA, Bannon SM, Mace RA, Plys E, Jacobo MC, Tehan T, Rosand J, Vranceanu AM. The recovering together initiative: integrating psychosocial care into ICUs. NEJM Catalyst Innovations in Care Delivery. 2022;3(8). https://doi.org/10.1056/CAT.22.0103.
Applebaum A. There is nothing informal about caregiving. Palliat Support Care. 2022;20:621–2.
Vranceanu AM, Bannon S, Mace R, Lester E, Meyers E, Gates M, Popok P, Lin A, Salgueiro D, Tehan T, Macklin E, Rosand J. Feasibility and efficacy of a resiliency intervention for the prevention of chronic emotional distress among survivor-caregiver dyads admitted to the neuroscience intensive care unit: a randomized clinical trial. JAMA Netw Open. 2020;3(10):E2020807.
Harris P, Taylor R, Thielke R, Payne J, Gonzalez N, Conde J. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Zigmond A, Snaith R. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67(6):361–70.
World Health Organization. WHOQOL-BREF introduction, administration, scoring and generic version of the assessment. www.who.int, Field Trial Version December 1996, https://www.who.int/mental_health/media/en/76.pdf. Accessed July 2020.
IBM. IBM SPSS statistics for Windows, version 25.0. 2017.
Fitzpatrick J, Gareau A, LaFontaine M, Gaudreau P. How to use the actor-partner interdependence model (APIM) to estimate different dyadic patterns in MPLUS: a step-by-step tutorial. The Quantitative Methods for Psychology. 2016;12(1):74–86.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Washington, DC: American Psychiatric Association; 2013.
Sannes T, Ranby K, Yusufov M, Brewer B, Jacobs J, Callan S, Ulrich G, Pensak N, Natvig C, Laudenslager M. More often than not, we’re in sync: patient and caregiver well-being over time in stem cell transplantation. Health Qual Life Outcomes. 2022;20:6.
Hackett M, Yapa C, Parag V, Anderson CS. Frequency of depression after stroke: a systematic review of observational studies. Stroke (1970). 2005;36(6):1330–1340.
Alsherbini K, Goyal N, Metter E, Pandhi A, Tsivgoulis G, Huffstatler T, Kelly H, Elijovich L, Malkoff M, Alexandrov A. Predictors for tracheostomy with external validation of the Stroke-Related Early Tracheostomy Score (SETscore). Neurocrit Care. 2019;30(1):185–92.
Jackson J, Mitchell N, Hopkins R. Cognitive functioning, mental health, and quality of life in ICU survivors: an overview. Psychiatr Clin North Am. 2015;38(1):91–104.
Rinkel G, Algra A. Long-term outcomes of patients with aneurysmal subarachnoid haemorrhage. Lancet Neurol. 2011;10(4):349–56.
Chun H, Whiteley W, Dennis M, Mead G, Carson A. Anxiety after stroke: the importance of subtyping. Stroke (1970). 2018;49(3):556–564.
Choi-Kwon S, Kim H, Kwon S, Kim J. Factors affecting the burden on caregivers of stroke survivors in South Korea. Arch Phys Med Rehabil. 2005;86(5):1043–8.
Griffith D, Salisbury L, Lee R, Lone N, Merriweather J, Walsh T. Determinants of health-related quality of life after ICU. Crit Care Med. 2018;46(4):594–601.
McCurley JL, Funes CJ, Zale EL, Lin A, Jacobo M, Jacobs JM, Salgueiro D, Tehan T, Rosand J, Vranceanu AM. Preventing chronic emotional distress in stroke survivors and their informal caregivers. NeuroCrit Care. 2019;30(3):581–9.
Detsky M, Kohn R, Delman A, Buehler A, Kent S, Ciuffetelli I, Mikkelsen M, Turnbull A, Harhay M. Patients’ perceptions and ICU clinicians’ predictions of quality of life following critical illness. J Crit Care. 2018;48:352–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Massachusetts General Hospital Institutional Review Board (IRB) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
Informed consent was obtained from all individual participants included in this study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Quinn, P.A., Mace, R.A., Presciutti, A. et al. Depression Negatively Impacts Dyadic Quality of Life Following Neuro-ICU Admission: A Prospective Study of Cognitively Intact Patients and Caregivers. Int.J. Behav. Med. 31, 97–108 (2024). https://doi.org/10.1007/s12529-022-10149-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-022-10149-8