Abstract
Background
Nightmares and insomnia are significant concerns that commonly co-occur with each other and with other health disorders. Limited research has examined the unique and shared aspects of insomnia and nightmares, and little is known about sleep in US National Guard personnel. This study sought to determine the prevalence and psychosocial correlates of nightmares with and without insomnia in US National Guard personnel.
Method
National Guard personnel (N = 841) completed an online survey and were classified as having nightmares only, insomnia only, both, or neither, using a minimum nightmare frequency of “less than once a week” and an Insomnia Severity Index cutoff of ≥ 15. Analyses examined differences in demographics, physical health, and psychosocial variables and in the prevalence of nightmares and insomnia in personnel with physical and mental health problems.
Results
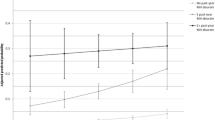
In this sample, 32% reported nightmares only, 4% reported insomnia only, and 12% reported both. Those in the youngest age group (18–21) were more likely to have no nightmares or insomnia. Those with both nightmares and insomnia had more deployments. Nightmares and insomnia were associated with poorer physical and mental health and greater prevalence of comorbid physical and mental health conditions. Personnel with both insomnia and nightmares reported the greatest severity of comorbid conditions.
Conclusion
US National Guard personnel with nightmares and/or insomnia reported worse mental and physical health impairment than those without these conditions. Personnel may benefit from screening for nightmares and insomnia and referrals for evidence-based treatment.
Similar content being viewed by others
References
Sjöström N, Hetta J, Waern M. Persistent nightmares are associated with repeat suicide attempt: a prospective study. Psychiatry Res. 2009;170(2–3):208–11.
Nadorff MR, Nazem S, Fiske A. Insomnia symptoms, nightmares, and suicide risk: duration of sleep disturbance matters. Suicide Life Threat Behav. 2013;43(2):139–49.
Neylan TC, Marmar CR, Metzler TJ, Weiss DS, Zatzick DF, Delucchi KL, et al. Sleep disturbances in the Vietnam generation: findings from a nationally representative sample of male Vietnam veterans. Am J Psychiatry. 1998;155(7):929–33.
Clum GA, Nishith P, Resick PA. Trauma-related sleep disturbance and self-reported physical health symptoms in treatment-seeking female rape victims. J Nerv Ment Dis. 2001;189(9):618–22.
Creamer JL, Brock MS, Matsangas P, Motamedi V, Mysliwiec V. Nightmares in United States military personnel with sleep disturbances. J Clin Sleep Med. 2018;14(03):419–26.
Leger D, Scheuermaier K, Philip P, Paillard M, Guilleminault C. SF-36: evaluation of quality of life in severe and mild insomniacs compared with good sleepers. Psychosom Med. 2001;63(1):49–55.
Taylor DJ, Kelly K, Kohut ML, Song K-S. Is insomnia a risk factor for decreased influenza vaccine response? Behav Sleep Med. 2016:1–18.
Taylor DJ, Lichstein KL, Durrence H. Insomnia as a health risk factor. Behav Sleep Med. 2003;1(4):227–47.
Taylor DJ, Pruiksma KE, Kelly K, et al.; and the STRONG STAR Consortium. Prevalence, correlates, and predictors of insomnia in the US Army prior to deployment. Sleep. 2016;39(10):1795–1806.
Vgontzas AN, Liao D, Pejovic S, Calhoun S, Karataraki M, Basta M, et al. Insomnia with short sleep duration and mortality: the Penn State cohort. Sleep. 2010;33(9):1159–64.
McCall WV. Insomnia is a risk factor for suicide—what are the next steps? Sleep. 2011;34(9):1149–50.
Lincoln ML, Moore RS, Ames GM. Sleep disturbances after deployment: National Guard soldiers’ experiences and strategies. Sleep Health. 2018;4(4):377–83.
Milanak ME, Zuromski KL, Cero I, Wilkerson AK, Resnick HS, Kilpatrick DG. Traumatic event exposure, posttraumatic stress disorder, and sleep disturbances in a national sample of US adults. J Trauma Stress. 2019;32(1):14–22.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 5th ed. Arlington, VA: American Psychiatric Association; 2013.
Kehle SM, Reddy MK, Ferrier-Auerbach AG, Erbes CR, Arbisi PA, Polusny MA. Psychiatric diagnoses, comorbidity, and functioning in National Guard troops deployed to Iraq. J Psychiatr Res. 2011;45(1):126–32.
Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, Hoge CW. Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Arch Gen Psychiatry. 2010;67(6):614–23.
Koffel E, Polusny MA, Arbisi PA, Erbes CR. Pre-deployment daytime and nighttime sleep complaints as predictors of post-deployment PTSD and depression in National Guard troops. J Anxiety Disord. 2013;27(5):512–9.
Gehrman P, Seelig AD, Jacobson IG, Boyko EJ, Hooper TI, Gackstetter GD, et al. Predeployment sleep duration and insomnia symptoms as risk factors for new-onset mental health disorders following military deployment: Sleep. J Sleep Sleep Disord Res. 2013;36(7):1009–18.
Agargun MY, Besiroglu L, Cilli AS, Gulec M, Aydin A, Inci R, et al. Nightmares, suicide attempts, and melancholic features in patients with unipolar major depression. J Affect Disord. 2007;98(3):267–70.
Nishith P, Resick PA, Mueser KT. Sleep difficulties and alcohol use motives in female rape victims with posttraumatic stress disorder. J Trauma Stress. 2001;14(3):469–79.
Ohayon MM, Morselli P, Guilleminault C. Prevalence of nightmares and their relationship to psychopathology and daytime functioning in insomnia subjects. Sleep. 1997;20(5):340–8.
Schredl M, Reinhard I. Gender differences in nightmare frequency: a meta-analysis. Sleep Med Rev. 2011;15(2):115–21.
Morin CM. Insomnia: psychological assessment and management. New York: Guilford Press; 1993.
Morin CM, Belleville G, Bélanger L, Ivers H. The Insomnia Severity Index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34(5):601–8.
Weathers FW, Litz BT, Herman DS, Huska JA, Keane TM, editors. The PTSD Checklist (PCL): reliability, validity, & diagnostic utility. 9th Annual Meeting of the International Society of Traumatic Stress; 1993 October; San Antonio, TX.
Nock MK, Holmberg EB, Photos VI, Michel BD. Self-Injurious Thoughts and Behaviors Interview: development, reliability, and validity in an adolescent sample. Psychol Assess. 2007;19(3):309–17.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9. J Gen Intern Med. 2001;16(9):606–13.
Saunders JB, Aasland OG, Babor TF, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88:791–804.
Kroenke K, Spitzer RL, Williams JB. The PHQ-15: validity of a new measure for evaluating the severity of somatic symptoms. Psychosom Med. 2002;64(2):258–66.
Izard CE, Libero DZ, Putnam P, Haynes OM. Stability of emotion experiences and their relations to traits of personality. J Pers Soc Psychol. 1993;64(5):847–60.
Brenner LA, Homaifar BY, Olson-Madden JH, Nagamoto HT, Huggins J, Schneider AL, et al. Prevalence and screening of traumatic brain injury among veterans seeking mental health services. J Head Trauma Rehabil. 2013;28(1):21–30.
Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. Applied Soc Psychol. 1983;58:304–9.
Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24(4):385–96.
Team RC. R: a language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing www.R-project.org. Accessed September 11, 2019.
Cohen J. Statistical power analysis for the behavioural sciences. Hillsdale: Erlbaum; 1988.
Troxel WM, Shih RA, Pedersen ER, et al. Sleep in the military: promoting healthy sleep among US servicemembers: RAND Health Q 2015;5(2):19.
McLay RN, Klam WP, Volkert SL. Insomnia is the most commonly reported symptom and predicts other symptoms of post-traumatic stress disorder in U.S. service members returning from military deployments. Mil Med. 2010;175(10):759–62.
Sandman N, Valli K, Kronholm E, Ollila HM, Revonsuo A, Laatikainen T, et al. Nightmares: prevalence among the Finnish general adult population and war veterans during 1972-2007. Sleep. 2013;36(7):1041–50.
Taylor DJ, Pruiksma KE, Hale WJ, Kelly K, Maurer D, Peterson AL, et al. Prevalence, correlates, and predictors of insomnia in the US Army prior to deployment. Sleep. 2016;39(10):1795–806.
Babson KA, Feldner MT. Temporal relations between sleep problems and both traumatic event exposure and PTSD: a critical review of the empirical literature. J Anxiety Disord. 2010;24(1):1–15.
Klingaman EA, Brownlow JA, Boland EM, Mosti C, Gehrman PR. Prevalence, predictors and correlates of insomnia in US army soldiers. J Sleep Res. 2018;27(3):e12612.
Nadorff MR, Nadorff DK, Germain A. Nightmares: under-reported, undetected, and therefore untreated. J Clin Sleep Med. 2015;11(7):747–50.
Taylor DJ, Wilkerson AK, Pruiksma KE, Williams JM, Ruggero CJ, Hale W, et al. Reliability of the structured clinical interview for DSM-5 sleep disorders module. J Clin Sleep Med. 2018;14(03):459–64.
Taylor DJ, Wilkerson AK, Pruiksma K, Dietch JR, Wardle-Pinkston S. Structured Clinical Interview for Sleep Disorders-Revised (SCISD-R). University of Arizona website. https://insomnia.arizona.edu/SCISD. Accessed September 11, 2019.
Pruiksma KE, Wilkerson AK, Dietch JR, Wardle-Pinkston S, Dolan M, Taylor DJ. User manual for the Structured Clinical Interview for Sleep Disorders – Revised (SCISD-R). University of Arizona website https://insomnia.arizona.edu/SCISD. Accessed September 11, 2019.
Taylor DJ, Pruiksma KE. Cognitive and behavioural therapy for insomnia (CBT-I) in psychiatric populations: a systematic review. Int Rev Psychiatry. 2014;26(2):205–13.
Colvonen PJ, Straus LD, Stepnowsky C, McCarthy MJ, Goldstein LA, Norman SB. Recent advancements in treating sleep disorders in co-occurring PTSD. Cur Psychiatry Rep. 2018;20(7):48.
Qaseem A, Kansagara D, Forciea MA, Cooke M, Denberg TD. Management of chronic insomnia disorder in adults: a clinical practice guideline from the American College of Physicians. Ann Intern Med. 2016;165(2):125–33.
Wilson SJ, Nutt D, Alford C, Argyropoulos SV, Baldwin DS, Bateson AN, et al. British Association for Psychopharmacology consensus statement on evidence-based treatment of insomnia, parasomnias and circadian rhythm disorders. J Psychopharmacol. 2010;24(11):1577–601.
Riemann D, Baglioni C, Bassetti C, Bjorvatn B, Dolenc Groselj L, Ellis JG, et al. European guideline for the diagnosis and treatment of insomnia. J Sleep Res. 2017;26(6):675–700.
Morgenthaler T, Kramer M, Alessi C, et al. Practice parameters for the psychological and behavioral treatment of insomnia: an update. An American Academy of Sleep Medicine report. Sleep. 2006;29(11):1415–9.
Department of Veterans Affairs, Department of Defense. VA/DoD clinical practice guideline for the management of chronic insomnia disorder and obstructive sleep apnea. Washington, D.C.: Department of Veterans Affairs, Department of Defense; 2019.
Pruiksma KE, Fina B, Dietch JR, Dondanville KA, Williams J, Wright EC, et al. Special considerations in the adaptation of cognitive behavioral therapy for insomnia with active-duty U.S. Army personnel. Cogn Behav Pract. 2018;25(4):515–30.
Morgenthaler TI, Auerbach S, Casey KR, Kristo D, Maganti R, Ramar K, et al. Position paper for the treatment of nightmare disorder in adults: an American Academy of Sleep Medicine position paper. J Clin Sleep Med. 2018;14(06):1041–55.
Harb GC, Cook JM, Phelps AJ, Gehrman PR, Forbes D, Localio R, et al. Randomized controlled trial of imagery rehearsal for posttraumatic nightmares in combat veterans. J Clin Sleep Med. 2019;15(05):757–67.
Seyffert M, Lagisetty P, Landgraf J, Chopra V, Pfeiffer PN, Conte ML, et al. Internet-delivered cognitive behavioral therapy to treat insomnia: a systematic review and meta-analysis. PLoS One. 2016;11(2):e0149139.
Roane BM, Taylor DJ. Adolescent insomnia as a risk factor for early adult depression and substance abuse. Sleep. 2008;31(10):1351–6.
Wickwire EM, Schnyer DM, Germain A, et al. Correction to: sleep, sleep disorders, and circadian health following mild traumatic brain injury in adults: review and research agenda. J Neurotrauma. 2019;36(23):3316.
Ryan MAK, Smith TC, Smith B, Amoroso P, Boyko EJ, Gray GC, et al. Millennium cohort: enrollment begins a 21-year contribution to understanding the impact of military service. J Clin Epidemiol. 2007;60(2):181–91.
Mental Health Advisory Team 9. Mental Health Advisory Team 9 (MHAT 9) Operation Enduring Freedom (OEF) 2013 Afghanistan. Washington, DC: Office of The Surgeon General United States Army Medical Command, Office of the Command Surgeon Headquarters, US Army Central Command, and Office of the Command Surgeon US Forces Afghanistan. https://apps.dtic.mil/dtic/tr/fulltext/u2/a593777.pdf. Accessed September 11, 2019.
Funding
This project was funded in part by a private donation from Ride to Zero made to the National Center for Veterans Studies. No off-label or investigational drugs were used in this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures were reviewed and approved by the University of Utah’s Institutional Review Board.
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
ESM 1
(DOCX 30 kb)
Rights and permissions
About this article
Cite this article
Pruiksma, K.E., Slavish, D.C., Taylor, D.J. et al. Nightmares and Insomnia in the US National Guard: Mental and Physical Health Correlates. Int.J. Behav. Med. 28, 238–249 (2021). https://doi.org/10.1007/s12529-020-09889-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12529-020-09889-2