Abstract
Purpose of Review
The purpose of this paper is to review the current role of echocardiography in the evaluation of patients with low gradient severe aortic stenosis (LG severe AS).
Recent Findings
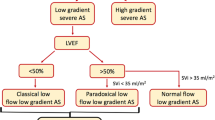
Discordant grading of AS severity, in which a small aortic valve area coexists with a small gradient, can result in diagnostic and therapeutic dilemmas. Transthoracic, transesophageal, and stress echocardiography play pivotal roles in reconciling the discordance and clarifying AS severity. Three physiologic categories of LG severe AS can be identified (classical low flow (LF) LG AS, paradoxical LF-LG AS, and normal flow LG AS), each with different prognostic and therapeutic implications. Echocardiographic measures of the severity of the valve stenosis, left ventricular function (and functional reserve), and right heart disease provide important prognostic information to assist with patient management.
Summary
A systematic comprehensive approach using echocardiography is essential in LG severe AS to understand the reason for the discordant hemodynamics, to confirm AS severity, and to guide therapeutic decision-making.









Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Eveborn GW, Schirmer H, Heggelund G, Lunde P, Rasmussen K. The evolving epidemiology of valvular aortic stenosis. The Tromsø study. Heart. 2013;99(6):396–400. https://doi.org/10.1136/heartjnl-2012-302265.
Osnabrugge RL, Mylotte D, Head SJ, Van Mieghem NM, Nkomo VT, LeReun CM, et al. Aortic stenosis in the elderly: disease prevalence and number of candidates for transcatheter aortic valve replacement: a meta-analysis and modeling study. J Am Coll Cardiol. 2013;62(11):1002–12. https://doi.org/10.1016/j.jacc.2013.05.015.
Nishimura RA, Otto CM, Bonow RO, Carabello BA, Erwin JP 3rd, Guyton RA, et al. American College of Cardiology/American Heart Association Task Force on Practice Guidelines. et al. 2014 AHA/ACC Guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. ACC/AHA Task Force Members. Circulation. 2014;129:e521–643. https://doi.org/10.1161/CIR.0000000000000031.
•• Baumgartner H, Falk V, Bax JJ, De Bonis M, Hamm C, Holm PJ, et al. ESC/EACTS guidelines for the management of valvular heart disease. ESC scientific document group. Eur heart J. 2017;38(36):2739–91. https://doi.org/10.1093/eurheartj/ehx391 An important document updating the previous 2012 ESC guidelines on the management of patients with valvular heart disease.
•• Baumgartner H, Hung J, Bermejo J, Chambers JB, Edvardsen T, Goldstein S, et al. Recommendations on the echocardiographic assessment of aortic valve stenosis: a focused update from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr. 2017;30(4):372–92. https://doi.org/10.1016/j.echo.2017.02.009 An important document updating the 2009 recommendations of the American Society of Echocardiography and the European Association of Echocardiography on the echocardiographic assessment of aortic stenosis.
Minners J, Allgeier M, Gohlke-Baerwolf C, Kienzle RP, Neumann FJ, Jander N. Inconsistencies of echocardiographic criteria for the grading of aortic valve stenosis. Eur Heart J. 2008;29:1043–8. https://doi.org/10.1093/eurheartj/ehm543.
Burwash IG, Thomas DD, Sadahiro M, Pearlman AS, Verrier ED, Thomas R, et al. Dependence of Gorlin formula and continuity equation valve areas on transvalvular volume flow rate in valvular aortic stenosis. Circulation. 1994;89(2):827–35. https://doi.org/10.1161/01.cir.89.2.827.
Burwash IG, Dickinson A, Teskey RJ, Tam JW, Chan KL. Aortic valve area discrepancy by Gorlin equation and Doppler echocardiography continuity equation: relationship to flow in patients with valvular aortic stenosis. Can J Cardiol. 2000;16(8):985–92 PMID: 10978934.
de Monchy CC, Lepage L, Boutron I, Leye M, Detaint D, Hyafil F, et al. Usefulness of the right parasternal view and non-imaging continuous-wave Doppler transducer for the evaluation of the severity of aortic stenosis in the modern area. Eur J Echocardiogr. 2009;10(3):420–4. https://doi.org/10.1093/ejechocard/jen301.
Thaden JJ, Nkomo VT, Lee KJ, Oh JK. Doppler imaging in aortic stenosis: the importance of the nonapical imaging windows to determine severity in a contemporary cohort. J Am Soc Echocardiogr. 2015;28(7):780–5. https://doi.org/10.1016/j.echo.2015.02.016.
Hahn RT, Pibarot P. Accurate measurement of left ventricular outflow tract diameter: comment on the updated recommendations for the echocardiographic assessment of aortic valve stenosis. J Am Soc Echocardiogr. 2017;30(10):1038–41. https://doi.org/10.1016/j.echo.2017.06.002.
LaBounty TM, Miyasaka R, Chetcuti S, Grossman PM, Deeb GM, Patel HJ, et al. Annulus instead of LVOT diameter improves agreement between echocardiography effective orifice area and invasive aortic valve area. JACC Cardiovasc Imaging. 2014;7:1065–6. https://doi.org/10.1016/j.jcmg.2014.03.021.
Piazza N, de Jaegere P, Schultz C, Becker AE, Serruys PW, Anderson RH. Anatomy of the aortic valvar complex and its implications for transcatheter implantation of the aortic valve. Circ Cardiovasc Interv. 2008;1:74–81. https://doi.org/10.1161/CIRCINTERVENTIONS.108.780858.
Ng AC, Delgado V, van der Kley F, Shanks M, van de Veire NR, Bertini M, et al. Comparison of aortic root dimensions and geometries before and after transcatheter aortic valve implantation by 2- and 3 dimensional transesophageal echocardiography and multislice computed tomography. Circ Cardiovasc Imaging. 2010;3:94–102. https://doi.org/10.1161/CIRCIMAGING.109.885152.
Khalique OK, Kodali SK, Paradis JM, Nazif TM, Williams MR, Einstein AJ, et al. Aortic annular sizing using a novel 3-dimensional echocardiographic method: use and comparison with cardiac computed tomography. Circ Cardiovasc Imaging. 2014;7:155–63. https://doi.org/10.1161/CIRCIMAGING.113.001153.
Kamperidis V, van Rosendael PJ, Katsanos S, van der Kley F, Regeer M, Al Amri I, et al. Low gradient severe aortic stenosis with preserved ejection fraction: reclassification of severity by fusion of Doppler and computed tomographic data. Eur Heart J. 2015;36(31):2087–96. https://doi.org/10.1093/eurheartj/ehv188.
Arangalage D, Laredo M, Ou P, Brochet E, Cimadevilla C, Enriquez-Sarano M, et al. Anatomic characterization of the aortic root in patients with bicuspid and tricuspid aortic valve stenosis: does fusion of Doppler-echocardiography and computed tomography resolve discordant severity grading? JACC Cardiovasc Imaging. 2019;12(1):210–2. https://doi.org/10.1016/j.jcmg.2018.04.013.
Clavel MA, Malouf J, Messika-Zeitoun D, Araoz PA, Michelena HI, Enriquez-Sarano M. Aortic valve area calculation in aortic stenosis by CT and Doppler echocardiography. JACC Cardiovasc Imaging. 2015;8:248–57. https://doi.org/10.1016/j.jcmg.2015.01.009.
Mehrotra P, Flynn AW, Jansen K, Tan TC, Mak G, Julien HM, et al. Differential left ventricular outflow tract remodeling and dynamics in aortic stenosis. J Am Soc Echocardiogr. 2015;28:1259–66. https://doi.org/10.1016/j.echo.2015.07.018.
Caballero L, Saura D, Oliva-Sandoval MJ, Gonzalez-Carrillo J, Espinosa MD, Garcia-Navarro M, et al. Three-dimensional morphology of the left ventricular outflow tract: impact on grading aortic stenosis severity. J Am Soc Echocardiogr. 2017;30:28–35. https://doi.org/10.1016/j.echo.2016.10.006.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015;28(1):1–39. https://doi.org/10.1016/j.echo.2014.10.003.
Stähli BE, Stadler T, Holy EW, Nguyen-Kim TDL, Hoffelner L, Erhart L, et al. Impact of stroke volume assessment by integrating multi-detector computed tomography and Doppler data on the classification of aortic stenosis. Int J Cardiol. 2017;246:80–6. https://doi.org/10.1016/j.ijcard.2017.03.112.
Dumesnil JG, Dion D, Yvorchuk K, Davies RA, Chan K. A new, simple and accurate method for determining ejection fraction by Doppler echocardiography. Can J Cardiol. 1995;11:1007–14.
Leye M, Brochet E, Lepage L, Cueff C, Boutron I, Detaint D, et al. Size adjusted left ventricular outflow tract diameter reference values: a safeguard for the evaluation of the severity of aortic stenosis. J Am Soc Echocardiogr. 2009;22:445–51. https://doi.org/10.1016/j.echo.2009.02.007.
Nakai H, Takeuchi M, Yoshitani H, Kaku K, Haruki N, Otsuji Y. Pitfalls of anatomical aortic valve area measurements using two-dimensional transoesophageal echocardiography and the potential of three-dimensional transoesophageal echocardiography. Eur J Echocardiogr. 2010;11:369–76. https://doi.org/10.1093/ejechocard/jep220.
Saito T, Muro T, Takeda H, Hyodo E, Ehara S, Nakamura Y, et al. Prognostic value of aortic valve area index in asymptomatic patients with severe aortic stenosis. Am J Cardiol. 2012;110:93–7. https://doi.org/10.1016/j.amjcard.2012.02.056.
Michelena HI, Margaryan E, Miller FA, Eleid M, Maalouf J, Suri R, et al. Inconsistent echocardiographic grading of aortic stenosis: is the left ventricular outflow tract important? Heart. 2013;99:921–31. https://doi.org/10.1136/heartjnl-2012-302881.
Jander N, Gohlke-Barwolf C, Bahlmann E, Gerdts E, Boman K, Chambers JB, et al. Indexing aortic valve area by body surface area increases the prevalence of severe aortic stenosis. Heart. 2014;100:28–33. https://doi.org/10.1136/heartjnl-2013-304443.
Minners J, Gohlke-Baerwolf C, Kaufmann BA, Bahlmann E, Gerdts E, Boman K, et al. Adjusting parameters of aortic valve stenosis severity by body size. Heart. 2014;100:1024–30. https://doi.org/10.1136/heartjnl-2013-305225.
• Tribouilloy C, Bohbot Y, Maréchaux S, Debry N, Delpierre Q, Peltier M, et al. Outcome implication of aortic valve area normalized to body size in asymptomatic aortic stenosis. Circ Cardiovasc imaging. 2016;9(11):Pii: e005121. https://doi.org/10.1161/CIRCIMAGING.116.005121 This paper shows that among AVA normalization methods, AVA/height showed better predictive performance than AVA/BSA for the occurrence of aortic valve replacement or all-cause death in asymptomatic AS.
Carabello BA. Aortic stenosis. N Engl J Med. 2002;346:677–82. https://doi.org/10.1056/NEJMcp010846.
Burwash IG. Low flow, low gradient aortic stenosis: from evaluation to treatment. Curr Opin Cardiol. 2007;22:84–91. https://doi.org/10.1097/HCO.0b013e32801466f5.
• Clavel MA, Burwash IG, Pibarot P. Cardiac imaging for assessing low-gradient severe aortic stenosis. JACC Cardiovasc imaging. 2017;10(2):185–202. https://doi.org/10.1016/j.jcmg.2017.01.002 This paper reviews the role of multimodality imaging in the diagnostic and therapeutic management of low-gradient AS.
Monin JL, Quéré JP, Monchi M, Petit H, Baleynaud S, Chauvel C, et al. Low-gradient aortic stenosis: operative risk stratification and predictors for long-term outcome: a multicenter study using dobutamine stress hemodynamics. Circulation. 2003;108:319–24. https://doi.org/10.1161/01.CIR.0000079171.43055.46.
Clavel MA, Fuchs C, Burwash IG, Mundigler G, Dumesnil JG, Baumgartner H, et al. Predictors of outcomes in low-flow, low gradient aortic stenosis: results of the multicenter TOPAS study. Circulation. 2008;118(14suppl):S234–42. https://doi.org/10.1161/CIRCULATIONAHA.107.757427.
• Pibarot P, Messika-Zeitoun D, Ben-Yehuda O, Hahn RT, Burwash IG, Van Mieghem NM, et al. Moderate aortic stenosis and heart failure with reduced ejection fraction: can imaging guide us to therapy? JACC Cardiovasc Imaging. 2019;12(1):172–84. https://doi.org/10.1016/j.jcmg.2018.10.021 This paper discusses two management strategies for patients with moderate AS and reduced LVEF. The current strategy of close clinical and imaging surveillance with AVR performed when the AS becomes severe and the provocative hypothesis that early TAVR may improve the outcome of patients with moderate AS and reduced LVEF. This hypothesis is being tested in the TAVR UNLOAD trial.
Fougeres E, Tribouilloy C, Monchi M, Petit-Eisenmann H, Baleynaud S, Pasquet A, et al. Outcomes of pseudosevere aortic stenosis under conservative treatment. Eur Heart J. 2012;33:2426–33. https://doi.org/10.1093/eurheartj/ehs176.
Blais C, Burwash IG, Mundigler G, Dumesnil JG, Loho N, Rader F, et al. Projected valve area at normal flow rate improves the assessment of stenosis severity in patients with low-flow, low-gradient aortic stenosis. The multicentre TOPAS (true or pseudo-severe aortic stenosis) study. Circulation. 2006;113:711–21. https://doi.org/10.1161/CIRCULATIONAHA.105.557678.
Clavel MA, Burwash IG, Mundigler G, Dumesnil JG, Baumgartner H. Bergler-Klein J, et al validation of conventional and simplified methods to calculate projected valve area at normal flow rate in patients with low flow, low gradient aortic stenosis: the multicenter TOPAS (true or pseudo severe aortic stenosis) study. J Am Soc Echocardiogr. 2010;23:380–6. https://doi.org/10.1016/j.echo.2010.02.002.
•• Annabi MS, Touboul E, Dahou A, Burwash IG, Bergler-Klein J, Enriquez-Sarano M, et al. Dobutamine stress echocardiography for management of low-flow, low-gradient aortic stenosis. J Am Coll Cardiol. 2018;71(5):475–85. https://doi.org/10.1016/j.jacc.2017 In classical LF-LG AS, DSE criteria of MG ≥ 40 mmHg and AVA ≤ 1.0 cm2 proposed in the guidelines to identify true-severe AS showed limited utility to predict actual stenosis severity and clinical outcome. AVAProj better distinguished true from pseudo-severe AS and was strongly associated with mortality during conservative management.
• Lancellotti P, Pellikka PA, Budts W, Chaudhry FA, Donal E, Dulgheru R, et al. The clinical use of stress echocardiography in non-ischaemic heart disease: recommendations from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J am Soc Echocardiogr. 2017;30(2):101–38. https://doi.org/10.1016/j.echo.2016.10.016 An important document providing recommendations for the clinical application of stress echocardiography in non-ischaemic heart disease.
Burwash IG, Lortie M, Pibarot P, de Kemp RA, Graf S, Mundigler G, et al. Myocardial blood flow in patients with low flow, low gradient aortic stenosis: differences between true and pseudo-severe aortic stenosis. Heart. 2008;94:1627–33. https://doi.org/10.1136/hrt.2007.135475.
Eleid MF, Sorajja P, Michelena HI, Malouf JF, Scott CG, Pellikka PA. Flow-gradient patterns in severe aortic stenosis with preserved ejection fraction: clinical characteristics and predictors of survival. Circulation. 2013;128:1781–9. https://doi.org/10.1161/CIRCULATIONAHA.113.003695.
Hachicha Z, Dumesnil JG, Bogaty P, Pibarot P. Paradoxical low flow, low gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation. 2007;115(22):2856–64. https://doi.org/10.1161/CIRCULATIONAHA.106.668681.
Adda J, Mielot C, Giorgi R, Cransac F, Zirphile X, Donal E, et al. Low-flow, low-gradient severe aortic stenosis despite normal ejection fraction is associated with severe left ventricular dysfunction as assessed by speckle tracking echocardiography: a multicenter study. Circ Cardiovasc Imaging. 2012;5(1):27–35. https://doi.org/10.1161/CIRCIMAGING.111.967554.
Lancellotti P, Magne J, Donal E, Davin L, O'Connor K, Rosca M, et al. Clinical outcome in asymptomatic severe aortic stenosis. Insights from the new proposed aortic stenosis grading classification. J Am Coll Cardiol. 2012;59(3):235–43. https://doi.org/10.1016/j.jacc.2011.08.072.
Leong DP, Pizzale S, Haroun MJ, Yazdan-Ashoori P, Ladak K, Sun YY, et al. Factors associated with low flow in aortic valve stenosis. J Am Soc Echocardiogr. 2016;29(2):158–65. https://doi.org/10.1016/j.echo.2015.10.007.
Tsang MY, Choi JO, Borlaug BA, Greason KL, Cha SS, Nishimura RA, et al. Low-flow, low-gradient severe aortic stenosis in the setting of constrictive pericarditis: clinical characteristics, echocardiographic features, and outcomes. Circ Cardiovasc Imaging. 2015;8(7):e002812. https://doi.org/10.1161/CIRCIMAGING.114.002812.
Pislaru SV, Pellikka PA. The spectrum of low-output low-gradient aortic stenosis with normal ejection fraction. Heart. 2016;102(9):665–71. https://doi.org/10.1136/heartjnl-2015-307893.
Cavalcante JL, Rijal S, Abdelkarim I, Althouse AD, Sharbaugh MS, Fridman Y, et al. Cardiac amyloidosis is prevalent in older patients with aortic stenosis and carries worse prognosis. J Cardiovasc Magn Reson. 2017;19(1):98. https://doi.org/10.1186/s12968-017-0415-x.
Dumesnil JG, Pibarot P, Carabello B. Paradoxical low flow and/or low gradient severe aortic stenosis despite preserved left ventricular ejection fraction: implications for diagnosis and treatment. Eur Heart J. 2010;31(3):281–9. https://doi.org/10.1093/eurheartj/ehp361.
Herrmann S, Stork S, Niemann M, Lange V, Strotmann JM, Frantz S, et al. Low-gradient aortic valve stenosis: myocardial fibrosis and its influence on function and outcome. J Am Coll Cardiol. 2011;58(4):402–12. https://doi.org/10.1016/j.jacc.2011.02.059.
Clavel MA, Côté N, Mathieu P, Dumesnil JG, Audet A, Pépin A, et al. Paradoxical low-flow, low-gradient aortic stenosis despite preserved left ventricular ejection fraction: new insights from weights of operatively excised aortic valves. Eur Heart J. 2014;35(38):2655–62. https://doi.org/10.1093/eurheartj/ehu152.
Clavel MA, Ennezat PV, Maréchaux S, Dumesnil JG, Capoulade R, Hachicha Z, et al. Stress echocardiography to assess stenosis severity and predict outcome in patients with paradoxical low-flow, low-gradient aortic stenosis and preserved LVEF. JACC Cardiovasc Imaging. 2013;6:175–83. https://doi.org/10.1016/j.jcmg.2012.10.015.
• Kusunose K, Yamada H, Nishio S, Torii Y, Hirata Y, Seno H, et al. Preload stress echocardiography predicts outcomes in patients with preserved ejection fraction and low gradient aortic stenosis. Circ Cardiovasc Imaging. 2017;10(10):e006690. https://doi.org/10.1161/CIRCIMAGING.117.006690 This novel study used preload stress echocardiography by leg compression to calculate AVAproj in 79 patients with LG severe AS with preserved LVEF and found that it was a strong predictor of the need for AVR.
Pibarot P, Clavel MA. Preload stress echocardiography: a new tool to confirm severity of low-gradient aortic stenosis. Circ Cardiovasc Imaging. 2017;10(10):pii: e007035. https://doi.org/10.1161/CIRCIMAGING.117.007035.
Saeed S, Senior R, Chahal NS, Lønnebakken M, Chambers JB, Bahlmann E, et al. Lower transaortic flow rate is associated with increased mortality in aortic valve stenosis. JACC Cardiovasc Imaging. 2017;10(8):912–20. https://doi.org/10.1016/j.jcmg.2017.05.008.
Côté N, Simard L, Zenses AS, Tastet L, Shen M, Clisson M, et al. Impact of vascular hemodynamics on aortic stenosis evaluation: new insights into the pathophysiology of normal flow-small aortic valve area-low gradient pattern. J Am Heart Assoc. 2017;6(7):e006276. https://doi.org/10.1161/JAHA.117.006276.
Liu D, Hu K, Liebner E, Weidemann F, Herrmann S, Ertl G, et al. Value of low-dose dobutamine stress echocardiography on defining true severe low gradient aortic stenosis in patients with preserved left ventricular ejection fraction. Int J Cardiovasc Imaging. 2018;34(12):1877–87. https://doi.org/10.1007/s10554-018-1416-z.
Chahal NS, Drakopoulou M, Gonzalez-Gonzalez AM, Manivarmane R, Khattar R, Senior R. Resting aortic valve area at normal transaortic flow rate reflects true valve area in suspected low-gradient severe aortic stenosis. JACC Cardiovasc Imaging. 2015;8(10):1133–9. https://doi.org/10.1016/j.jcmg.2015.04.021.
Connolly HM, Oh JK, Schaff HV, Roger VL, Osborn SL, Hodge DO, et al. Severe aortic stenosis with low transvalvular gradient and severe left ventricular dysfunction: result of aortic valve replacement in 52 patients. Circulation. 2000;101:1940–6. https://doi.org/10.1161/01.cir.101.16.1940.
Levy F, Laurent M, Monin JL, Maillet JM, Pasquet A, Le Tourneau T, et al. Aortic valve replacement for low-flow/low-gradient aortic stenosis operative risk stratification and long-term outcome: a European multicenter study. J Am Coll Cardiol. 2008;51:1466–72. https://doi.org/10.1016/j.jacc.2007.10.067.
Pai RG, Varadarajan P, Razzouk A. Survival benefit of aortic valve replacement in patients with severe aortic stenosis with low ejection fraction and low gradient with normal ejection fraction. Ann Thorac Surg. 2008;86:1781–9. https://doi.org/10.1016/j.athoracsur.2008.08.008.
Tribouilloy C, Lévy F, Rusinaru D, Guéret P, Petit-Eisenmann H, Baleynaud S, et al. Outcome after aortic valve replacement for low-flow/low-gradient aortic stenosis without contractile reserve on dobutamine stress echocardiography. J Am Coll Cardiol. 2009;53:1865–73. https://doi.org/10.1016/j.jacc.2009.02.02.
Clavel MA, Berthelot-Richer M, Le Ven F, Capoulade R, Dahou A, Dumesnil JG, et al. Impact of classic and paradoxical low flow on survival after aortic valve replacement for severe aortic stenosis. J Am Coll Cardiol. 2015;65:645–53. https://doi.org/10.1016/j.jacc.2014.11.047.
Clavel MA, Webb JG, Rodes-Cabau J, Masson JB, Dumont E, De Larochellière R, et al. Comparison between transcatheter and surgical prosthetic valve implantation in patients with severe aortic stenosis and reduced left ventricular ejection fraction. Circulation. 2010;122:1928–36. https://doi.org/10.1161/CIRCULATIONAHA.109.929893.
Saybolt MD, Fiorilli PN, Gertz ZM, Herrmann HC. Low-flow severe aortic stenosis: evolving role of transcatheter aortic valve replacement. Circ Cardiovasc Interv. 2017;10(8):pii: e004838. https://doi.org/10.1161/CIRCINTERVENTIONS.117.004838.
• Sato K, Sankaramangalam K, Kandregula K, Bullen JA, Kapadia SR, Krishnaswamy A, et al. Contemporary outcomes in low gradient aortic stenosis patients who underwent dobutamine stress echocardiography. J Am Heart Assoc. 2019;8(6):e011168. https://doi.org/10.1161/JAHA.118.011168 In classical LF-LG AS, contractile (flow) reserve and AS severity stratification by DSE (true-severe AS = Vmax ≥ 4m/s with AVA ≤ 1.0 cm2) were not associated with survival. AVR was associated with better survival independent of contractile (flow) reserve. While AVR was associated with better survival in patients with true-severe AS by AVAproj, this was not true in patients with pseudo-severe AS by AVAproj, suggesting AVAproj better identifies AS patients who benefit from AVR.
• Ribeiro HB, Lerakis S, Gilard M, Cavalcante JL, Makkar R, Herrmann HC, et al. Transcatheter aortic valve replacement in patients with low-flow, low-gradient aortic stenosis: the TOPAS-TAVI registry. J Am Coll Cardiol. 2018;71(12):1297–308. https://doi.org/10.1016/j.jacc.2018.01.054 This multicenter registry of 234 patients with classical LF-LG AS undergoing DSE and TAVR showed that TAVR had a low 30-day mortality rate (3.8%) and the absence of contractile reserve on DSE did not predict clinical outcome or improvement in LVEF post-TAVR.
Quere JP, Monin JL, Levy F, Petit H, Baleynaud S, Chauvel C, et al. Influence of preoperative left ventricular contractile reserve on postoperative ejection fraction in low-gradient aortic stenosis. Circulation. 2006;113:1738–44. https://doi.org/10.1161/CIRCULATIONAHA.105.568824.
Dahou A, Bartko PE, Capoulade R, Clavel MA, Mundigler G, Grondin SL, et al. Usefulness of global left ventricular longitudinal strain for risk stratification in low ejection fraction, low-gradient aortic stenosis: results from the multicenter true or pseudo-severe aortic stenosis study. Circ Cardiovasc Imaging. 2015;8(3):e002117. https://doi.org/10.1161/CIRCIMAGING.114.002117.
Dahou A, Magne J, Clavel MA, Capoulade R, Bartko PE, Bergler-Klein J, et al. Tricuspid regurgitation is associated with increased risk of mortality in patients with low-flow low-gradient aortic stenosis and reduced ejection fraction: results of the multicenter TOPAS study (true or pseudo-severe aortic stenosis). JACC Cardiovasc Interv. 2015;8(4):588–96. https://doi.org/10.1016/j.jcin.2014.08.019.
• Dahou A, Clavel MA, Capoulade R, Bartko PE, Magne J, Mundigler G, et al. Right ventricular longitudinal strain for risk stratification in low-flow, low-gradient aortic stenosis with low ejection fraction. Heart. 2016;102(7):548–54. https://doi.org/10.1136/heartjnl-2015-308309 This study shows the importance of evaluating the right heart during the assessment of patients with classical LF-LG AS. Absolute RV free wall longitudinal strain < 13% was associated with increased mortality even after adjustment for LV longitudinal strain and tricuspid regurgitation severity.
Herrmann HC, Pibarot P, Hueter I, Gertz ZM, Stewart WJ, Kapadia S, et al. Predictors of mortality and outcomes of therapy in low-flow severe aortic stenosis: a placement of aortic transcatheter valves (PARTNER) trial analysis. Circulation. 2013;127(23):2316–26. https://doi.org/10.1161/CIRCULATIONAHA.112.001290.
O'Sullivan CJ, Stortecky S, Heg D, Pilgrim T, Hosek N, Buellesfeld L, et al. Clinical outcomes of patients with low-flow, low-gradient, severe aortic stenosis and either preserved or reduced ejection fraction undergoing transcatheter aortic valve implantation. Eur Heart J. 2013;34(44):3437–50. https://doi.org/10.1093/eurheartj/eht408.
• Chetcuti SJ, Deeb GM, Popma JJ, Yakubov SJ, Grossman PM, Patel HJ, et al. Self-expanding transcatheter aortic valve replacement in patients with low-gradient aortic stenosis. JACC Cardiovasc Imaging. 2019;12(1):67–80. https://doi.org/10.1016/j.jcmg.2018.07.028 The study included patients who were not candidates for surgical AVR and were excluded from the U.S. Pivotal Extreme Risk Trial and Continued Access Study because of LG. The patients with (1) LG severe AS with preserved LVEF and (2) LG severe AS with reduced LVEF who were non-responders to DSE (peak MG < 40 mmHg) had 1-year survival and quality of life outcomes post transcatheter AVR comparable to the enrolled patients who were either DSE responders (peak MG > 40 mmHg and AVA < 1.0 cm2) or had HG severe AS. Patients with pseudo-severe AS were excluded from the study.
O'Sullivan CJ, Englberger L, Hosek N, Heg D, Cao D, Stefanini GG, et al. Clinical outcomes and revascularization strategies in patients with low-flow, low-gradient severe aortic valve stenosis according to the assigned treatment modality. JACC Cardiovasc Interv. 2015;8(5):704–17. https://doi.org/10.1016/j.jcin.2014.11.020.
van Gils L, Clavel MA, Vollema EM, Hahn RT, Spitzer E, Delgado V, et al. Prognostic implications of moderate aortic stenosis in patients with left ventricular systolic dysfunction. J Am Coll Cardiol. 2017;69(19):2383–92. https://doi.org/10.1016/j.jacc.2017.03.023.
Dayan V, Vignolo G, Magne J, Clavel MA, Mohty D, Pibarot P. Outcome and impact of aortic valve replacement in patients with preserved LVEF and low-gradient aortic stenosis. J Am Coll Cardiol. 2015;66(23):2594–603. https://doi.org/10.1016/j.jacc.2015.09.076.
Eleid MF, Sorajja P, Michelena HI, Malouf JF, Scott CG, Pellikka PA. Survival by stroke volume index in patients with low-gradient normal EF severe aortic stenosis. Heart. 2015;101(1):23–9. https://doi.org/10.1136/heartjnl-2014-306151.
Maor E, Beigel R, Grupper A, Kuperstein R, Hai I, Medvedofsky D, et al. Relation between stroke volume index to risk of death in patients with low-gradient severe aortic stenosis and preserved left ventricular function. Am J Cardiol. 2014;114(3):449–55. https://doi.org/10.1016/j.amjcard.2014.05.014.
Rusinaru D, Bohbot Y, Ringle A, Maréchaux S, Diouf M, Tribouilloy C. Impact of low stroke volume on mortality in patients with severe aortic stenosis and preserved left ventricular ejection fraction. Eur Heart J. 2018;39(21):1992–9. https://doi.org/10.1093/eurheartj/ehy123.
Jander N, Hochholzer W, Kaufmann BA, Bahlmann E, Gerdts E, Boman K, et al. Velocity ratio predicts outcomes in patients with low gradient severe aortic stenosis and preserved EF. Heart. 2014;100(24):1946–53. https://doi.org/10.1136/heartjnl-2014-305763.
Sato K, Seo Y, Ishizu T, Takeuchi M, Izumo M, Suzuki K, et al. Prognostic value of global longitudinal strain in paradoxical low-flow, low-gradient severe aortic stenosis with preserved ejection fraction. Circ J. 2014;78(11):2750–9. https://doi.org/10.1253/circj.CJ-14-0726.
• Mehrotra P, Jansen K, Tan TC, Flynn A, Hung JW. Clinical features and prognosis of patients with isolated severe aortic stenosis and valve area less than 1.0 cm2. Heart. 2018;104(3):222–9. https://doi.org/10.1136/heartjnl-2016-310729 This paper showed that the outcomes of AS patients with an AVA of 0.80–0.99 cm 2 are dependent on their flow-gradient status. Patients with NF-LG AS have a prognosis similar to moderate AS in the first 1.5 years of follow-up.
Kang DH, Jang JY, Park SJ, Kim DH, Yun SC, Song JM, et al. Watchful observation versus early aortic valve replacement for symptomatic patients with normal flow, low-gradient severe aortic stenosis. Heart. 2015;101(17):1375–81. https://doi.org/10.1136/heartjnl-2015-307528.
Yousef A, Hibbert B, Feder J, Bernick J, Russo J, MacDonald Z, et al. A novel echocardiographic hemodynamic index for predicting outcome of aortic stenosis patients following transcatheter aortic valve replacement. PLoS One. 2018;13(4):e0195641. https://doi.org/10.1371/journal.pone.0195641.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Ian G. Burwash has no conflict of interest to declare.
David Messika-Zeitoun reports grants and personal fees from Edwards Lifesciences.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Echocardiography
Rights and permissions
About this article
Cite this article
Burwash, I.G., Messika-Zeitoun, D. Low Gradient Aortic Stenosis: Role of Echocardiography. Curr Cardiovasc Imaging Rep 12, 40 (2019). https://doi.org/10.1007/s12410-019-9518-0
Published:
DOI: https://doi.org/10.1007/s12410-019-9518-0